1
The Diagnostic Anatomy of the Median Nerve
The median nerve has contributions from four nerve roots via the brachial plexus (C6 to T1), and maintains a “median” location throughout its anatomical course down the upper extremity; whether along the intermuscular septum between the biceps and triceps, in the antecubital fossa, or distally at the wrist—the median nerve is always in the anatomical “center.” From a functional standpoint, this nerve innervates key muscles of the hand, including those responsible for wrist flexion and movement of the first three fingers. Compression of the median nerve at the wrist results in carpal tunnel syndrome, the most common peripheral nerve entrapment seen in clinical practice.
 Anatomical Course
Anatomical Course
The Arm
The median nerve is derived from both the lateral and medial cords of the brachial plexus, with the lateral cord providing mostly sensory axons from C6 and C7, and the medial cord providing motor axons from C8 and T1. Therefore, the majority of motor input is from the medial cord. Based on their relationship to the axillary artery deep to the pectoralis minor muscle, the brachial plexus cords receive their names (medial, lateral, and posterior). In agreement with this nomenclature, when viewing the upper arm from its medial (inside) surface toward the axilla, the medial cord is medial to the axillary artery and the lateral cord is lateral to the axillary artery. Terminal divisions of the medial and lateral cords merge to create the median nerve, forming a Y-shaped confluence over the superficial surface of the brachial artery. Once formed, the median nerve travels distally while maintaining an intimate relationship with this artery in the upper arm.
The median nerve remains slightly lateral and superficial to the brachial artery as it passes down the arm. It runs anterior and parallel to the intermuscular septum, which separates the triceps from the arm flexors (i.e., biceps brachii, brachialis) (Fig. 1-1). When the inside of the upper arm is viewed from a medial viewpoint (e.g., with the arm abducted and externally rotated), the median nerve runs down the midline toward the antecubital fossa. About halfway down the arm, the median nerve crosses over the top of the brachial artery and then rests just medial to it by the time it passes under the bicipital aponeurosis (lacertus fibrosis) in the proximal forearm. The median nerve innervates no muscles in the arm, and in general, has no branches.
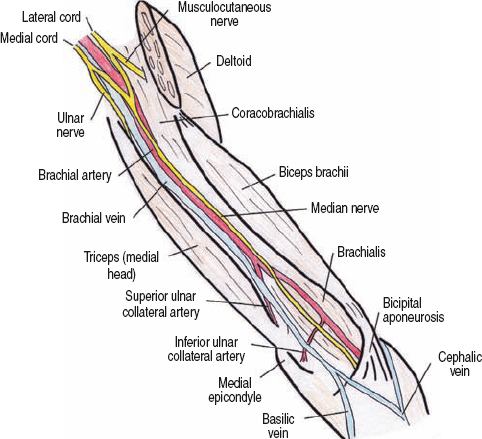
Figure 1-1 Median nerve in upper arm. The median nerve remains slightly lateral and superficial to the brachial artery as it passes down the arm. About halfway down the arm, the median nerve crosses over the top of the brachial artery and then rests just medial to it by the time it passes under the bicipital aponeurosis.
 A few anatomical variations of the median nerve can occur in the arm. First, the medial and lateral cord components, which form the median nerve, may not fuse in the axilla, but instead join at various points along the arm, sometimes as low as the elbow. Second, these components may alternatively loop under the axillary/brachial artery, rather than superficial to it, when joining to form the median nerve. Finally, in some persons, the lateral component of the median nerve from the lateral cord is very small, with the majority of the median nerve’s C6 and C7 fibers running instead in the musculocutaneous nerve, only to be returned to the median nerve via a communication about halfway down the arm. This temporary misrouting of innervation is not an uncommon phenomenon; it is almost as if the fibers took a wrong turn during development, asked for some directions, and rerouted themselves.
A few anatomical variations of the median nerve can occur in the arm. First, the medial and lateral cord components, which form the median nerve, may not fuse in the axilla, but instead join at various points along the arm, sometimes as low as the elbow. Second, these components may alternatively loop under the axillary/brachial artery, rather than superficial to it, when joining to form the median nerve. Finally, in some persons, the lateral component of the median nerve from the lateral cord is very small, with the majority of the median nerve’s C6 and C7 fibers running instead in the musculocutaneous nerve, only to be returned to the median nerve via a communication about halfway down the arm. This temporary misrouting of innervation is not an uncommon phenomenon; it is almost as if the fibers took a wrong turn during development, asked for some directions, and rerouted themselves.
The Antecubital Fossa/Elbow
At the elbow, the anatomy of the median nerve becomes more complex. It enters the antecubital fossa medial to the biceps brachii, passing over the brachialis muscle, which separates the nerve from the distal humerus. In the antecubital fossa, the median nerve passes under three successive arches or tunnels, bringing it deep into the forearm, only for it to re-emerge in the distal forearm prior to reaching the hand (Fig. 1-2). The first arch it passes under is the bicipital aponeurosis (lacertus fibrosis), which is a thick layer of fascia attaching the biceps brachii to the proximal forearm flexor mass. Of note, one may directly palpate the median nerve prior to its diving below this aponeurosis by palpating two fingerbreadths proximal, and two lateral, to the medial epicondyle. Under this aponeurosis, the biceps tendon and brachial artery are both lateral, while the humeral head of the pronator teres muscle is medial to the median nerve (Fig. 1-3).
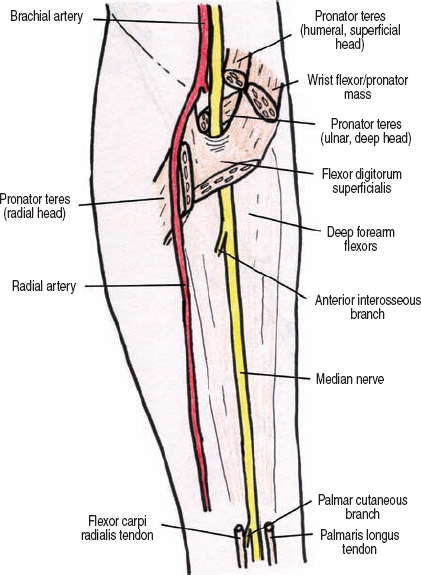
Figure 1-2 Median nerve in the forearm. In the antecubital fossa, the median nerve passes under three successive arches or tunnels (bicipital aponeurosis, pronator teres, and flexor digitorum superficialis), bringing it deep into the forearm, only for it to re-emerge in the distal forearm prior to reaching the hand.
A short distance past the proximal edge of the bicipital aponeurosis, the median nerve dives below a second structure–the humeral head of the pronator teres. The pronator teres is a Y-shaped muscle with the bottom stem of the Y inserting into the radius distally and laterally. When viewing the antecubital fossa from anterior with the forearm supinated and extended, the Y of the pronator teres is turned on its side, so that the upper limbs of the Y are proximal, medial, and on top of each other. These proximal two heads include a larger superficial head that attaches to the humerus (humeral head), and a deeper, smaller head that attaches more distally to the ulna (ulnar head). The median nerve passes right in the crotch of this Y, with the ulnar head deep, and the humeral head superficial.
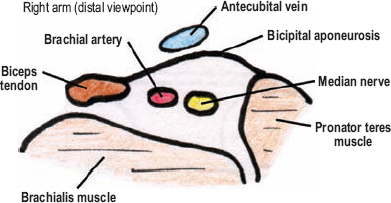
Figure 1-3 Cross section of median nerve in the antecubital fossa. The bicipital aponeurosis is superficial, the brachialis is deep, the biceps tendon and brachial artery are both lateral, and the humeral head of the pronatorteres muscle is medial.
Next, just beyond the pronator teres, the median nerve almost immediately passes under a third structure: the two heads of the flexor digitorum superficialis (sublimis). This muscle’s humeroulnar head is medial; its radial head is lateral. The flexor digitorum superficialis, in essence, forms a second Y through which the median nerve once again passes. In contrast to the pronator teres, however, when viewed anteriorly with the forearm supinated, the flexor digitorum superficialis’ Y is not turned on its side. A fibrous ridge between its two heads is termed the sublimis ridge, and under this ridge, the median nerve passes.
 Variations in this area are predominantly musculotendinous. Either the pronator teres or the flexor digitorum superficialis may have only one head, not two, and their proximal origins may vary. These muscular variations potentially create anatomical situations that may predispose to median nerve entrapment in the antecubital fossa.
Variations in this area are predominantly musculotendinous. Either the pronator teres or the flexor digitorum superficialis may have only one head, not two, and their proximal origins may vary. These muscular variations potentially create anatomical situations that may predispose to median nerve entrapment in the antecubital fossa.
The Forearm
The median nerve travels down the center of the forearm deep to the digitorum superficialis, but superficial to the underlying flexor digitorum profundus. More precisely, the median nerve lies toward the lateral margin of the flexor digitorum profundus, near the flexor pollicis longus, which is the neighboring muscle on its lateral aspect. About one third or halfway down the forearm, an important branch of the median nerve, the anterior interosseous nerve, exits from its dorso-lateral aspect. Once formed, the anterior interosseous nerve passes deeper in the forearm to run between the radius and ulna on the interosseous membrane, between and below the muscle bellies of the flexor digitorum profundus and flexor pollicis longus. This branch terminates in the distal forearm deep to the pronator quadratus. Near its origin, the anterior interosseus nerve passes under one or more fibrous ridges that originate off the pronator teres or flexor digitorum superficialis.
The median nerve proper continues down the arm, and becomes, once again, superficial about 5 cm proximal to the wrist crease, just medial to the flexor carpi radialis tendon. This muscle’s tendon is the most prominent one that bowstrings proximal to the wrist (just lateral to midline) when the wrist is flexed against resistance. The palmaris longus tendon, when present, lies just medial to the median nerve at the proximal wrist. Once superficial, and before entering the hand, the median nerve gives a pure sensory branch, the palmar cutaneous branch, which runs superficial to the carpal tunnel and ramifies over the proximal, radial half of the palm, particularly over the thenar eminence. Occasionally, this sensory branch passes through its own tunnel in the transverse carpal ligament.
The brachial artery passes under the bicipital aponeurosis, where it bifurcates into the radial and ulnar arteries. The radial artery passes distally, near the superficial sensory radial nerve. The ulnar artery, alternatively, passes deep to the flexor-pronator mass, where it loops under the median nerve. In the distal forearm, the ulnar artery joins the ulnar nerve, and together they travel toward the wrist. Prior to passing below the median nerve in the antecubital fossa, the ulnar artery gives the interosseous communis artery, which shortly thereafter divides into the anterior and posterior interosseous arteries. The anterior interosseous artery passes distally with the anterior interosseous nerve, deep between the flexor pollicis longus and flexor digitorum profundus.
The Wrist/Hand
The median nerve passes through the center of the wrist in the carpal tunnel. A common analogy is to think of the carpal tunnel as an upside-down table. The tabletop is composed of carpal bones, with the legs of the table being the hook of the hamate and pisiform medially, and the tubercle of the trapezium and distal pole of the scaphoid laterally. Stretched over these legs, like a rug on an imaginary floor, is the thick transverse carpal ligament. From a volar viewpoint, the median nerve is the most superficial of nine structures running though the carpal tunnel. These other structures include the flexor pollicis longus tendon, four superficial flexor tendons, and four deep flexor tendons (Fig. 1-4). The palmaris longus tendon does not enter the carpal tunnel, but instead attaches more proximally to the superficially located palmaris aponeurosis. The flexor carpi radialis also does not pass through the carpal tunnel, but enters its own small tunnel, located lateral to the carpal tunnel, attaching to the second metacarpal bone.
After passing through the carpal tunnel, the median nerve gives a branch off its radial side: the thenar motor branch (or recurrent thenar motor branch). Then in the deep palm, the median nerve divides into two divisions, radial and ulnar. The radial division divides into the common digital nerve to the thumb, and the proper digital nerve to the radial half of the index finger. The common digital nerve to the thumb subsequently divides into the two proper digital nerves to the thumb. The ulnar division of the median nerve divides into the common digital nerves of the second and third web spaces, which also subsequently divide into proper digital nerves. The ulnar and radial divisions of the median nerve run deep (or dorsal) to the superficial palmar arch, but superficial to the flexor tendons.
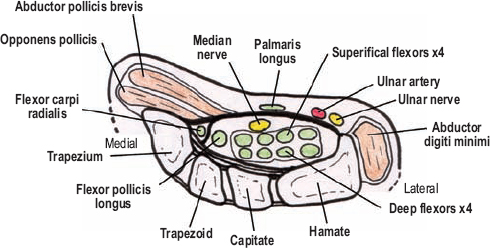
Figure 1-4 Cross section of median nerve in the carpal tunnel. From a volar viewpoint, the median nerve is the most superficial of nine structures running though the carpal tunnel. These other structures include the flexor pollicis longus tendon, four superficial flexor tendons, and four deep flexor tendons.
 Numerous variations in the origin and path of the thenar motor branch can occur. For instance, this motor branch may originate within the carpal tunnel, may pierce the transverse carpal ligament for a more direct route to the thenar muscles, and even emerge on the ulnar side of the median nerve, only to then cross deep or superficial to the median nerve to reach the thenar muscles. Other median nerve variations include (1)an early branching of the median nerve into radial and ulnar divisions proximal to the carpal tunnel (which often occurs with a “persistent median artery”), and (2) a connection between the thenar motor branch and the deep palmar branch of the ulnar nerve (discussed below).
Numerous variations in the origin and path of the thenar motor branch can occur. For instance, this motor branch may originate within the carpal tunnel, may pierce the transverse carpal ligament for a more direct route to the thenar muscles, and even emerge on the ulnar side of the median nerve, only to then cross deep or superficial to the median nerve to reach the thenar muscles. Other median nerve variations include (1)an early branching of the median nerve into radial and ulnar divisions proximal to the carpal tunnel (which often occurs with a “persistent median artery”), and (2) a connection between the thenar motor branch and the deep palmar branch of the ulnar nerve (discussed below).
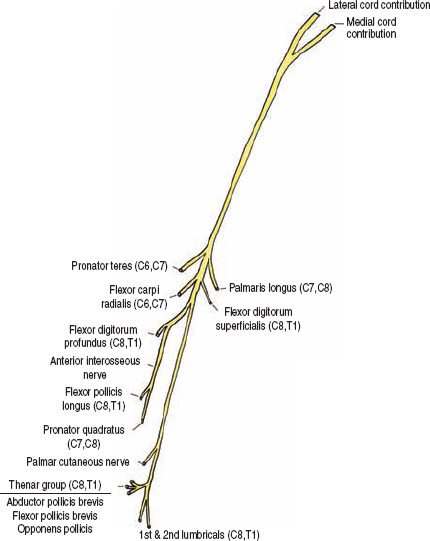
Figure 1-5 Motor innervation of the median nerve. The median nerve does not innervate any muscles in the upper arm. It does, however, innervate numerous muscles in the forearm and hand that are involved in forearm pronation, wrist flexion, flexion of the digits (especially the first three), and thumb opposition and abduction.
 Motor Innervation and Testing
Motor Innervation and Testing
The median nerve does not innervate any muscles in the upper arm. It does, however, innervate numerous muscles in the forearm and hand that are involved in forearm pronation, wrist flexion, flexion of the digits (especially the first three), and thumb opposition and abduction (Fig. 1-5). To aid memorization, these muscles may be separated into four sequential groups: proximal forearm, anterior interosseous, thenar motor, and terminal.
The Proximal Forearm Group
This group comprises four muscles: pronator teres, flexor carpi radialis, flexor digitorum superficialis, and palmaris longus. The pronator teres (C6, C7) is the main pronator of the forearm and the first muscle innervated by the median nerve. Branches to the pronator teres exit the median nerve at the lowest aspect of the upper arm, prior to the median nerve passing between the two heads of the pronator teres. From a mechanical perspective, the forearm needs to be extended for the pronator teres to have mechanical advantage. Therefore, to test this muscle the patient’s forearm is first extended and then fully pronated. The patient is instructed to resist supination by the examiner (Fig. 1-6). The flexor carpi radialis (C6, C7) is one of the two major wrist flexors. The other is the flexor carpi ulnaris, which is innervated by the ulnar nerve. The flexor carpi radialis is the important wrist flexor, with loss of function severely limiting wrist flexion except in an ulnar direction. Test the flexor carpi radialis by having the patient flex the wrist along the trajectory of the forearm (Fig. 1-7). For severe weakness, have the patient flex the wrist with the forearm on a table, ulnar side down, which eliminates gravity. The tendon of the flexor carpi radialis can be seen and felt proximal to the wrist. The palmaris longus (C7, C8) is attached to the palmar aponeurosis and corrugates the palmar skin. This muscle is not readily examined for muscular strength, and in fact, is absent in about 15% of the population. The flexor digitorum superficialis (also known as the sublimis muscle, C8, T1) is also innervated by the median nerve and mediates flexion of the second to fifth digits (all except the thumb) at their proximal interphalangeal joints. To assess proximal interphalangeal joint flexion, each finger is tested separately. Placing your fingers between the patient’s single finger to be tested and the remaining fingers isolates this movement (Fig. 1-8). This maneuver places the finger to be tested in mild flexion at the metacarpal-phalangeal (knuckle) joint, and simultaneously stabilizes the remaining fingers in extension, a position that allows isolation of the flexor digitorum superficialis.

Figure 1-6 Pronator teres (C6, C7) assessment: The patient’s forearm is extended and fully pronated. The patient is then instructed to resist supination of the forearm by the examiner.

Figure 1-7 Flexor carpi radialis (C6, C7) assessment: The patient flexes the wrist along the trajectory of the forearm. For severe weakness, have the patient flex the wrist with the forearm on a table, ulnar side down, which eliminates gravity. Its tendon can be seen and felt proximal to the wrist.

Figure 1-8 Flexor digitorum superficialis (C8, T1) assessment: To test proximal interphalangeal joint flexion, the supinated forearm and hand are placed straight. Each finger is tested separately. Placing your fingers between the single finger to be tested and the remaining fingers that are immobilized isolates this movement. This maneuver places the finger to be tested in mild flexion at the metacarpal–phalangeal (knuckle) joint, and stabilizes the remaining fingers in extension, a position that allows isolation of the flexor digitorum superficialis.
A topographical aid in identifying the muscles of the medial forearm flexor mass is to place a hand on the opposite forearm with its thenar eminence on the medial epicondyle, the ring finger along the medial border of the forearm, and the rest of the fingers naturally lying over the forearm pointing in a distal trajectory toward the other hand. In this position, the thumb is over the pronator teres, the index finger is over the flexor carpi radialis, the long finger is over the palmaris longus, and the ring finger is along the flexor carpi ulnaris, the latter being innervated by the ulnar nerve.
 In patients with pronator teres (and pronator quadratus, see below) weakness, a combination of arm abduction and internal rotation can allow gravity to mimic arm pronation. Furthermore, when testing pronation the patient should keep the fingers and hand relaxed to avoid substitution for pronation by the flexor carpi radialis and long finger flexors. When testing the finger flexors the wrist should be kept neutral and not allowed to extend because with wrist extension a tenodesis (distal joint movement mediated by lengthening the distance a tendon has to pass by changing the position of a more proximal joint) may occur that causes the fingers to passively flex.
In patients with pronator teres (and pronator quadratus, see below) weakness, a combination of arm abduction and internal rotation can allow gravity to mimic arm pronation. Furthermore, when testing pronation the patient should keep the fingers and hand relaxed to avoid substitution for pronation by the flexor carpi radialis and long finger flexors. When testing the finger flexors the wrist should be kept neutral and not allowed to extend because with wrist extension a tenodesis (distal joint movement mediated by lengthening the distance a tendon has to pass by changing the position of a more proximal joint) may occur that causes the fingers to passively flex.
The Anterior Interosseous Group
This nerve innervates three deeply situated anterior forearm muscles: the flexor digitorum profundus (to the second and third digits), the flexor pollicis longus, and the pronator quadratus. The flexor digitorum profundus (C8, T1), as a whole, is innervated by both the median and ulnar nerves. The median nerve controls flexion of the distal interphalangeal joint of the second, and partly, the third digits; the ulnar nerve controls this muscle’s action upon the third (partly), fourth, and fifth digits. Distal interphalangeal joint flexion of the third (or long) digit has variable dominance by the median or ulnar nerves. Additionally, even with complete denervation of one of these nerves, some movement of the long finger is usually preserved because both the median and ulnar portions of the flexor digitorum profundus act via a common tendon to this digit. Therefore, to assess in isolation median innervation of the flexor digitorum profundus one should concentrate on the index finger. To do so, hold the metacarpal-phalangeal and proximal interphalangeal joints immobile, and have the patient flex the distal phalanx against your resistance (Fig. 1-9). The flexor pollicis longus (C8, T1) performs a function similar to the profundus, but on the thumb; it flexes the distal phalanx of the thumb at the interphalangeal joint. Assess the flexor pollicis longus by immobilizing the thumb, except the interphalangeal joint, and ask the patient to flex the distal phalanx against resistance (Fig. 1-10). A quick way to assess both flexor digitorum profundus and flexor pollicis longus innervation from the anterior interosseous nerve is to ask the patient to make an okay sign by touching the tips of the thumb and index finger together. With weakness in these muscles, the distal phalanges cannot flex, and instead of the fingertips touching, the volar surfaces of each distal phalanx make contact (Fig. 1-11). The third muscle innervated by the anterior interosseous nerve is the pronator quadratus (C7, C8). This is a significantly weaker forearm pronator that the pronator teres. In fact, weakness in this muscle is often not readily apparent with a functioning pronator teres. However, with the forearm fully flexed, which removes the mechanical advantage of the pronator teres, weakness of the pronator quadratus should be detectable when compared with the normal arm. Test the pronator quadratus by having the patient resist supination of a fully flexed and pronated forearm (Fig. 1-12).

Figure 1-9 Flexor digitorum profundus (C8, T1) assessment: To assess the median innervation of the flexor digitorum profundus one should concentrate on the index finger. To do so, hold the metacarpal-phalangeal and proximal interphalangeal joints immobile, and have the patient flex the distal phalanx against your resistance.
 When testing the flexor digitorum profundus or the flexor pollicis longus, do not let the patient extend the distal interphalangeal joints prior to flexion because the passive reflexion may mimic active joint flexion.
When testing the flexor digitorum profundus or the flexor pollicis longus, do not let the patient extend the distal interphalangeal joints prior to flexion because the passive reflexion may mimic active joint flexion.
The Thenar Group
The thenar group consists of three muscles innervated by the thenar motor branch of the median nerve. The first is the abductor pollicis brevis (C8, T1), which as the name implies, abducts the thumb. Thumb abduction may be separated into two vectors: palmar abduction away from the plane of the palm (mediated by the abductor pollicis brevis), and radial abduction away from the line of the forearm (mediated by the abductor pollicis longus). Therefore, even with a complete palsy of the abductor pollicis brevis, radial abduction of the thumb can still occur. To test the abductor pollicis brevis, resist movement of the thumb away from the plane of the palm (palmar abduction) while the metacarpals of the remaining fingers are immobilized (Fig. 1-13). The flexor pollicis brevis (C8, T1) is innervated by both the median nerve (its superficial head) and ulnar nerve (its deep head). This muscle flexes the thumb at the metacarpal-phalangeal joint. To test the flexor pollicis brevis, immobilize the thumb’s interphalangeal joint and have the patient flex at the metacarpal-phalangeal joint (Fig. 1-14). Make certain the distal interphalangeal joint does not flex because in allowing this, substitution by the flexor pollicis longus occurs. Use your other hand to immobilize the first metacarpal to reduce substitution by the opponens pollicis. Because of its dual innervation, even with complete thenar motor branch palsies some thumb flexion should still occur. However, when compared with the normal hand, relative weakness is usually evident. Assess the opponens pollicis (C8, T1) by having the patient forcibly maintain contact between the volar pads of the distal thumb and fifth digit while you try to pull the distal first metacarpal away from the fifth digit (Fig. 1-15). Although the median nerve solely controls thumb opposition, a combination of thumb adduction (adductor pollicis, ulnar nerve) and thumb flexion (flexor pollicis brevis, deep head, ulnar nerve) may mimic thumb opposition when there is complete median nerve palsy present.

Figure 1-10 Flexor pollicis longus (C8, T1) assessment: Immobilize the thumb, except the interphalangeal joint, and then ask the patient to flex the distal phalanx against resistance.

Figure 1-11 “Okay” or “circle” sign with anterior interosseous nerve weakness. A quick way to assess the flexor digitorum profundus and flexor pollicis longus innervation from the anterior interosseous nerve is to ask the patient to make an okay sign by touching the tips of the thumb and index finger together. With weakness in these muscles, the distal phalanges cannot flex, and instead of the fingertips touching, the volar surfaces of each distal phalanx make contact.

Figure 1-12 Pronator quadratus (C7, C8) assessment: Have the patient resist supination of a fully flexed and pronated forearm. With full forearm flexion, pronation by the usually dominant pronator teres is minimized.

Figure 1-13 Abductor pollicis brevis (C8, T1) assessment: Resist movement of the thumb away from the plane of the palm (palmar abduction), while stabilizing the metacarpals of the remaining fingers.

Figure 1-14 Flexor pollicis brevis (C8, T1) assessment: The patient flexes the thumb at the metacarpal-phalangeal joint against resistance placed over both the proximal and distal phalanges. Make certain the distal interphalangeal joint does not flex because in allowing this, substitution by the flexor pollicis longus occurs. Use your other hand to immobilize the first metacarpal to reduce substitution by the opponens pollicis. Because of its dual innervation, even with complete thenar motor branch palsies some thumb flexion still occurs.

Figure 1-15 Opponens pollicis (C8, T1) assessment: Have the patient forcibly maintain contact between the volar pads of the distal thumb and fifth digit, while you try to pull the distal first metacarpal away from the fifth digit. Although thumb opposition is only innervated by the median nerve, a combination of thumb adduction (adductor pollicis, ulnar nerve) and thumb flexion (flexor pollicis brevis, deep head, ulnar nerve) may mimic thumb opposition even when there is complete median nerve palsy present.
 Examining the motor function of the thumb is not straightforward. The key principle is to compare the results with the normal hand, keeping in mind that even following complete loss of median nerve function, some movement of the thumb will still be present secondary to either true muscle action via radial and ulnar innervation, or from substitutions by adjacent muscles.
Examining the motor function of the thumb is not straightforward. The key principle is to compare the results with the normal hand, keeping in mind that even following complete loss of median nerve function, some movement of the thumb will still be present secondary to either true muscle action via radial and ulnar innervation, or from substitutions by adjacent muscles.
The Terminal Group
The terminal group simply consists of the first and second lumbricals (C8, T1), which are innervated by the terminal radial and ulnar divisions of the median nerve, respectively. To examine the first lumbrical, stabilize the index finger in a hyper-extended position at the metacarpal-phalangeal joint and then provide resistance as the patient extends the finger at the proximal interphalangeal joint (Fig. 1-16).
 The muscular origins and insertions of the lumbricals are quite variable. In fact, one or more may be absent. This variability and/or absence of the lumbricals is functionally acceptable because flexion at the metacarpal-phalangeal joints, as well as extension at the proximal interphalangeal joints when the metacarpal-phalangeal joints are hyper-extended (both movements performed by the lumbricals), are also partly performed by the palmar or dorsal interossei muscles. Therefore, whenever you test lumbrical strength, it is being assisted by the interossei.
The muscular origins and insertions of the lumbricals are quite variable. In fact, one or more may be absent. This variability and/or absence of the lumbricals is functionally acceptable because flexion at the metacarpal-phalangeal joints, as well as extension at the proximal interphalangeal joints when the metacarpal-phalangeal joints are hyper-extended (both movements performed by the lumbricals), are also partly performed by the palmar or dorsal interossei muscles. Therefore, whenever you test lumbrical strength, it is being assisted by the interossei.

Figure 1-16 Lumbrical of second digit (C8, T1) assessment: Stabilize the patient’s index finger in a hyper-extended position at the metacarpal-phalangeal joint and then provide resistance as the patient extends the finger at the proximal interphalangeal joint.
 Sensory Innervation
Sensory Innervation
Although the median nerve only provides sensory innervation to a relatively small portion of the upper extremity, it is probably the most important. Via three branches, the palmar cutaneous nerve, and the radial and ulnar divisions of the median nerve (via digital branches) in the palm, the median nerve carries cutaneous sensory information from the radial two thirds of the palm, and the volar surfaces of the first, second, third, and radial half of the fourth digits (Fig. 1-17). Dorsal fingertip sensation is also carried by the median nerve, including the dorsum of the ulnar half of the distal phalanx of the thumb, as well as the dorsum of the distal phalanges of the second, third, and radial half of the fourth digits.
The palmar cutaneous branch innervates the majority of the median nerve’s palmar distribution, while that of the digits is through small branches of the median nerve’s radial and ulnar divisions in the palm. Therefore, one should use the thenar eminence to assess the palmar cutaneous branch, and the distal portion of the second and third digits to assess the sensory fibers that pass through the carpal tunnel. In addition to sensory cutaneous innervation, the median nerve also carries sensory fibers for joint proprioception and muscle tension, especially from the elbow and wrist. Although many refer to the anterior interosseous nerve as a “pure” motor nerve without cutaneous innervation, it does, in fact carry sensory fibers from the wrist joints and muscles.
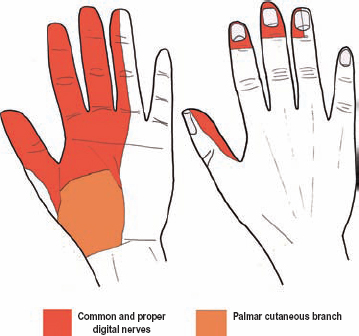
Figure 1-17 Sensory innervation of the median nerve. The median nerve carries cutaneous sensory information from the radial two thirds of the palm, and the volar surfaces of the first, second, third, and radial half of the fourth digit.
 The ulnar border of the median nerve’s sensory innervation in the hand may vary, depending on its relationship, or dominance over, the adjacent ulnar nerve. For example, either the ulnar or the median nerve may receive sensory innervation from the complete volar fourth digit. Furthermore, the percentage of the palm’s median innervated region carried by the palmar cutaneous branch versus branches of the radial and ulnar divisions of the median nerve is also variable.
The ulnar border of the median nerve’s sensory innervation in the hand may vary, depending on its relationship, or dominance over, the adjacent ulnar nerve. For example, either the ulnar or the median nerve may receive sensory innervation from the complete volar fourth digit. Furthermore, the percentage of the palm’s median innervated region carried by the palmar cutaneous branch versus branches of the radial and ulnar divisions of the median nerve is also variable.
Martin–Gruber and Riche–Cannieu Anastomoses
Cross talk, or anastomoses, between the ulnar nerve and either the median nerve or its anterior interosseous branch may occur in the forearm. Many variations are possible, and knowing a few of the more common ones is clinically useful.
The Martin–Gruber anastomosis occurs in up to 15% of patients and involves the median innervated thenar muscles (opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis). In this anomaly, instead of their usual pathway down the median nerve and out the thenar motor branch, nerve fibers destined for these three muscles run instead down the anterior interosseous branch, are transferred through the flexor digitorum profundus muscle to the ulnar nerve, and then enter the palm via the deep ulnar branch. Deep in the palm, these fibers are eventually transferred back to the thenar motor branch, where they innervate their respective muscles. This distal communication between the deep ulnar branch and the thenar motor branch in the palm is termed the Riche–Cannieu anastomosis, and is anatomically (not functionally) present in at least 50% of patients.
Therefore, when motor axons destined for the median nerve’s thenar muscles cross over to the ulnar nerve via the Martin–Gruber anastomosis, low median nerve injuries in the wrist or forearm spare thenar motor function. The corollary is that damage to the ulnar nerve at the wrist in this anatomical situation leads to a much more severe deficit of intrinsic hand function than expected.
 Another version of the Martin–Gruber anastomosis involves the hand intrinsic muscles usually innervated by the deep ulnar branch in the hand, including the lumbricals, first dorsal interosseous, adductor pollicis, and deep (ulnar) portion of the flexor pollicis brevis. For this variation, motor axons innervating these muscles accidentally pass down the median nerve and then pass back to the ulnar nerve halfway down the forearm via communications with the anterior interosseous branch of the median nerve, through or around the flexor digitorum profundus muscle. Yet another variation occurs when the median nerve’s thenar motor branch aberrantly innervates the third lumbrical, or even all the lumbricals, via the Riche–Cannieu anastomosis
Another version of the Martin–Gruber anastomosis involves the hand intrinsic muscles usually innervated by the deep ulnar branch in the hand, including the lumbricals, first dorsal interosseous, adductor pollicis, and deep (ulnar) portion of the flexor pollicis brevis. For this variation, motor axons innervating these muscles accidentally pass down the median nerve and then pass back to the ulnar nerve halfway down the forearm via communications with the anterior interosseous branch of the median nerve, through or around the flexor digitorum profundus muscle. Yet another variation occurs when the median nerve’s thenar motor branch aberrantly innervates the third lumbrical, or even all the lumbricals, via the Riche–Cannieu anastomosis
 Clinical Findings and Syndromes
Clinical Findings and Syndromes
The Arm
Complete Palsy
Damage to the median nerve in the arm is usually secondary to trauma: lacerations, gunshots, or blunt contusions. Because of the median nerve’s close proximity to the brachial artery, concomitant injury to this vessel may occur. Furthermore, in the proximal arm both the ulnar and radial nerves are in close proximity to the median nerve, and therefore, all three of these nerves can be simultaneously injured (triad neuropathy). The Saturday night palsy, which can occur from hanging the arm over the back of a chair and passing out (drunk), or the honeymooners palsy, which occurs when the arm is under the neck of someone sleeping for a length of time, can both cause a median nerve palsy. Although classically injuring the radial nerve, a crutch head can also damage the median nerve in the axilla.
A complete injury to the median nerve is debilitating. The forearm cannot pronate against gravity or resistance. The hand can only weakly flex at the wrist in an ulnar direction. The thumb cannot be opposed or abducted in a palmar direction. Lumbrical weakness in the index and long fingers is present. Numbness occurs on the volar surfaces of the first three and a half digits, and radial two thirds of the palm. Additionally, when a patient with a complete median palsy is asked to make a fist, the first digit barely flexes, the second digit partially flexes (secondary to substitution from nonmedian innervated muscles), the third digit flexes but is weak, while the fourth and fifth digits flex normally, which is called a Benedictine sign (or orator’s hand) (Fig. 1-18). This sign of median nerve palsy is so named because of its similarity to the hand position during blessings, and is seen in many portraits of Jesus.
When examining a complete median nerve palsy, the following pitfalls must be considered. The brachioradialis (radial innervated), with the help of gravity, may pronate the forearm from full supination. You may be tricked into observing thumb opposition by the indirect actions of the flexor pollicis brevis (deep head) and the adductor pollicis (both ulnar innervated). Lastly, palmar abduction of the thumb may be falsely mimicked by the flexor pollicis brevis (deep head), or truly moved in radial abduction by the abductor pollicis longus (radial innervated).

Figure 1-18 Benedictine sign. When a patient with a complete median palsy is asked to make a fist, the first digit barely flexes, the second digit partially flexes (secondary to substitution from non-median innervated muscles), the third digit flexes but is weak, while the fourth and fifth digits flex normally, creating what is known as the Benedictine sign.
Supracondylar Spur/Ligament of Struthers
Approximately 1% of people have a supracondylar spur on the medial side of the humerus about 5 cm proximal to the medial epicondyle. When this accessory condyle is present, it is thought that in most cases a ligament bridging it to the medial epicondyle is present. This ligament is called the ligament of Struthers after the anatomist who first described the supracondylar spur. When present, the median nerve usually passes underneath this ligament with either the brachial artery or its ulnar branch. This anatomically confined channel can cause median nerve entrapment in some patients (Fig. 1-19).
Clinically, this entrapment has been reported to cause insidious onset of forearm and hand weakness, with variable sensory loss in a median distribution. A deep aching pain is often present in the proximal forearm, which occasionally worsens with repetitive pronation/supination, or strength testing of the pronator teres or flexor carpi radialis. On examination, variable weakness, and even muscle wasting, may occur in any median nerve innervated muscle. Occasionally, the branches to the pronator teres arise proximal to the median nerve passing under the ligament of Struthers, and therefore, may be spared. Weakness of proximal forearm flexors, particularly the muscles innervated by the anterior interosseous nerve (ask the patient to make the okay sign), should be documented because this pattern of weakness frequently occurs in this entrapment (more below). A Tinel’s sign in the distal, medial upper arm may be present. Of course, palpation or a radiograph confirming the presence of a supracondylar spur is also required to make this diagnosis.
Supracondylar Fractures
Supracondylar fractures usually occur in children, and may cause median nerve damage. This is especially true for displaced fractures. Delayed median palsies can also occur secondary to progressive callus formation. As mentioned for ligament of Struthers entrapment of the median nerve, supracondylar injuries often involve axons destined for the anterior interosseous nerve. This occurs for two reasons. First, the relatively fixed anterior interosseous nerve is placed on stretch when a fractured arm is displaced posteriorly. Second, the nerve fibers destined to the anterior interosseous nerve, along with the sensory fibers destined for the first two digits, are located posteriorly in the median nerve, and are prone to injury as it passes through the supracondylar region. When a patient has isolated anterior interosseous motor loss secondary to partial median nerve damage in the supracondylar region (not to the anterior interosseous branch), it is indicative of pseudo-anterior interosseous neuropathy. This more proximal damage also causes thumb and index finger numbness, which helps differentiate this injury from a true anterior interosseous neuropathy.
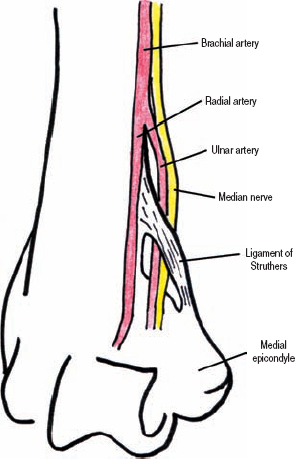
Figure 1-19 Ligament of Struthers. Approximately 1% of people have a supracondylar spur on the medial side of the humerus about 5 cm proximal to the medial epicondyle. When this accessory condyle is present, in most cases a ligament bridging this supracondylar spur to the medial epicondyle is present.
The Forearm
Musculotendinous Median Neuropathies
The bicipital aponeurosis, which crosses from lateral to medial over the antecubital fossa and serves to attach indirectly the biceps brachii tendon to the ulna, may irritate the median nerve. The pathogenesis of this is uncertain, but a thickened aponeurosis, hypertrophied brachialis (which lies under the median nerve and theoretically can push it superficially into the aponeurosis), or an anomalous muscle insertion of the pronator teres (which alters the local anatomic arrangements), may each predispose to this type of compression. Patients with bicipital aponeurosis entrapment have a similar presentation and exam to those with ligament of Struthers compression. They frequently report elbow pain radiating both proximally and distally. Occasionally, resisted forearm flexion in the supinated position for 30 seconds may precipitate symptoms. Of note, this compression is very rare.
The median nerve may be compressed or pinched where it passes between the two heads of the pronator teres (Fig. 1-20). This occurs most commonly in people who perform repetitive, forceful pronation of their forearm; it is called pronator teres syndrome. The only median-innervated muscle that cannot be affected by this syndrome is the pronator teres because branches from the median nerve destined for this muscle originate proximal to where the median nerve passes under this muscle. Pronator teres syndrome is characterized by an insidious onset of dull aching pain in the proximal forearm that is worsened by repetitive or forceful pronation. In fact, the most common finding is tenderness of the pronator teres to palpation. Median innervated hand sensation is often normal, and motor function may be difficult to ascertain because of pain. Nonetheless, weakness is occasionally seen during flexion of the second and third digits. A Tinel’s sign can often be elicited at the antecubital fossa. In contradistinction to carpal tunnel syndrome, patients usually do not complain of nocturnal pain and/or numbness. The true incidence of this syndrome is unknown, and some authors suggest it should be separated into those with objective findings versus those without.
A fibrotic arch between the two heads of the flexor digitorum superficialis may also irritate the median nerve (Fig. 1-20). This ridge has been called the sublimis arch, and may compress the median nerve as it passes underneath. Clinical manifestation of this entrapment is quite similar to pronator teres syndrome, except that forceful flexion of the proximal interphalangeal joints of the second to fifth digits, which is mediated by contraction of the flexor digitorum superficialis muscle, may precipitate symptoms.
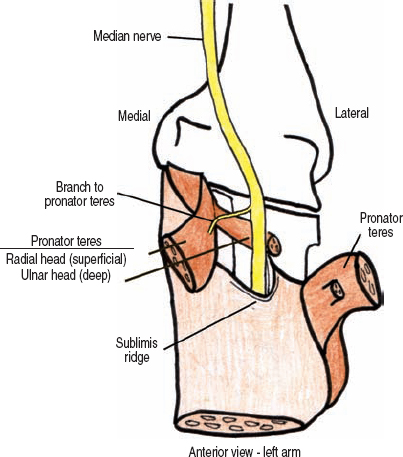
Figure 1-20 Pronator teres syndrome and sublimis arch. The median nerve may be compressed or pinched where it passes between the two heads of the pronator teres. A fibrotic arch may alternatively compress it when it passes under the two heads of the flexor digitorum superficialis.
Of note, with surgical treatment of median nerve entrapment at the elbow, all three possible compression points–bicipital aponeurosis, pronator teres, and sublimis arch–are each inspected and decompressed.
The Anterior Interosseous Nerve
An isolated palsy affecting the anterior interosseous nerve may occur secondary to trauma, fractures, Parsonage–Turner syndrome, anomalous muscles and/or tendons, or without known cause. Patients usually complain of weakness or clumsiness in grasping objects with their first two fingers (e.g., grasping the handle of a coffee cup). There are usually no complaints of pain, and because this nerve does not carry cutaneous sensation, no numbness occurs. Weakness of the flexor digitorum profundus (to the second and third digits), flexor pollicis longus, and pronator quadratus is present. Patients have a positive okay sign (Fig. 1-11). To confirm pure, anterior interosseous nerve palsy, all other median nerve innervated muscles, as well as sensation, must be normal. Partial anterior interosseous palsies are possible, as are partial median nerve palsies mimicking an anterior interosseus nerve deficit (pseudo-anterior interosseous neuropathy). Although anterior interosseous nerve palsy is a clinical diagnosis, magnetic resonance imaging (MRI) would show denervation of the three muscles innervated by this nerve.
 Patients with rheumatoid arthritis can have spontaneous and painless rupture of the flexor digitorum profundus and flexor pollicis longus tendons, mimicking an anterior interosseous palsy. To exclude this possibility, have the patient open and relax the hand. If the tendons are intact, pressing your thumb firmly across the ventral aspect of the forearm about 2 to 3 inches proximal to the wrist should cause passive finger flexion.
Patients with rheumatoid arthritis can have spontaneous and painless rupture of the flexor digitorum profundus and flexor pollicis longus tendons, mimicking an anterior interosseous palsy. To exclude this possibility, have the patient open and relax the hand. If the tendons are intact, pressing your thumb firmly across the ventral aspect of the forearm about 2 to 3 inches proximal to the wrist should cause passive finger flexion.
Carpal Tunnel Syndrome
The symptoms of carpal tunnel syndrome are well described: aching pain and paresthesias in the radial half of the palm and first three digits that wakes the patient up at night, and is relieved by “shaking it away.” Of course, each patient’s presentation is a variation of this central theme; perhaps it is only in the fingers, maybe they “don’t shake it away,” maybe it is only paresthesias or coldness, etc. On examination, hypesthesia, hyperesthesia, and/or diminished vibratory sense may be present in the first three digits. Remember, the majority of the median innervated palm region is via the palmar cutaneous branch, which does not pass through the carpal tunnel. Therefore, objective sensory testing on the thenar eminence is often normal; however, patients still commonly report pain and “abnormal” sensation in this area. In severe cases, thenar muscle wasting can be seen, as well as weakness in thumb opposition, flexion, and palmar abduction. Rarely, the thenar motor branch is selectively compressed. Other tests include a Tinel’s sign at the wrist, and the Phalen’s test and/or reverse Phalen’s test. A positive Phalen’s test is when flexing the affected wrist for about one minute precipitates symptoms. The reverse Phalen’s test is when extending the wrist does the same. Dr. Phalen, of note, was a pioneer in the field of carpal tunnel diagnosis and surgical treatment.
The etiology of carpal tunnel syndrome is uncertain. Space-occupying lesions in this passage obviously may predispose one to this syndrome (e.g., ganglion cysts, anomalous lumbrical muscles, fractures, etc.). Certain systemic diseases are also associated with entrapment here, including diabetes, chronic dialysis treatment, rheumatoid arthritis, acromegaly, obesity, and hypothyroidism, to name a few. A genetic predisposition to carpal tunnel syndrome (familial carpal tunnel syndrome) has been reported; these patients are thought to have a small carpal tunnel and/or a thickened transverse carpal ligament.
As with other more common compression syndromes, the clinical situation may worsen or improve over time, rapidly or slowly. A simple grading system separating carpal tunnel syndrome into mild, moderate, and severe is useful for treatment decision-making and prognosis. Mild carpal tunnel syndrome includes complaints of numbness and tingling at night, and occasionally during the day. The most common area involved is the long finger followed by the palm. A significant portion of the day the patient’s hand feels near normal. Pain is uncommon at this early stage. Two-point discrimination is usually okay, although vibration sense and light touch may actually be heightened in the affected fingers. No weakness or atrophy is present. In moderate carpal tunnel syndrome, the symptoms are more pervasive throughout the day. Sensory testing now reveals hypesthesia to light touch and vibration. Two-point discrimination may be abnormal. A Tinel’s sign is now present at the wrist, and a positive Phalen’s test may occur. Muscle weakness is still not present. In severe carpal tunnel syndrome, the patient’s symptoms are constant, weakness and atrophy may occur, and a Tinel’s sign at this point may even be absent secondary to extensive nerve damage. To reiterate, mild carpal tunnel syndrome is a diagnosis of medical history, with physical findings not usually present; moderate cases have sensory abnormalities and likely a Tinel’s sign; and severe cases have constant sensory symptoms and perhaps motor weakness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




