Fig. 1
The traditional decompressive craniectomy. (a) Large right-sided fronto-temporal-parietal decompressive craniectomy is done and the bone is removed. Additional bone is removed for the subtemporal decompression. The dura is opened in a stellate fashion to allow the brain to protrude outward. (b) A patulous graft is placed (i.e. bovine pericardium) under the leaves of the stellated dura. The leaves of the dura are sutured to the graft to “tent” down the leaves against the patcth. Thus, the brain is allowed to expand out in a controlled manner. Note the prominent veins at the craniectomy edge. The dural patch is designed to prevent pinching of the veins that can exacerbate the situation by leading to venous congestion, increased cerebral edema, and cerebral infarction.
It is our thought that there is a role for the removal of tICH to prevent secondary brain injury from mass effect and cerebral edema. In this retrospective study, we discuss our experience using a minimally invasive tubular technique to reach subcortical tICH. This was done in an abbreviated manner from the Mi Space technique. These modifications were necessary because of patient acuity. These did not impact the overall ability to rapidly and safely remove the tICH.
Methods and Materials
We retrospectively reviewed our experience utilizing the modified Mi SPACE technique [15] to treat tICH. The BrainPath access system was used in all cases to reach the hematoma; it is a cylindrical tube with a fixed 13.5 mm diameter with built-in ventilation along the transition point, which allows for existing increased ICP from the bleed to be dissipated during cannulation per Ritsma et al. [15]. This along with the Myriad, a motor-driven instrument that mimics the function of suction and microscissors, are US Food and Drug Administration (FDA)-cleared devices that were obtained from NICO Corp. (Indianapolis, IN, USA). Neuronavigation was performed using the Stryker navigation system (Stryker Corp., Kalamazoo, MI, USA). Visualization was accomplished with the Zeiss Pentaro operating microscope rather than using the Video Telescopic Assisted Microscopy (VTOM) (Storz Corp., Culver City, CA, USA) described as part of the Mi SPACE technique [15].
The craniotomy was performed over the sulcus overlying the tICH. The craniotomy was typically about 3 cm in diameter. A trans-sulcal approach was utilized to reach the epicenter of the blood clot. In planning the trajectory to the clot, the pathway was taken to preserve the surrounding white matter tracks and to follow the long axis of the hemorrhage. Figure 2 depicts the principle of the trans-sulcal approach to reach a deep basal ganglia region hemorrhage. This is a coronal view. The actual trajectory is via a more anterior approach.
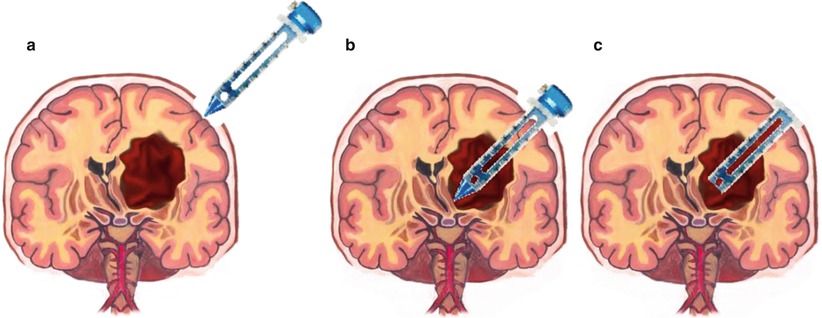
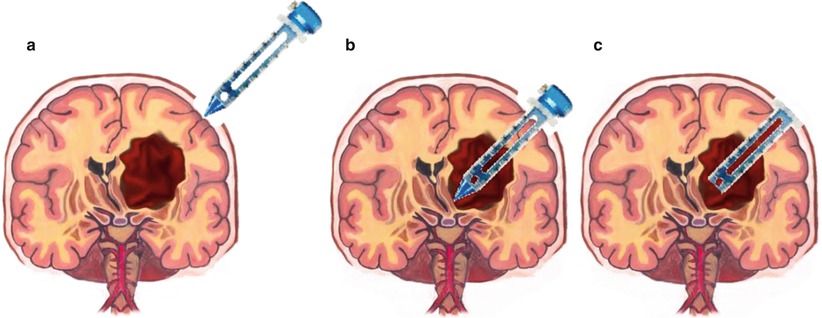
Fig. 2
Use of the trans-sulcal BrainPath approach to deep subcortical hemorrhages. Diagram depicting the trans-sulcal BrainPath approach to the deep seated hemorrhage (a). The trajectory is selected to follow the long axis of the ICH. For a basal ganglia region hemorrhage, an approach anterior to the coronal suture that angles back is effective in reaching the epicenter (b). Once the sheath is docked (c) in position, the tICH frequently delivers itself because of the surrounding increased ICP. It may also be aspirated out using the NICO Myriad aspirator that has a specially designed foot pedal that allows fine regulation of the aspiration force
Results
We identified 6 patients with 8 tICHs that were evacuated using the modified Mi SPACE technique during the time period from August 2014 to December 2014 (see Table 1). There were two patients who had two tICHs evacuated via two separate mini-craniotomies because the clots were in different lobes or different hemispheres of the brain. All of the hemorrhages were supratentorial and located as follows: right frontal-basal ganglia region = 3, right temporal = 1, left temporal = 1, bilateral ventricles = 1, right subfrontal = 1, left subfrontal = 1. The age range was 26–65. The mean age was 50. The male-to-female ratio was 2:1. Mechanisms of injury were as follows: motor vehicle related = 2, falls = 3, assault = 1. Seven out of eight hemorrhages were evacuated with the use of the Stryker neuronavigation system; one was evacuated based on anatomical landmarks because there was not sufficient time to organize the navigation scan and system as the patient had an evolving tICH with rapidly increasing ICP after a high-speed motor vehicle collision. One patient had previously undergone a decompressive craniectomy for the tICH (see Fig. 3).
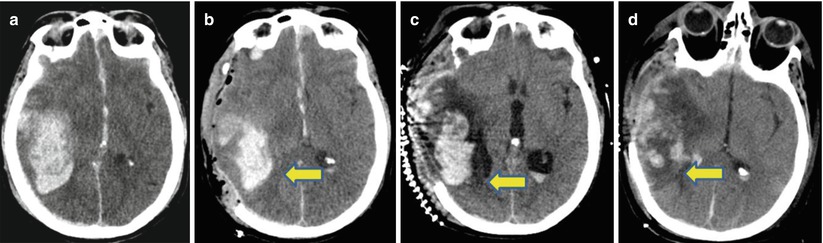
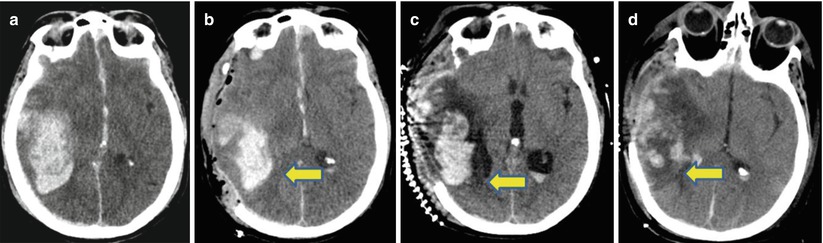
Fig. 3
Large subcortical traumatic intracerebral hemorrhage (tICH) treated first with decompressive craniectomy then with the BrainPath subcortical removal technique. Evolution of the cerebral edema around a tICH. This patient suffered a ground level fall and had a coagulopathy from alcohol. The initial CT scan demonstrated the large right temporal tICH and the patient had a declining Glascow Coma Score (GCS) of 5 (a). She underwent urgent right-sided decompressive craniectomy and her postoperative scan on postoperative day #1 is seen in (b). The arrow is pointing to the zone of edema extending into the white matter tracks. This edema increases on postoperative day 3 (arrow c) to involve the white matter tracks. Because of the increased edema and trapping of the ventricles as well as increased ICP and decline in wakefulness, the patient underwent evacuation of the tICH via the Mi SPACE technique. Her immediate postoperative CT scan is seen in (d). The zone of edema is less pronounced but still present. At 3 months, the patient made an excellent recovery and was independent with activities of daily living
Table 1
Characteristics of patients undergoing BrainPath evacuation of tICH
Patient # | Age (years) | Gender | Mechanism of injury | Coagulopathy | Location | Volume (ml) | GCS | GOS | Time to BrainPath |
|---|---|---|---|---|---|---|---|---|---|
1 | 26 | M | Assault | N | R subfrontal | 19 | 4 T | 3 | 3 days |
L subfrontal | 27 | ||||||||
2 | 41 | M | Fall | Y: renal failure | Bifrontal intraventricular | 165 | 3 T | 5 | 18 h |
3 | 54 | F | Fall | Y: ETOH liver | R frontal | 25 | 4 T | 2 | 3 days |
R temporal | 32 | ||||||||
4 | 55 | M | Peds vs. motor vehicle | N | L temporal | 38 | 11 T | 3 | 3 days |
5 | 57 | F | Fall | Y: ETOH liver | R frontal | 85 | 11 T | 5 | 3 h |
6 | 65 | M | High-speed MVC | N | Left BG | 56 | 7 T | 5 | 2 h |









