chapter 4
The Cranial Nerves and Understanding the Brainstem
THE ‘RULE OF 4’
The first section of this chapter will describe the anatomy, the techniques for examining the individual cranial nerves and the more common abnormalities encountered. The second part will discuss the ‘Rule of 4’ to aid in localising the problem within the brainstem, in particular understanding brainstem vascular syndromes [1].
THE OPTIC NERVE, CHIASM, RADIATION AND THE OCCIPITAL CORTEX
The visual pathways together, with the visual field abnormalities produced by lesions at certain sites along the pathway, are illustrated in Figure 4.1. Note that the lateral retina radiates back to the occiput on the same side via the optic nerve, chiasm and optic radiation, while the fibres from the medial retina cross at the optic chiasm and radiate to the opposite occipital lobe. The left occipital lobe receives fibres from the left lateral retina and the right medial retina (i.e. the right visual field), while the opposite is the case for the right occipital lobe.
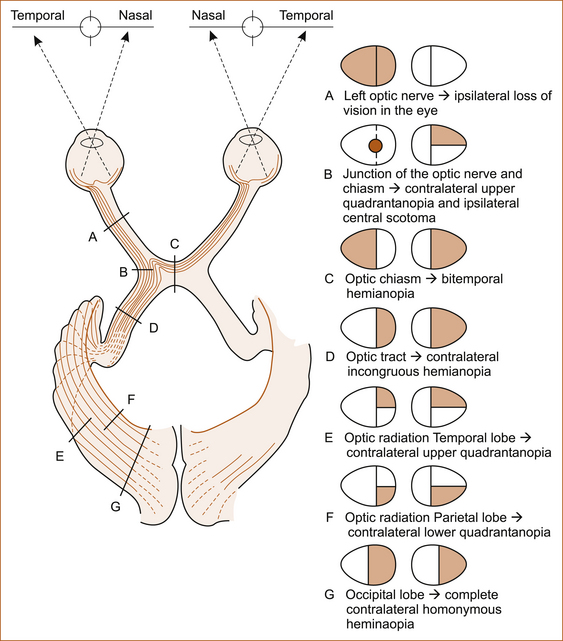
An optic nerve lesion will produce a visual field loss in one eye. The optic chiasm lies above the pituitary gland and beneath the hypothalamus and is subject to compression from pituitary and hypothalamic tumours. Lesions of the optic chiasm will produce a bitemporal field loss. An optic radiation or occipital lobe problem will result in a contralateral visual field loss, either a hemianopia (loss of one-half of the visual field) or a quadrantanopia (loss of one-quarter of the visual field).
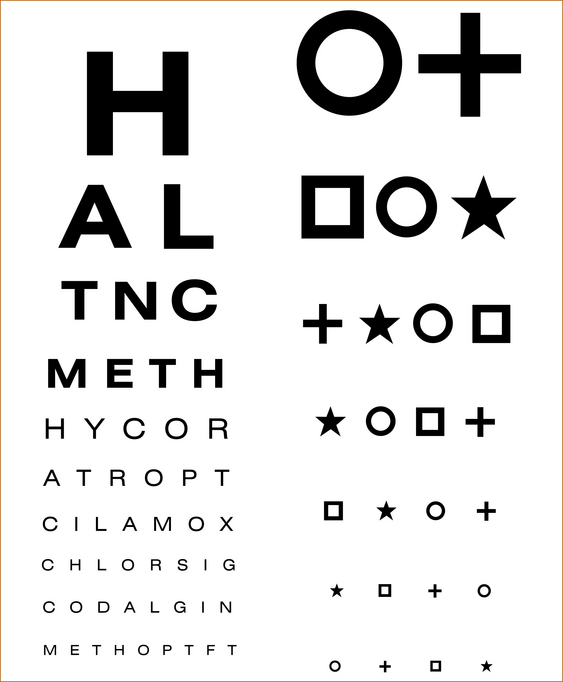
Methods of testing
The visual acuity in each eye is assessed with glasses on (corrected) and glasses off (uncorrected) using a Snellen chart (see Figure 4.2). In patients with a neurological problem it is preferable to check the acuity corrected to remove any ocular refractive error contributing to visual impairment. In the absence of glasses, impaired vision due to a refractive error can be corrected by asking the patient to look through a small hole in a piece of cardboard or paper. This will improve the vision if impairment is related to a refractive error in the eye.
COLOUR VISION
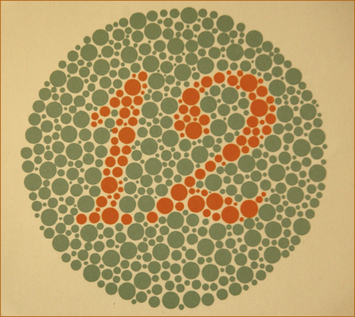
The Ishihara charts (Figure 4.3) are used to check colour vision. Colour blindness is most often hereditary, and there are two distinct patterns of impairment:
• If the patient is a protanope, colour blindness is characterised by defective perception of red and confusion of red with green or bluish green.
• If the patient is a deuteranope, color blindness is characterised by insensitivity to green.
Pathological colour blindness indicates disease in the optic nerves and can occur even in the absence of prior visual symptoms, typically with a demyelinating optic neuropathy associated with multiple sclerosis.
THE VISUAL FIELDS
Severe visual field loss: quadrantanopia, hemianopia, visual inattention
To differentiate between these two possibilities, the examiner’s finger is moved in one visual field at a time. If the visual disturbance is a loss of vision, the finger will not be seen until it reaches the midline. On the other hand, if the visual problem is inattention the single moving finger will be seen in the areas of vision where it could not initially be seen with double simultaneous stimuli. Once again, this is the principle of testing from the area of abnormality until normality is found to define the exact pattern of impairment.
CENTRAL SCOTOMA: To detect more subtle defects of the visual fields at the bedside a 4-mm red pin is used. In this test the examiner holds the pin at a distance midway between himself and the patient. The visual field of the examiner is used as a normal control. The visual fields are tested with the patient covering the left eye, for example, while the examiner covers the right eye, directly opposite the patient’s closed eye. The patient and the examiner look directly into each other’s eye and in this way the examiner can tell if the patient’s eye is moving during the test. Initially the 4-mm red pin is placed in the centre of the visual field to detect if there is a loss of central vision, a central scotoma. If there is a loss of vision in the centre, the pin is moved slowly away in each of the 4 quadrants in turn until it is visualised by the patient, establishing the size of the central scotoma. This indicates a lesion of the fovea in the eye.
ENLARGED BLIND SPOT: An enlarged blind spot occurs with a lesion of the optic discs (either optic neuritis or papilloedema). To detect an enlarged blind spot, the examiner slowly moves the 4-mm red pin out laterally from the centre at the level of the equator of the eye until the blind spot is detected. Once found, the examiner moves the pin up, down, medially and laterally until the size of the patient’s blind spot is established and compared with that of the examiner.
SUBTLE HEMIANOPIA, QUADRANTANOPIA OR BITEMPORAL HEMIANOPIA: To test the visual fields for a subtle hemianopia, quadrantanopia or bi-temporal hemianopia, the examiner moves the pin slowly from the periphery to the midline in each of the 4 quadrants asking the patient to indicate when the red pin is first noticed. If a loss is detected with this technique, the pin is then moved slowly from the area of abnormal vision to normal vision to establish the exact pattern of visual loss. Testing the visual fields individually with the 4-mm red pin will NOT detect visual inattention.
A Goldman Perimeter or Bjerum Screen is used to formally test the visual fields.
EXAMINATION OF THE OPTIC FUNDI
The patient is instructed to look straight ahead, preferably at a small dot or mark on the wall. The examiner approaches from the side at about 30–45° lateral to the midline until a retinal blood vessel is visualised and this is traced back to the optic disc (Figure 4.4). The blood vessels can be traced outwards from the optic disc to detect any abnormality. To examine the fovea (central vision), the patient looks directly at the ophthalmoscope with the intensity of the light reduced.
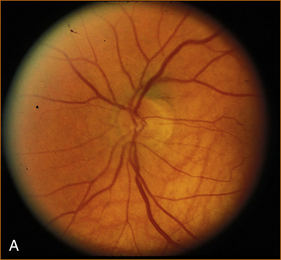
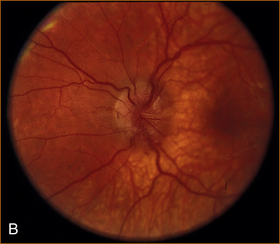
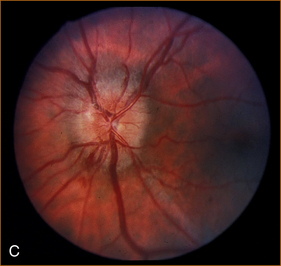
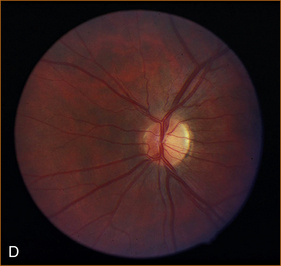
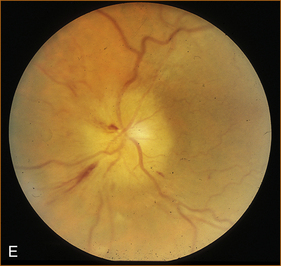
FIGURE 4.4 Normal optic disc and the more common abnormalities of the optic discs
A Normal optic disc
B Papilloedema
The visual acuity is normal unless the papilloedema is chronic, and the blind spot is enlarged. The visual fields are otherwise normal. The pupillary responses are normal.
C Acute optic neuritis
The visual acuity is markedly impaired; colour vision is abnormal if the patient can read the chart (severe visual impairment will prevent the patient from seeing the numbers on the chart). The blind spot is enlarged. The direct pupillary response is slow and there is a Marcus–Gunn pupillary phenomenon (the pupil contracts promptly when the light is shone in the normal eye and when the light is shone in the abnormal eye the pupil initially dilates and then slowly contracts). Retrobulbar neuritis is the term applied to an inflammatory optic nerve lesion within the optic nerve but not affecting the optic nerve head, the part of the optic nerve that is visualised on examination of the fundus. In this situation, the visual acuity and colour vision are impaired, the visual field defect is usually a central scotoma although it may be a diffuse, lateral, superior or inferior defect. The fundus looks normal [3].
D Long-standing optic neuritis with pallor of the optic disc
The visual acuity is reduced, colour vision is abnormal, and a Marcus–Gunn pupillary phenomenon is present (see 4C for an explanation of this abnormality).
E Anterior ischaemic optic neuropathy (AION)
AION is the most common cause of acute optic neuropathy among older persons. It can be non-arteritic (nonarteritic anterior ischaemic optic neuropathy [NAION]) or arteritic, the latter being associated with giant cell arteritis. Visual loss usually occurs suddenly, or over a few days at most, and it is usually permanent. The optic disc is pale and swollen and there are flame haemorrhages.
THE 3RD, 4TH AND 6TH CRANIAL NERVES
ANATOMY
The 3rd nerve nucleus is in the midbrain close to the midline, and the nerve exits the brainstem at the junction of the midbrain and pons just lateral to the midline (see Figure 1.6). It then crosses the subarachnoid space and, after traversing the cavernous sinus, it enters the orbit through the superior orbital fissure. The posterior communicating artery lies close to the nerve and this artery is a common site for berry aneurysm formation which can cause a 3rd nerve palsy.
The 3rd nerve supplies the following muscles:
The trochlear (4th) nerve
The 4th nerve nucleus is in the paramedian midbrain. The fibres of the 4th nerve cross the midline in the posterior aspect of the midbrain and emerge adjacent to the crus cerebri (see Figure 1.6). The 4th nerve passes through the cavernous sinus and enters the orbit via the superior orbital fissure. It supplies the superior oblique (SO) muscle that depresses the eye when it is in the adducted position and internally rotates the eye when it is looking laterally (abducted) and down. Fourth nerve palsies are commonly associated with lesions of the other oculomotor nerves due to their proximity in the cavernous sinus and orbit; an isolated 4th nerve palsy is rare but can be congenital in origin or the result of trauma.
The abducent (6th) nerve
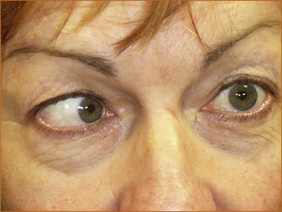
The 6th nerve nucleus lies within the pons (encircled by the 7th cranial nerve). It exits the pons laterally at the junction of the pons and medulla (see Fig. 1.6). It crosses the subarachnoid space, passes through the cavernous sinus and enters the orbit via the superior orbital fissure to supply the lateral rectus (LR) muscle. The close proximity between the 6th nerve nucleus and the 7th nerve within the pons means it is very unusual to have an isolated 6th nerve lesion with disease within the pons. Most often a 6th nerve palsy indicates a lesion directly affecting the nerve, but occasionally it can be a false localising sign due to raised intracranial pressure. A 6th nerve palsy results in an inability to abduct (move the eye laterally within the orbit) the eye fully (see Figure 4.5).
METHOD OF TESTING
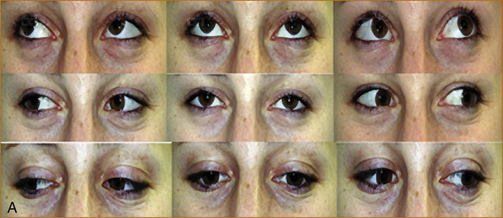
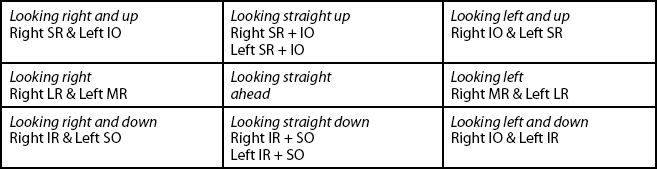
A Normal full ocular movements all directions
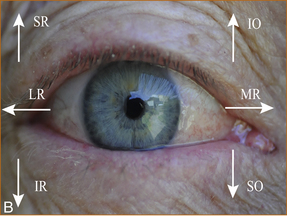
B The direction of action of the individual ocular muscles in the right eye
IO = inferior oblique, IR = inferior rectus, LR= lateral rectus, MR = medial rectus, SO = superior oblique, SR = superior rectus
Note: It is important to examine up gaze in the primary position (looking straight ahead) and also in the direction of action of each individual ocular muscle as shown.
CONTROL OF EYE MOVEMENTS, THE PUPIL AND EYELID OPENING: SYMPATHETIC AND PARASYMPATHETIC INNERVATION OF THE PUPIL AND EYELID
When a patient complains of diplopia it is important to clarify whether they actually are seeing double as some patients use the term ‘double vision’ to describe simple blurred vision. Once diplopia is confirmed, the next step is to enquire whether the diplopia is horizontal or vertical. Horizontal diplopia occurs with 6th nerve palsies and an internuclear ophthalmoplegia while vertical diplopia occurs with 3rd or 4th nerve palsies. An internuclear ophthalmoplegia occurs when the eye on the side of the brainstem where the pathology is fails to adduct and there is nystagmus in the contralateral eye as it looks outwards (refer to Figure 4.10).
Methods of examining eye movement
1. The examiner stands in front of the patient and observes the eye movements carefully.
2. The patient is requested to look up as a check for impairment of up gaze. This is a common finding in older patients but it may also represent a supranuclear gaze palsy, which refers to impairment of eye movements due to pathology above the cranial nerve nuclei that innervate the extraocular muscles.
3. The patient is asked to look to the right and then to the left while the examiner observes the eyes to see that there is a full range of horizontal eye movements.
4. The patient is instructed to look up and then down when the eye is fully abducted towards the lateral aspect of the eye and then when it is fully adducted towards the nose.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree