4
The Diagnostic Anatomy of the Brachial Plexus
Mentioning the phrase “brachial plexus anatomy” is likely to clear a medical school classroom faster than a fire drill. Sure, rout memorization of brachial plexus anatomy out of context can be very frustrating, but this does not have to be the case. For example, when one is familiar with the function of its major, terminal branches (median, ulnar, radial nerves), as well as with that of its spinal nerve input (the C5-T1 nerve roots), learning what comes in between (i.e., the brachial plexus) becomes straightforward. In fact, there is less anatomical detail to absorb than for a single upper extremity nerve.
In this chapter, I will review brachial plexus anatomy with a focus on the student’s needs—by systematically discussing the basics, not the minutia. In this chapter, only the most standard anatomy will be presented. Learning variations, despite being both common and important, is best approached after the basics have been mastered.
 The Proximal Brachial Plexus
The Proximal Brachial Plexus
Nerves and Trunks
The brachial plexus is made up of axons from five spinal nerves: C5, C6, C7, C8, and T1. Theses nerves emerge from their respective intervertebral foramina and merge to form the brachial plexus. From each spinal cord segment, multiple ventral (motor) and dorsal (sensory) rootlets exit the spinal cord, coalescing into motor and sensory roots before entering the intervertebral foramen. In the proximal intervertebral foramen, the sensory root enters its spinal ganglion. At the midportion of the intervertebral foramen, the motor and sensory roots merge to form a single spinal nerve. This merger is short-lived, however, because the spinal nerve almost immediately splits into ventral and dorsal rami after exiting the foramen. The dorsal rami of the spinal nerves run posteriorly to innervate paraspinal muscles and skin; the ventral rami form the brachial plexus.
As the spinal nerves pass through the intervertebral foramen, their enveloping dura gradually turns into epineurium. The primary site of adherence, or stabilization, of these spinal nerves is located just outside the foramen, where the inferior aspect of the nerve is attached to a depression in the transverse process. This is the only bony attachment of the brachial plexus, and serves to protect the weak intradural rootlets from traction injury that may cause traumatic avulsion. This attachment is well developed for C5, C6, and C7, but is weak or absent for C8 and T1, making these latter two nerves more susceptible to avulsion injury.
Immediately on formation, the ventral rami, which are destined for the brachial plexus, communicate with the sympathetic ganglia. This connection with the sympathetic nervous system includes both gray and white rami. More proximally, the gray ramus carries postsynaptic fibers from the sympathetic ganglia to the spinal nerve; they are destined for sweat glands and vasoconstrictors. The slightly more distal white ramus carries preganglionic information from the spinal cord to the sympathetic ganglia.
Of importance, the sympathetic fibers destined for the face via the trigeminal nerve originate from the upper thoracic spinal cord, travel through the T1 and T2 spinal nerves, and pass via the white rami into the paravertebral ganglia. These sympathetic axons pass cranially, ultimately terminating in the superior cervical ganglion. Postsynaptic sympathetic axons exit this ganglion and enter the head upon the internal carotid artery, only to be subsequently transferred to the trigeminal nerve in the cavernous sinus. Following the branches of the trigeminal nerve, these axons mediate facial sweating, pupillary dilatation, and contraction of tarsal muscles and Mueller’s muscle. Therefore, with damage to the T1 and/or T2 spinal nerves, one can have Horner’s syndrome: anhidrosis (lack of sweating), miosis (lack of pupillary dilatation), ptosis (tarsal muscle weakness), and enophthalmus (palsy of Mueller’s muscle). The presence of a Horner’s syndrome is a sign of very proximal injury to the brachial plexus.
The two upper roots, C5 and C6, merge to become the upper trunk. The lower two roots, C8 and T1, travel a bit cranially over the first rib to form the lower trunk. This leaves the C7 root to create the middle trunk. These three trunks (upper, middle, and lower), once formed, travel distal toward the clavicle (Fig. 4-1). The middle and lower trunks, as well as the C8 and T1 spinal nerves, usually do not have any branches of clinical significance. Excluding variations, the only branches from the proximal brachial plexus originate from the C5, C6, and C7 spinal nerves, as well as the upper trunk.
From the spine to the clavicle, the spinal nerves and trunks run sandwiched between the anterior and middle scalene muscles (the scalenes). The only components of the supraclavicular brachial plexus not completely covered by these two muscles are C5, C6, and a proximal segment of the upper trunk. The point where C5 and C6 merge to create the upper trunk, is called Erb’s point. C8 and T1 start below the scalenes, but initially rise cranially to be flanked by them.
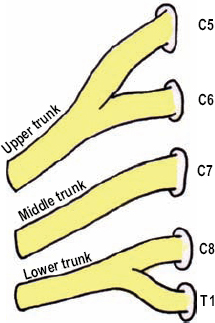
Figure 4-1 Proximal brachial plexus: spinal nerves to trunks without branches. The two upper roots, C5 and C6, merge to become the upper trunk, while the lower two roots, C8 and T1, travel a bit cranially over the first rib to form the lower trunk. That leaves only the C7 root to create the middle trunk.
 Prior to entering the brachial plexus, the spinal nerves are commonly referred to as roots. Although this nomenclature is not correct, it is commonly used. Occasionally, either C4 or T2 may contribute to the brachial plexus. When there is C4 contribution and a small T1 input, the brachial plexus is considered prefixed. In contrast, when there is minor C5 spinal nerve input with a definite T2 contribution, the plexus is called postfixed.
Prior to entering the brachial plexus, the spinal nerves are commonly referred to as roots. Although this nomenclature is not correct, it is commonly used. Occasionally, either C4 or T2 may contribute to the brachial plexus. When there is C4 contribution and a small T1 input, the brachial plexus is considered prefixed. In contrast, when there is minor C5 spinal nerve input with a definite T2 contribution, the plexus is called postfixed.
The Spinal Nerve Branches
Three nerves receive fibers from the C5 nerve root: the phrenic nerve to the diaphragm, long thoracic nerve to the serratus anterior, and the dorsal scapular nerve to the rhomboid muscles. C6 and C7 also provide fibers to the long thoracic nerve (Fig. 4-2). As mentioned, no important branches usually arise from the C8 and T1 spinal nerves.
The Phrenic Nerve
The C5 spinal nerve provides input to the phrenic nerve. The phrenic nerve is made up of motor fibers from C3, C4, and C5; hence, the phrase “C3, 4, and 5 keeps a man alive.” After being formed, the phrenic nerve runs distally on the superficial aspect of the anterior scalene muscle, laterally to medially (it is the only nerve that runs laterally to medially in the posterior triangle). Along with the anterior scalene, the phrenic nerve passes between the subclavian artery located posteriorly and the subclavian vein anteriorly, to enter the thorax. Each phrenic nerve innervates one hemidiaphragm. Depending on the amount of C5 input to the phrenic nerve, a very proximal lesion to the C5 nerve root may cause an ipsilaterally elevated and paralyzed diaphragm. This may be diagnosed by comparing the percussion of both lungs during inspiration. A radiograph or ultrasound will also confirm this type of paralysis.
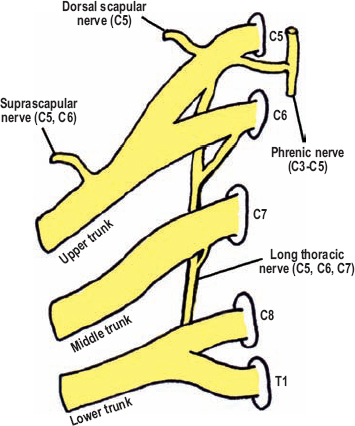
Figure 4-2 Proximal brachial plexus: spinal nerves to trunks with branches. Three branches receive a contribution from the C5 nerve root: the phrenic, long thoracic, and dorsal scapular. C6 and C7 also contribute to the long thoracic nerve. One important branch originates from the upper trunk: the suprascapular nerve.
Phrenic nerve damage may occur during open-heart surgery; it is associated with the use of ice slush to cool the heart. When this occurs postoperatively, it is thought to be a cause of respirator dependence, especially when bilateral palsies are present.
The Long Thoracic Nerve
Another branch from the proximal brachial plexus is the long thoracic nerve, having intraforaminal contributions from C5, C6, and C7. The long thoracic nerve forms dorsal to the spinal nerves, travels behind the proximal brachial plexus caudally between the anterior and middle scalenes, over the posterolateral portion of the first rib, eventually innervating the serratus anterior muscle. The serratus anterior pulls the scapula away from the midline and forward around the thorax (scapular abduction). It also rotates the scapular upward. Most importantly, however, this muscle fixes and stabilizes the scapula so that muscles originating from it can function properly.
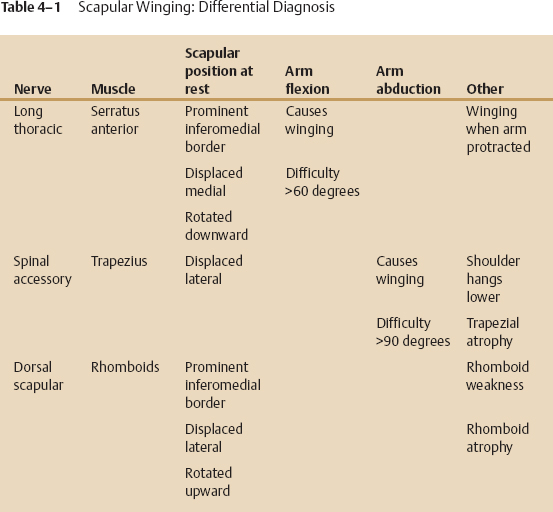
Injury to the long thoracic nerve causes winging of the scapula. At rest, there may be prominence of the scapula’s inferomedial edge, with medial displacement and downward rotation. Winging is classically worsened when the patient pushes forward against resistance with the elbow fully extended and the shoulder girdle protracted forward (anterior) (Fig. 4-3). This latter finding is the hallmark of a long thoracic palsy.
To test this muscle, instruct the patient to reach for a point on the wall in front of him or her, and then apply resistance at the hand or wrist while stabilizing the thorax with the other hand. A common mistake is to not have the patient displace the shoulder girdle forward enough because without doing so, scapular winging from trapezius or rhomboid weakness may be misdiagnosed as a long thoracic palsy. Of note, weakness of any of these three muscles can cause winging when the arm is pushed against resistance across the chest with the arm bent.
 The C7 spinal nerve variably provides a branch to the long thoracic nerve. Although weakness itself of the serratus anterior often causes a dull ache in the shoulder region, if the pain is acute and severe, then one should consider acute brachial neuritis as the etiology.
The C7 spinal nerve variably provides a branch to the long thoracic nerve. Although weakness itself of the serratus anterior often causes a dull ache in the shoulder region, if the pain is acute and severe, then one should consider acute brachial neuritis as the etiology.
The Dorsal Scapular Nerve
Another branch from the C5 spinal root is the dorsal scapular nerve. This nerve innervates both the major and minor rhomboid muscles (the rhomboids). The rhomboids connect the medial edge of the scapula to the spinal column. When contracted, the rhomboids pull the scapula toward the midline (scapular adduction) and superiorly (scapular downward rotation)–the opposite direction to that of the serratus anterior muscle. The dorsal scapular nerve passes dorsally perforating the middle scalene. It then travels along the undersurface of the levator scapulae down to the rhomboids. With chronic denervation of the rhomboids, interscapular wasting is evident. With rhomboid weakness, there may be mild scapular winging at rest, especially at the inferomedial edge. The scapula may also be laterally displaced and upwardly rotated. To test the rhomboids have the patient place the palm on his or her lower back facing outward. Instruct the patient to push the palm away from the lower back as you apply resistance to the hand as well as to the arm (apply resistance in an anterolateral direction around the thorax) (Fig. 4-4). Observe and palpate the rhomboids during this maneuver. Concurrent damage to the proximal brachial plexus is often present; therefore, the forearm may need to be supported. An alternate method to examine the rhomboids is to have the patient bring the shoulders and scapulae together posteriorly. In this position, the contracted rhomboids can be palpated between the medial aspects of the scapulae.

Figure 4-3 Serratus anterior (C5, C6, C7) assessment: Instruct the patient to reach for a point on the wall in front of him or her, and then apply resistance at the wrist while stabilizing the thorax with your other hand. A common mistake is to not have the patient displace the shoulder girdle forward enough (i.e., enough shoulder protraction) because without doing so, scapular winging from trapezius or rhomboid weakness may be misdiagnosed as a long thoracic palsy.
 The dorsal scapular nerve can provide partial innervation to the levator scapula as it passes underneath this muscle.
The dorsal scapular nerve can provide partial innervation to the levator scapula as it passes underneath this muscle.
The Truncal Branches
There is only one branch of significance from the brachial plexus trunks: the suprascapular nerve. This nerve originates from the distal, superior aspect of the upper trunk, just above the clavicle. In summary, therefore, all the proximal brachial plexus branches come from the C5, C6, and C7 spinal nerves, or the upper trunk, with C5 input being present in all of them (Fig. 4-2).

Figure 4-4 Major and minor rhomboids (C5) assessment: Have the patient place the palm facing outward on his or her lower back. Instruct the patient to push the palm away from the lower back as you apply resistance to the hand as well as to the arm (the arm is pushed anterior and lateral around the thorax). Instruct the patient to lead with the hand, not the elbow.
The Suprascapular Nerve
The suprascapular nerve (C5, C6) descends posteriorly and distally along the superior portion of the upper trunk, then between the inferior belly of the omohyoid and the trapezius muscle toward the suprascapular notch. The suprascapular nerve’s convergence with the omohyoid muscle at the scapula confirms its identity. The suprascapular artery and vein traverse the brachial plexus just superior and deep to the clavicle, joining the suprascapular nerve as it approaches the suprascapular notch. The suprascapular nerve passes through the notch and under the superior scapular ligament; the artery and vein pass over this ligament (Fig. 4-5). The nerve and vessels join again as they pass around the lateral edge of the scapular spine through the spinoglenoid fossa. Here, all components of the neurovascular bundle pass under the inferior scapular ligament. The suprascapular nerve innervates the supraspinatus and infraspinatus muscles. The supraspinatus attaches to the superior aspect of the humeral head and mediates the initial 20 to 30 degrees of arm abduction. The infraspinatus attaches to the posterior aspect of the humeral head and is the primary external rotator of the arm. Test the supraspinatus muscle by having the patient abduct a straight arm from his or her side against resistance (Fig. 4-6). To test the infraspinatus muscle, instruct the patient to flex the forearm to 90 degrees. Then stabilize the elbow against the side of the patient, and ask him or her to rotate the arm externally against resistance, like a tennis swing (Fig. 4-7). Contraction of these two muscles can be observed and palpated during testing. With chronic denervation, atrophy above (supraspinatus) or below (infraspinatus) the scapular spine is readily appreciated.
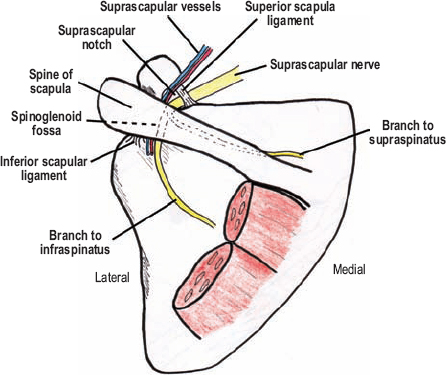
Figure 4-5 Suprascapular anatomy. The suprascapular nerve passes under the superior scapular ligament; the artery and vein pass over this ligament. This neurovascular bundle then passes around the lateral edge of the scapular spine through the spinoglenoid fossa. Here both the vessels and nerve pass under the inferior scapular ligament.
Acute suprascapular palsies are usually secondary to trauma (abrupt shoulder distraction or scapular fractures); therefore, for gradual-onset palsies one should consider ganglion cysts or idiopathic entrapment at the suprascapular notch. If there is a great deal of shoulder pain that improves as muscle weakness appears, then acute brachial neuritis is likely. For entrapment cases, narrowing or callus involving the suprascapular notch may be seen on properly directed radiographs.

Figure 4-6 Supraspinatus (C5, C6) assessment: Test the supraspinatus muscle by having the patient abduct a straight arm from his or her side against resistance.

Figure 4-7 Infraspinatus (C5, C6) assessment: Test the infraspinatus muscle by instructing the patient to flex the forearm to 90 degrees. Then stabilize the elbow against the side of the patient, and ask him or her to rotate the arm externally against resistance, like a tennis swing. (The teres minor also externally rotates the arm.)
 The small, often forgotten, subclavius nerve to the subclavius muscle also originates from the upper trunk. This muscle, however, cannot be tested clinically or electrophysiologically; therefore, it is unimportant.
The small, often forgotten, subclavius nerve to the subclavius muscle also originates from the upper trunk. This muscle, however, cannot be tested clinically or electrophysiologically; therefore, it is unimportant.
 The Distal Brachial Plexus
The Distal Brachial Plexus
Major Branches from the Cords
The distal portion of the brachial plexus is composed of cords, which are named according to their relationship to the axillary artery deep to the pectoralis minor muscle (lateral, medial, posterior)(Fig. 4-8). The cords are intimately associated with the axillary artery and vein in this region. As the brachial plexus cords pass further distal to the pectoralis minor, their anatomical relationship to this artery changes-they are no longer lateral, medial, and posterior.
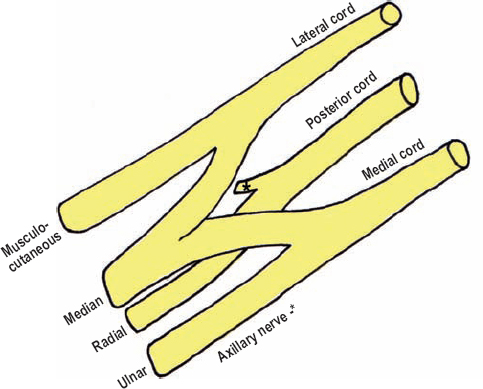
Figure 4-8 Distal brachial plexus cords and terminal branches. The distal portion of the brachial plexus is composed of cords, which are named according to their relationship to the axillary artery deep to the pectoralis minor (lateral, medial, posterior).
The major, terminal branches of the brachial plexus have been discussed in previous chapters (median, ulnar, and radial nerves). The median nerve is not a continuation of any cord per se, but is created from a lateral contribution from the lateral cord (mostly sensory), as well as a medial contribution from the medial cord (mostly motor to hand intrinsics). Both of these contributions pass superficial to the axillary artery and form the median nerve on its anterior surface. After giving these contributions, the remaining portion of the medial cord continues into the arm as the ulnar nerve; the remaining portion of the lateral cord continues as the musculocutaneous nerve. This anatomical arrangement resembles an M over the axillary artery, with the center leg being the median nerve, the lateral leg the musculocutaneous nerve, and the medial leg the ulnar nerve. The posterior cord runs deep to the axillary artery. In the axilla, the posterior cord remains deep between the axillary artery and vein, with the axillary nerve branching off, prior to it continuing as the radial nerve into the arm. The musculocutaneous and axillary nerves will be discussed further at this point.
The Musculocutaneous Nerve
The musculocutaneous nerve (C5, C6) is the distal continuation of the lateral cord containing fibers from the upper trunk (Fig. 4-9). In the axilla, the musculocutaneous nerve travels distal, and somewhat lateral, to pierce the coracobrachialis muscle, which it innervates. The coracobrachialis muscle assists the anterior deltoid in flexing the arm (forward in front of the body). It also stabilizes the humerus during forearm flexion. The coracobrachialis cannot be isolated or palpated, and therefore, is not examined clinically. After passing through, and then deep to this muscle, the musculocutaneous nerve continues on the superficial surface of the brachialis muscle deep to the lateral border of the biceps brachii. These two muscles are also innervated via multiple branches off the musculocutaneous nerve. Distally, the musculocutaneous nerve enters the antecubital fossa where it pierces the superficial fascia just lateral to the biceps tendon, entering the subcutaneous space as the lateral antebrachial cutaneous nerve. The territory of this sensory nerve includes, as the name implies, the lateral half of the forearm (Fig. 4-10). The lateral antebrachial cutaneous nerve has an anterior and posterior division. The biceps brachii, with the assistance of the brachialis and brachioradialis, flexes the forearm. The biceps brachii is also a strong supinator of the forearm when the elbow is flexed. To test the biceps brachii and brachialis, have the patient flex a fully supinated arm against resistance (Fig. 4-11). By testing the arm in full supination, the contribution from the brachioradialis is minimized.
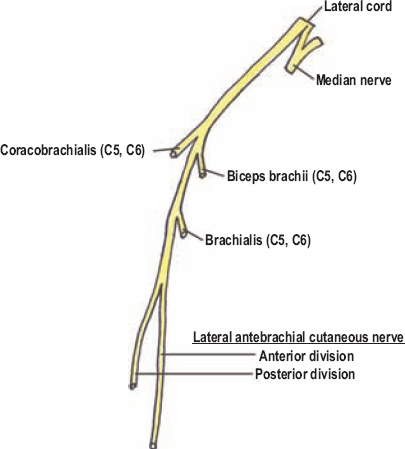
Figure 4-9 Motor innervation of the musculocutaneous nerve.
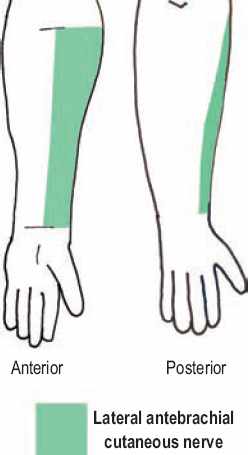
Figure 4-10 Musculocutaneous nerve sensory territory. The territory of the lateral antebrachial cutaneous nerve includes, as the name implies, the lateral one half of the forearm.

Figure 4-11 Biceps brachii (C5, C6) assessment: To test the biceps brachii and brachialis, have the patient flex a fully supinated arm against resistance. By testing the arm in full supination, contribution from the brachioradialis (radial nerve) is minimized.
Isolated musculocutaneous palsies are rare, but can occur occasionally following trauma or shoulder dislocation. These patients would present with numbness in their anterolateral forearm and with forearm flexion weakness. These findings need to be clinically differentiated from a biceps tendon rupture, as well as from a C6 radiculopathy. Following tendon rupture, the biceps still contracts and can be felt rolling up the arm. A C6 radiculopathy can also be differentiated not only because of the radicular pain, but also because of possible weakness in other, non-musculocutaneous innervated, C6 muscles, including the brachioradialis and latissimus dorsi. Furthermore, C6 radiculopathies usually cause numbness confined to the thumb and index finger, whereas the sensory coverage of the lateral antebrachial cutaneous nerve stops at the wrist. Focal damage to the lateral antebrachial cutaneous nerve can be from venipuncture in the antecubital fossa.
The Axillary Nerve
The axillary nerve (C5, C6) arises from the posterior cord deep to the axillary artery. A branch off the axillary artery, the posterior humeral circumflex artery, joins the axillary nerve, passing inferiorly and medially to it. This neurovascular bundle passes briefly upon the subscapularis muscle toward the surgical neck of the humerus. It then passes through the quadrangular, or quadrilateral, space, which is bordered superiorly by the teres minor, inferiorly by the teres major, laterally by the neck of the humerus, and medially by the long head of the triceps (Fig. 4-12). The axillary nerve is relatively fixed at the quadrangular space, and analogous to the suprascapular nerve in the suprascapular notch, is especially vulnerable to stretch injury when blunt or traction forces are applied to the brachial plexus. Immediately after passing through the quadrangular space, the axillary nerve divides into anterior and posterior divisions. The anterior division curves anteriorly and somewhat superiorly under the deltoid muscle, which it innervates. The posterior division gives an immediate branch to the teres minor after passing through the quadrangular space (Fig. 4-13). The posterior division then pierces the brachial fascia distal and posterior to the deltoid’s insertion into the humerus to become cutaneous. This cutaneous portion of the axillary nerve carries sensation from the upper lateral arm (Fig. 4-14); it is called the upper lateral brachial cutaneous nerve. The axillary nerve also carries sensory fibers from the shoulder joint.
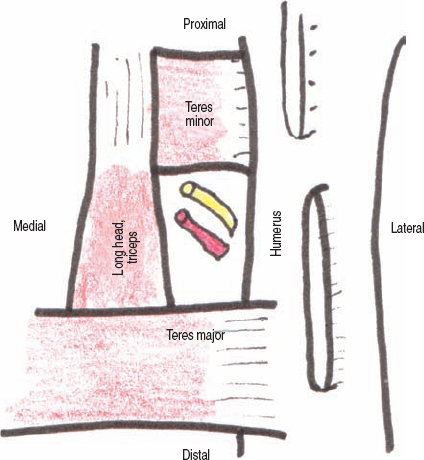
Figure 4-12 Borders of the quadrangular space, ventral perspective. The axillary nerve passes through the quadrangular space, which is bordered superiorly by the teres minor, inferiorly by the teres major, laterally by the neckofthehumerus, and medially by the long head of the triceps.
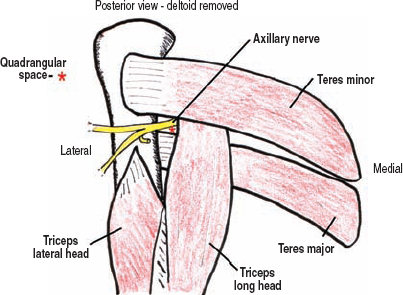
Figure 4-13 Axillary nerve anatomy, posterior view with deltoid removed. Immediately after passing through the quadrangular space, the axillary nerve divides into an anterior and posterior division. The anterior division curves anteriorly and somewhat superiorly under the deltoid muscle, which it innervates. The posterior division gives an immediate branch to the teres minor after passing through the quadrangular space, and then becomes subcutaneous by piercing the brachial fascia.
The teres minor assists the infraspinatus in externally rotating the arm. It also weakly assists the teres major in adducting a straight arm. It is not possible to test the teres minor in complete isolation, but one may observe and palpate its contraction if the patient is thin. The deltoid is the prime abductor of the arm, especially between 30 and 90 degrees. The initial 30 degrees of abduction is primarily controlled by the supraspinatus, whereas abduction above 90 degrees has an important trapezial component, which rotates the shoulder girdle upward. Test the deltoid by having the patient abduct the arm against resistance (Fig. 4-15). The deltoid has three separate heads: the anterior, lateral, and posterior. Abducting the arm to the side and slightly in front of the body tests the anterior and lateral heads of the deltoid. To assess the posterior head, have the patient place a straightened arm almost 90 degrees abducted, and then ask the patient to move the arm posteriorly and superiorly against resistance (Fig. 4-16). The absence of posterior deltoid contraction can help confirm an axillary palsy, especially in those patients with a powerful supraspinatus muscle that alone can abduct the arm to 90 degrees. Arm flexion (in front of the body) is mediated by the anterior deltoid. Although the initial 60 degrees of arm flexion is mostly anterior deltoid, the serratus anterior assists the deltoid during flexion above 60 degrees.
The axillary nerve is usually injured in isolation by shoulder trauma, including shoulder dislocations or humeral fractures. For patients with suspected axillary neuropathy following shoulder trauma, one should always exclude partial damage to the posterior division of the brachial plexus as an alternate diagnosis. By examining the latissimus dorsi (the thoracodorsal nerve), as well as all the muscles innervated by the radial nerve, posterior cord involvement can be excluded. The axillary nerve may be compressed at the quadrangular space, which is known as the quadrangular space syndrome. The etiology of this entrapment is uncertain.

Figure 4-14 Axillary nerve sensory territory. The posterior division of the axillary nerve ends by piercing the brachial fascia distal and posterior to the deltoid’s insertion into the humerus. This cutaneous extension of the axillary nerve carries sensation from the upper lateral arm, and is called the upper lateral brachial cutaneous nerve.

Figure 4-15 Deltoid (C5,C6) assessment: Testthe deltoid by having the patient abduct the arm against resistance. The deltoid has three separate heads: anterior, lateral, and posterior. Abducting the arm to the side, and slightly in front of the body tests the anterior and lateral heads of the deltoid. The deltoid controls abduction between 30 and 90 degrees.
 Sensory loss on the upper lateral arm is usually only temporary, even with complete axillary palsies. This is because following injury the descending cervical plexus branches to supply sensation to this area. Even with complete deltoid paralysis, the patient may use other upper-extremity muscles to abduct the arm, thereby mimicking deltoid function. As mentioned, a well-developed supraspinatus can achieve more than 30 degrees of arm abduction. The external rotators of the arm may also weakly abduct the arm. In addition, both the coracobrachialis and long head of the triceps, which connect the scapula to the humerus and olecranon, respectively, can substitute for deltoid function by lifting the arm. Therefore, palpating the deltoid during muscle testing is important.
Sensory loss on the upper lateral arm is usually only temporary, even with complete axillary palsies. This is because following injury the descending cervical plexus branches to supply sensation to this area. Even with complete deltoid paralysis, the patient may use other upper-extremity muscles to abduct the arm, thereby mimicking deltoid function. As mentioned, a well-developed supraspinatus can achieve more than 30 degrees of arm abduction. The external rotators of the arm may also weakly abduct the arm. In addition, both the coracobrachialis and long head of the triceps, which connect the scapula to the humerus and olecranon, respectively, can substitute for deltoid function by lifting the arm. Therefore, palpating the deltoid during muscle testing is important.

Figure 4-16 Posterior deltoid (C5, C6) assessment: To assess the posterior deltoid, have the patient place a straightened arm almost 90 degrees abducted, and then ask him or her to move the arm posteriorly and superiorly against resistance. Contraction of the posterior head can be observed and palpated.
 Distal Brachial Plexus
Distal Brachial Plexus
Minor Branches from the Cords
Aside from the major terminal branches described in the previous section (musculocutaneous and axillary nerves), each cord has other smaller branches (Fig. 4-17). The lateral cord gives one minor branch, the lateral pectoral nerve to the pectoralis major. The medial cord gives three minor branches, a medial pectoral nerve to both the pectoralis minor and major, and two cutaneous branches: the medial brachial and antebrachial cutaneous nerves. The posterior cord also has three small branches: It has two subscapular nerves, the upper subscapular to the subscapularis and the lower subscapular to the subscapularis and teres major, as well as a third branch called the thoracodorsal nerve, which innervates the latissimus dorsi. Damage to any of these nerves helps localize a lesion to the cord level.
The Lateral Cord
The lateral pectoral nerve (C5, C6) branches from the proximal lateral cord, travels over the brachial plexus and axillary artery, pierces the clavipectoral fascia (which separates the pectoralis major from all other deep structures, including the pectoralis minor), and then fans out to innervate the pectoralis major from below. The lateral pectoral nerve concentrates its innervation upon the clavicular head of the pectoralis major. When this branch passes over the plexus, there is a reliable connection, or temporary merger, with the medial pectoral nerve, which as the name implies, comes from the medial cord. The pectoralis major is a strong adductor and internal rotator of the arm. To test the clavicular head of the pectoralis major, and therefore the lateral pectoral nerve, have the patient abduct the arm 90 degrees with the forearm flexed and palm facing forward (Fig. 4-18). Then, against resistance at the medial elbow, have the patient swing his or her arm toward mid-line. The lateral pectoral nerve is the only minor branch from the lateral cord.
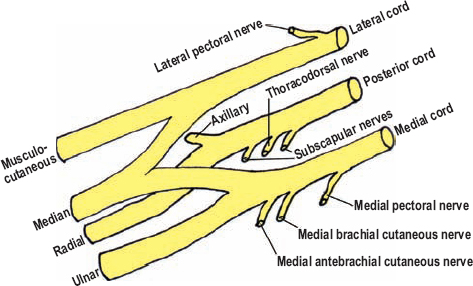
Figure 4-17 Distal brachial plexus and branches. Aside from the major terminal branches, each cord has other smaller branches: The lateral cord has one, and both the medial and posterior cords have three.

Figure 4-18 Clavicular head of the pectoralis major (C5, C6) assessment: To test the clavicular head of the pectoralis major, start by having the patient abduct the arm 90 degrees with the forearm in flexion and palm facing forward. Then, against resistance atthe medial elbow, instructthe patient to swing his or her arm anterior toward the midline (across the chest).
The Medial Cord
There are three minor branches from the medial trunk: the more proximal medial pectoral nerve, and the more distal medial brachial and antebrachial cutaneous nerves. The medial pectoral nerve (C6-T1) innervates the pectoralis minor, which it passes through, and then pierces the clavipectoral fascia to innervate the sternal head of the pectoralis major. As mentioned, this nerve almost always communicates with the lateral pectoral nerve. To test the sternal head of the pectoralis major, the patient should begin with the forearm flexed 90 degrees and the arm abducted approximately 30 degrees. Instruct the patient to adduct the arm against resistance placed at the medial elbow (Fig. 4-19). The pectoralis minor cannot be adequately isolated from the pectoralis major, and is therefore not assessed clinically.
Just prior to formation of the ulnar nerve, the medial cord gives off two branches: the medial brachial cutaneous nerve and the medial antebrachial cutaneous nerve. Both of these nerves were discussed in the ulnar nerve chapter because they are more readily understood in that context. In summary, sensory loss on the medial one half of the arm (medial brachial cutaneous) and forearm (medial antebrachial cutaneous) should be used to confirm involvement of the medial cord.

Figure 4-19 Sternal head of the pectoralis major (C6-T1) assessment: To test the sternal head of the pectoralis major, the patient begins with the forearm flexed 90 degrees and the arm abducted approximately 30 degrees. Then instruct the patient to adduct the arm against resistance applied to the medial elbow.
 The medial arm is part of the T2 dermatome. Therefore, the medial antebrachial cutaneous nerve returns sensory impulses through the medial cord and lower trunk to the T2 spinal nerve. The presence of T2 axons in the brachial plexus has been excluded thus far from discussion for simplicity.
The medial arm is part of the T2 dermatome. Therefore, the medial antebrachial cutaneous nerve returns sensory impulses through the medial cord and lower trunk to the T2 spinal nerve. The presence of T2 axons in the brachial plexus has been excluded thus far from discussion for simplicity.
Posterior Cord
Like the medial cord, the posterior cord also has three minor branches. The muscles they innervate are easy to remember because they are the same three muscles upon which the radial nerve (terminal continuation of the posterior cord) passes superficial to when exiting the axilla: the subscapularis, latissimus dorsi, and teres major. All three of these branches hang down like icicles from the posterior cord over the surface of the subscapularis muscle.
The first and last minor branches from the posterior cord are aptly named the upper and lower subscapular nerves (C5, C6). The upper subscapular nerve is not very long and enters the subscapularis muscle to innervate it. The subscapularis muscle, along with the teres major (and latissimus dorsi and pectoralis major), internally rotates the arm. The subscapularis muscle cannot be completely isolated, but one can test internal arm rotation as a composite test (Fig. 4-20). The lower subscapular nerve innervates the lower half of the subscapularis muscle, as well as the teres major. The teres major, along with the latissimus dorsi and pectoralis major, are the main arm adductors. To test the teres major, begin with a straightened arm abducted horizontally with the palm down. Instruct the patient to adduct the extended arm against resistance while you inspect the teres major (Fig. 4-21). The third branch from the posterior cord is the thoracodorsal nerve, which arises between the upper and lower subscapular nerves. The thoracodorsal nerve innervates the latissimus dorsi muscle. To assess the latissimus dorsi, the patient should adduct the arm when the forearm is flexed 90 degrees with the palm facing forward (Fig. 4-22). In summary, all of the branches from the posterior cord act to adduct and internally rotate the arm, a point worth remembering.

Figure 4-20 Subscapularis (C5, C6) assessment: Have the patient internally rotate his or her arm while the forearm is flexed. Stabilize the elbow at the patient’s flank.

Figure 4-21 Teres major (C5, C6) assessment: To test the teres major, begin with the straightened arm abducted horizontally with the palm down. Instruct the patient to adduct the arm against resistance while you inspect the teres major.
 Brachial Plexus Divisions and the Complete Picture
Brachial Plexus Divisions and the Complete Picture
Previous chapters reviewed the median, ulnar, and radial nerves. This section discussed the remaining branches of the brachial plexus, including the musculocutaneous and axillary nerves, as well as several more minor branches. The hard part is over; connecting the proximal and distal ends of the plexus is easy.

Figure 4-22 Latissimus dorsi (C6-C8) assessment: To assess the latissimus dorsi, have the patient adduct the arm when the forearm is flexed 90 degrees with the palm facing forward.
The brachial plexus divisions connect the trunks to the cords (Fig. 4-23). There are no distinct branches from the divisions. Each of the three trunks has both an anterior and posterior division. All three posterior divisions merge to create the posterior cord. The anterior divisions from the upper and middle trunks create the lateral cord; only the anterior division of the lower trunk forms the medial cord. The posterior cord receives the largest number of divisions (three); this can be remembered by the fact that the posterior cord subsequently yields the largest terminal branch of the plexus, the radial nerve. The medial cord receives the anterior division of the lower trunk, which is made up of the C8 and T1 spinal nerves. Knowing that the ulnar nerve is predominantly C8 and T1, it makes sense that the medial cord, which continues distally as the ulnar nerve, originates from the anterior division of the lower trunk (Fig. 4-24).
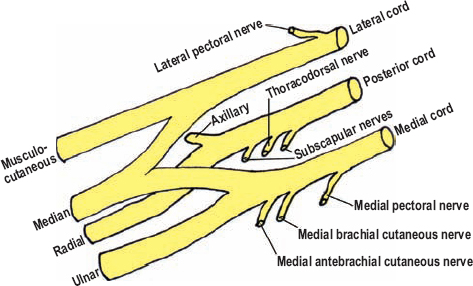
Figure 4-23 Brachial plexus divisions. The posterior cord is made up of all three posterior divisions, the lateral cord from the anterior divisions of the upper and middle trunks, and the medial cord from the lower trunk’s anterior division.
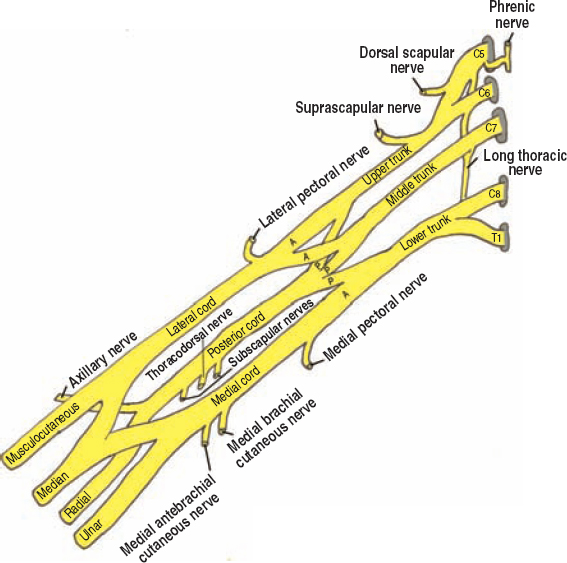
Figure 4-24 The complete brachial plexus and its branches.
 The ulnar nerve can also have a C7 contribution. In this case, a more distal, accessory communication from the lateral cord to the ulnar nerve is usual present, which carries the C7 input.
The ulnar nerve can also have a C7 contribution. In this case, a more distal, accessory communication from the lateral cord to the ulnar nerve is usual present, which carries the C7 input.
 Regional Anatomical Relationships
Regional Anatomical Relationships
The brachial plexus runs in a linear path from the intervertebral foramina, under the clavicle, through the axilla, finally ending in the medial arm as terminal branches. It is intimately associated with numerous muscular, arterial, and venous structures as it passes through these regions.
The proximal brachial plexus is located within the posterior triangle of the neck. The posterior triangle of the neck is defined by the sternocleidomastoid muscle anteriorly, the trapezius posteriorly, and by the clavicle inferiorly. The posterior belly of the omohyoid traverses the lower aspect of the posterior triangle, converging with the suprascapular nerve at the scapula.
The brachial plexus runs through the interscalene triangle, which is bordered by the anterior scalene, the middle scalene, and the first rib. The apex of the interscalene triangle is located in the posterior triangle of the neck. The anterior and middle scalenes originate from the anterior and posterior tubercles, respectively, of the cervical transverse processes. These muscles run down and attach along the first rib, with the spinal nerves and brachial plexus being sandwiched between them. The region where the brachial plexus and subclavian artery exit together from between the scalenes and over the first rib is a potential site of entrapment (thoracic outlet syndrome). The brachial plexus divisions lie deep to the clavicle, while the cords and their branches are deep to the pectoralis minor and coracoid process. In the axilla, the distal brachial plexus cords lie between the clavipectoral fascia (superficial) and subscapularis muscle (deep).
The subclavian vessels exit the thorax through the ring of the first rib. The anterior scalene runs between the subclavian artery and vein, with the artery being posterior and adjacent to the C8, T1 spinal nerves and lower trunk, and the vein anterior to the anterior scalene, just deep to the clavicle. Originating from the subclavian artery soon after it emerges from the thorax, two small arterial branches traverse the surface of the brachial plexus across the posterior triangle of the neck. The more superior one is the transverse (superficial) cervical artery and the lower one is the suprascapular artery. The latter joins up with the suprascapular nerve near the suprascapular notch. A third artery, called the dorsal scapular artery, often passes between the upper and middle trunks of the brachial plexus.
The blood supply to the proximal brachial plexus is from the subclavian system. Specifically, the vertebral and ascending cervical arteries supply C5 and C6, the deep cervical artery irrigates C7, and the superior intercostal arteries cover C8 and T1.
As expected, the venous anatomy surrounding the brachial plexus is variable. The subclavian vein runs anterior to the anterior scalene and receives the axillary vein, which runs medial and ventral to the axillary artery in the axilla. The posterior cord lies deep to these two vessels. The external jugular vein drains into the subclavian vein under the clavicular attachment of the sternocleidomastoid. The external jugular vein, in general, begins at the angle of the jaw, and runs toward the shoulder by crossing the lower, anterior aspect of the posterior triangle. It runs deep to the platysma, and occasionally deep to the posterior belly of the omohyoid.
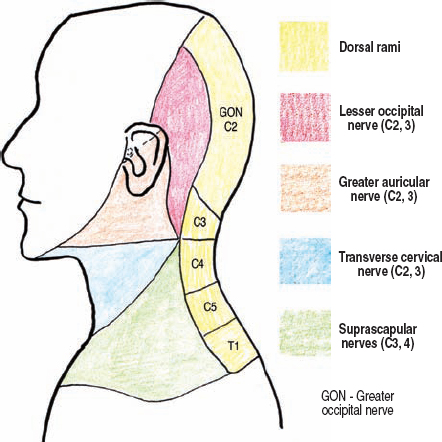
Figure 4-25 Head and neck sensory coverage, excluding the face. Sensory branches from the cervical plexus, along with the dorsal rami of the upper cervical spinal nerves, provide innervation to this area. Of note, the greater occipital nerve is made up solely of the dorsal rami of C2, and is not considered a branch of the cervical plexus.
 The Cervical Plexus
The Cervical Plexus
The other plexus of the neck, the cervical plexus, is made up of the ventral rami of C1 to C4. After emerging from their respective intervertebral foramina, these ventral rami merge and communicate with each other, ultimately yielding several deep (motor) and superficial (sensory) branches, which originate underneath the sternocleidomastoid muscle.
The deep branches remain under the sternocleidomastoid, innervating various neck muscles (scalenes, strap muscles, levator scapula, etc.). The ansa cervicalis innervates the strap muscles of the neck, and is derived from these deep motor branches. The superior loop of the ansa cervicalis is made from the C1 and C2 ventral rami, while the inferior loop is from C2 and C3. The superior and inferior loops of the ansa cervicalis join anteriorly to the jugular vein.
In contrast to the deep branches, the superficial branches of the cervical plexus pour over (around and superficial to) the posterior edge of the sternocleidomastoid muscle to provide sensory coverage from the neck down to the shoulder and upper chest, including the area just below the clavicle (Fig. 4-25). Four named sensory branches originate from the cervical plexus, from superior to inferior: the lesser occipital, greater auricular, transverse cervical, and supraclavicular (Fig. 4-26). The only nerve from the cervical plexus that crosses the posterior triangle of the neck is the supraclavicular nerve and its terminal branches. If one follows the great auricular nerve back to the point where it emerges from below the sternocleidomastoid muscle, the spinal accessory nerve can often be located just a few millimeters more cranial to this point.
 The greater occipital nerve originates from the dorsal ramus of C2. C1 provides no sensation to the skin. The spinal accessory nerve (CN XI) crosses the most-cranial aspect of the neck’s posterior triangle.
The greater occipital nerve originates from the dorsal ramus of C2. C1 provides no sensation to the skin. The spinal accessory nerve (CN XI) crosses the most-cranial aspect of the neck’s posterior triangle.
 Spinal Accessory Nerve (CN XI)
Spinal Accessory Nerve (CN XI)
The spinal accessory nerve is made up of intraspinal branches from C1 to C4, and the medulla. These branches merge intradurally, with the nerve, once formed, exiting the skull base via the jugular foramen. Its relationship to the jugular vein just below the skull base is variable. After the spinal accessory nerve innervates the sternocleidomastoid muscle, which is also innervated by deep motor branches of the cervical plexus, it exits from below the sternocleidomastoid and enters the posterior triangle of the neck, approximately 8 cm superior to the clavicle. The spinal accessory nerve travels toward the top of the shoulder, eventually passing under the trapezius muscle, which it innervates (Fig. 4-26). As mentioned previously, this nerve commonly emerges from under the sternocleidomastoid muscle just cranial to the greater auricular nerve, the latter being an excellent surgical landmark. Across the posterior triangle, the spinal accessory nerve is interwoven with a major chain of lymph nodes. For this reason, the most common cause of isolated spinal accessory nerve palsy is iatrogenic injury following cervical lymph node dissection or biopsy. Alternatively, a painful, idiopathic spinal accessory neuropathy may also occur, which is thought to be a variant of acute brachial plexitis. Vernet syndrome consists of spinal accessory, vagus, and glossopharyngeal damage at the jugular foramen, through which all three of these nerves pass. This syndrome is usually from a local metastatic deposit or schwannoma.
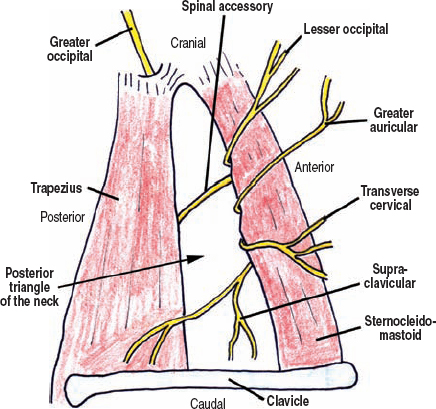
Figure 4-26 Cervical plexus and spinal accessory nerve (schematic). Four named sensory branches originate from the cervical plexus, from superior to inferior: the lesser occipital, greater auricular, transverse cervical, and supraclavicular. The only sensory nerve from the cervical plexus that crosses the posterior triangle of the neck is the supraclavicular nerve. The spinal accessory nerve emerges from under the sternocleidomastoid just a few millimeters cranially to the greater auricular nerve.
A spinal accessory nerve palsy causes trapezial weakness. A patient with a weak trapezius will report trouble abducting the arm above the head (laterally), as well as shoulder girdle discomfort. Upward rotation of the scapula, mediated by the trapezius, assists the deltoid in abducting the arm above 90 degrees. Discomfort is thought to be from stress to muscles and ligaments that compensate for the trapezial weakness. At rest, the affected shoulder often lies lower than the unaffected one. Even with a complete trapezial palsy, shoulder shrug weakness seldom occurs. This is because the levator scapula muscle also shrugs the shoulder (innervated by the C3 and C4 via the cervical plexus). Weakness of the sternocleidomastoid muscle is rare, not only because the motor branches from the spinal accessory nerve branch quite proximally, but also because this muscle receives co-innervation from the cervical plexus.
Secondary to the trapezial weakness, a spinal accessory palsy also causes scapular winging. Trapezial winging is mild at rest and usually involves the upper border of the scapula, although this is variable. All types of winging (serratus anterior, trapezial, and rhomboid) are worse when the arm (partially flexed at the elbow) is pushed across the chest or in front of the body against resistance. However, only serratus anterior weakness causes winging when an extended, protracted arm is resisted. The presence of rhomboid weakness helps differentiate rhomboid versus trapezial winging. Table 4-1 compares the three muscular causes of scapular winging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



