chapter 5
The Cerebral Hemispheres and Cerebellum
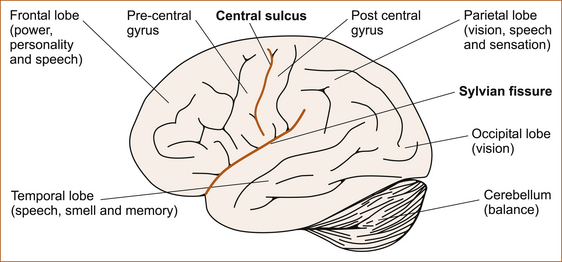
ASSESSMENT OF HIGHER COGNITIVE FUNCTION
Although subtitled ‘Assessment of higher cognitive function’, this chapter will not deal with the very complex neuropsychological testing that can be performed in patients with impairment of cognitive function. Rather, this chapter discusses a simplistic assessment of language disturbances and some very basic higher cortical functions, in particular of the parietal lobes, which can be used while taking the neurological history and examining the patient to localise the site of the pathology within the nervous system. This involves the usage of terms such as the primary pathways and secondary association areas. These terms are an aid to understanding and there is no evidence that the parietal lobes are ‘hard-wired’ in such a manner. In fact, symptoms from lesions in a part of the nervous system do not necessarily reflect the function of that part; the symptoms may arise from either a loss of certain functions or functional overactivity of the portions of the brain that remain intact [1]. The higher cortical functions represent the parallels of latitude within the cerebral hemisphere and, as already stated, ‘the pathology is ALWAYS at the level of the parallel of latitude’. More comprehensive discussions of higher cortical function can be found in the major textbooks [1–3]. Figure 5.1 gives a lateral view of the cerebral hemispheres and the cerebellum. The frontal, parietal, occipital and temporal lobes and the various functions pertaining to those lobes are shown.
THE FRONTAL LOBES
• changes in personality or behaviour
• difficulty walking in the absence of any weakness or sensory symptoms in the legs (a condition referred to as an apraxia of gait)
Contralateral weakness
The area just in front of the central sulcus, referred to as the pre-central gyrus (see Figure 5.1), is the origin of the motor fibres that innervate the muscles on the opposite side of the body. This pathway is referred to as the corticospinal tract and it crosses the midline at the level of the foramen magnum, the junction of the lower end of the brainstem and the upper end of the cervical spinal cord. Lesions affecting the pre-central gyrus will result in a contralateral hemiparesis affecting the face, arm and leg although, one limb may be weaker than the other and the face may be affected to a variable degree (partial weakness) or with hemiplegia (total weakness).
The clues that the hemiparesis is derived from a lesion in the frontal lobe are:
• conjugate eye deviation, in which the eyes look away from the side of the weakness and towards the side of the lesion due to involvement of the area of the frontal lobe that controls conjugate deviation of the eyes to the opposite side
• cortical sensory signs due to associated involvement of the parietal lobe on that side
Changes to personality or behaviour
An inability to perform acts voluntarily or to make decisions is seen in patients with pre-frontal problems and is termed abulia, reflecting pathology in the medial aspect of the frontal lobes. Abulia sometimes occurs with a subarachnoid haemorrhage (bleeding into the subarachnoid space) from vasospasm of the anterior cerebral artery related to a ruptured berry aneurysm on the anterior communicating artery (see Chapter 10, ‘Cerebrovascular disease’).
Difficulty walking
Another presentation of patients with frontal lobe pathology is apraxia of gait. The history is one of progressive difficulty walking in the absence of any weakness, sensory disturbance, ataxia or extrapyramidal dysfunction to account for the difficulty walking. It is as if the patient has forgotten how to walk. This is discussed in Chapter 12, ‘Back pain and common leg problems with or without difficulty walking’.
• a grasp reflex, where the patient involuntarily grasps an object (usually the examiner’s hand) placed in the palm of their hand
• a positive palmo-mental reflex, where the palm of the hand is stroked and there is retraction of the ipsilateral chin beneath the lips
• a pout reflex, where the patient purses the lips when a stimulus is applied to them.
THE PARIETAL LOBES
Patients with parietal lobe problems may present in a number of ways:
• speech disturbance such as fluent dysphasia and, if Wernicke’s area in the posterior temporal lobe is also affected, the patient may also present with confusion (discussed in the section ‘Disturbances of speech’ below)
• disturbances of vision in the contralateral visual field
• lost and disoriented patients who appear to be lost or disorientated even in a familiar environment
• a concerned relative brings the patient for assessment, as some patients are not even aware of any problem at all and the problem is only detected when another person observes that there is something wrong.
Speech disturbance (dysphasia) and the term RAAF (an abbreviation for the Royal Australian Air Force) best describe the features of problems in the dominant hemisphere, while the term ‘lost in space’ is the easy way to remember the characteristics of non-dominant parietal lobe problems (see Table 5.1). RAAF refers to the clinical findings seen in dominant parietal lobe problems and, in its pure form, is referred to as Gerstmann’s syndrome (for an explanation of RAAF, see ‘Gerstmann’s syndrome’ below).
TABLE 5.1
Summary of the clinical features with lesions of the dominant and non-dominant parietal lobes
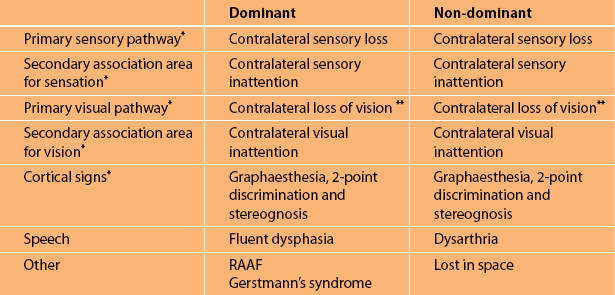
∗It can be seen that sensory and visual symptoms together with the unique parietal cortical signs are common to both the dominant and non-dominant parietal lobes. It is the speech disturbance and the parietal lobe abnormalities associated with Gerstmann’s syndrome in the dominant hemisphere and the characteristic abnormalities seen in the non-dominant hemisphere (referred to as ‘lost in space’) that differentiate between the two hemispheres.
∗∗Either loss of vision in the opposite visual field (hemianopia) or loss of vision in the upper or lower aspect of the visual field on the opposite side (quadrantanopia).
Abnormalities of vision
• Contralateral loss of vision. The optic radiation from the contralateral visual field passes through the parietal lobes to the occipital lobe (see Figure 5.1). If the ‘primary pathways’ are affected, there will be a loss of vision on the contralateral side resulting in a lower quadrantanopia if only the parietal lobe is affected, but often the optic radiation fibres in the temporal lobe are also affected and the resulting deficit is a contralateral homonymous (the visual field disturbance is identical when each eye is tested separately) hemianopia.
• Contralateral visual inattention. If the ‘primary visual pathways’ are preserved, but the so-called ‘secondary association areas’ are affected, there will be visual inattention elicited with double simultaneous stimuli. The patient is unable to appreciate the visual stimulus in one visual field, usually a moving finger applied simultaneously to both visual fields, but can if only one visual field is stimulated at a time.
Abnormalities of sensation
• Contralateral loss of sensation affecting the primary sensory modalities of vibration and proprioception, pain and temperature
• Contralateral sensory inattention where the patient cannot appreciate sensation on one side of the body when the stimulus is applied simultaneously to both sides
• Unique parietal sensory phenomena
1. Impairment of stereognosis: the patient is unable to appreciate the shape and size of an object, for example a pen or a coin, placed in the affected hand. Proprioception must not be affected, otherwise the inability to identify the object would reflect impairment of the proprioceptive pathway and not necessarily the contralateral parietal cortex as the site of abnormality.
2. Impairment of graphaesthesia: the patient is unable to identify a number drawn on the palm of the contralateral affected hand. The drawing must be greater than 4 cm in size and initially a number is drawn on the palm of the hand while the patient watches. The patient is then instructed to close their eyes and identify another number drawn on the palm. It is easier for patients to identify numbers if their palm is facing towards them and not the examiner. If light touch is severely impaired, abnormal graphaesthesia may occur and not indicate a cortical problem.
3. Impairment of 2-point discrimination: an inability to distinguish two points from one. This can be tested on any part of the body but the distance between the two points varies greatly from 1 mm on the tip of the tongue to 20–30 mm on the dorsum of the hands and feet [1]. The most useful site to test 2-point discrimination is on the fingertips where the normal distance is 3–5 mm. It is recommended to test the opposite hand (if it is normal) to determine the distance between the two points in this particular patient as this can vary from patient to patient depending on the age of the patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree