6
The Diagnostic Anatomy of the Sciatic Nerve
The sciatic nerve is the largest peripheral nerve in the body, and the lifeline to the lower extremities. It’s sensory and motor function are so important that in the absence of proper medical care, severe, proximal sciatic nerve lesions can actually lead to limb amputation secondary to recurrent trauma and infection. Fortunately, with contemporary management of sciatic injuries this is not the rule; many patients recover some motor function, as well as enough protective sensation to ambulate and return to work.
Overall, the sciatic nerve mediates knee flexion and all motor function below the knee. The tibial half of the sciatic nerve controls plantar foot flexion, inversion, and the foot intrinsic muscles; the common peroneal portion controls foot dorsiflexion and eversion. Although both the tibial and common peroneal nerves carry sensation from large areas of the leg and foot, the sensation from the sole of the foot is by far the most important, which is carried by the tibial nerve.
 Anatomical Course
Anatomical Course
The Buttock
The sciatic nerve is the main product of the sacral plexus, being made up of fibers from the L4, L5, S1, S2, and S3 spinal nerves. After formation, the sciatic nerve exits the pelvis via the greater sciatic foramen inferior to the pyriformis muscle. The pyriformis muscle originates on the lateral intrapelvic surface of the sacrum and inserts on the most superior tip of the femur’s greater trochanter. This muscle has a triangular shape, with its base on the sacrum and its apex on the trochanter.
After exiting the pelvis, the sciatic nerve runs distally toward the midline of the thigh, underneath the gluteus maximus, and over a bed of five successive muscles that run perpendicular to its course. In sequence, they are the following: superior gemelli, obturator internus, inferior gemelli, quadratus femoris, and the adductor magnus. The sciatic nerve remains posterior (dorsal) to the adductor magnus as it courses down the thigh (Fig. 6-1). The first three muscles (superior gemelli, obturator internus, and inferior gemelli) form a group and attach to the greater trochanter. The quadratus femoris inserts into the lesser trochanter; the adductor magnus has a long insertion on the shaft of the femur.
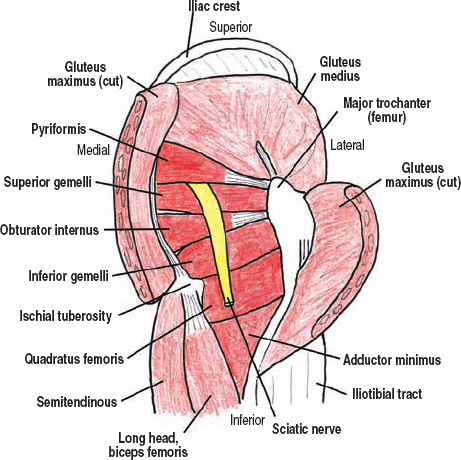
Figure 6-1 The muscular anatomy of the piriformis and deep buttock muscles. After formation, the sciatic nerve exits the pelvis via the greater sciatic foramen inferior to the pyriformis muscle. After leaving the pelvis, the sciatic nerve then runs distally toward the midline of the thigh, underneath the gluteus maximus and over a bed of five successive muscles that run perpendicular to its course.
The sciatic nerve is actually two nerves, the tibial and common peroneal, which are joined by a common epineurium from the pelvis to the lower third of the thigh where these two components separate. The tibial nerve is medial and larger, being composed of fibers from L4 through S3. The common peroneal nerve is lateral and smaller, and is composed of fibers from fewer spinal nerves, specifically L4-S2, with a large contribution from the lumbosacral trunk. Before forming the sciatic nerve, the ventral rami of these spinal nerves split into anterior and posterior divisions, with the tibial nerve being composed of the anterior divisions and the common peroneal by the posterior divisions. This orientation is opposite than expected because the tibial nerve innervates posterior compartment muscles, whereas the common peroneal nerve innervates anterior compartment ones. The sciatic nerve is protected by the large gluteus maximus, as well as by the ischial tuberosity when one sits.
Also exiting the pelvis through the greater sciatic notch under the pyriformis muscle, but medial to the sciatic nerve, are the posterior cutaneous nerve to the thigh (the lesser sciatic nerve), the inferior gluteal nerve and vessels, and most medially, the pudendal nerve and vessels. The superior gluteal nerve exits the greater sciatic foramen superior to the pyriformis. These nerves are discussed in the lumbosacral plexus section.
 The sciatic nerve may also pass superior to, or even through, the pyriformis muscle when exiting the sciatic notch. The S3 contribution to the sciatic nerve is variable. Alternatively, the sciatic nerve sometimes contains fibers from S4.
The sciatic nerve may also pass superior to, or even through, the pyriformis muscle when exiting the sciatic notch. The S3 contribution to the sciatic nerve is variable. Alternatively, the sciatic nerve sometimes contains fibers from S4.
The Thigh and Knee
The sciatic nerve runs down the midline of the posterior thigh toward the popliteal fossa. It runs superficial, or dorsal, to the adductor magnus, but underneath the hamstring muscles. There are four hamstring muscles, two medial and two lateral. The lateral pair are the long and short heads of the biceps femoris. The long head of the biceps femoris originates from the ischial tuberosity; the short head originates from the shaft of the femur. Together, both heads insert distally into the fibular head. The long head of the biceps femoris crosses the midline of the thigh, similar to the arm of an “X,” from medial to lateral. The long head is superficial to the short head. The medial pair of hamstrings are the semitendinous and semimembranous muscles, both originating from the ischial tuberosity and remaining medial along the thigh to insert into the lateral tibia, along with the sartorius and gracilis tendons. The semitendinous is more superficial and medial. The sciatic nerve runs deep to the hamstrings, remaining mostly deep to the long head of the biceps femoris as this muscle runs medial to lateral. The sciatic nerve bifurcates into the tibial and common peroneal nerves approximately two thirds of the way down the thigh. Distally, like the archway of a door, both the medial and lateral groups of hamstrings part away from midline to expose the popliteal fossa.
The larger and more-medial tibial nerve (anterior divisions of L4 to S3) continues down the thigh and into the popliteal fossa while remaining midline. In the distal thigh, the tibial nerve joins the popliteal artery and vein. These vessels are the distal continuations of the femoral artery and vein, and enter the posterior compartment of the thigh by passing medial to the femur via the adductor hiatus. Viewing the popliteal fossa from posterior, the tibial nerve lies lateral to the popliteal vessels (Fig. 6-2). This neurovascular bundle runs deep into the leg (defined as the lower extremity between the knee and the ankle) by passing under the gastrocnemius and soleus muscles. Underneath these proximal calf muscles, the tibial nerve runs over or dorsal to the popliteal muscle, which creates the floor of the popliteal fossa by running transversely from the upper medial aspect of the tibia to the lower lateral femur.
Prior to entering the leg, the tibial nerve branches to the medial sural cutaneous nerve. This branch runs superficially along the midline between the two heads of the gastrocnemius muscle, eventually piercing the subcutaneous fascia just distal to this muscle. Upon piercing the fascia, the medial sural cutaneous nerve merges with the lateral sural cutaneous nerve (from the common peroneal nerve) to form the proper sural nerve. The sural nerve runs down the posterior leg, behind the lateral malleolus, and into the dorsolateral foot.
The common peroneal nerve (posterior divisions of L4-S2) runs obliquely from the apex of the popliteal fossa to the posterior fibular head (Fig. 6-2). In doing so, this nerve skirts along the medial margin of the biceps femoris muscle. In this region, the common peroneal nerve gives off two sensory branches, the lateral sural cutaneous (mentioned previously), which merges with the medial sural cutaneous (from the tibial nerve), and the lateral cutaneous nerve to the calf. Following these two branches, the common peroneal nerve passes lateral to the very proximal fibular shaft, underneath the peroneus longus muscle.
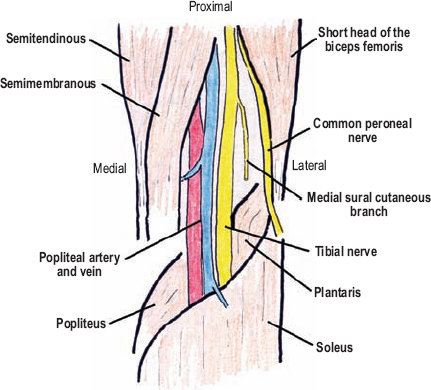
Figure 6-2 Popliteal fossa anatomy. Viewing the popliteal fossa from posterior, the tibial nerve lies lateral to the popliteal artery and vein. The common peroneal nerve skirts along the medial margin of the biceps femoris muscle, from the apex of the popliteal fossa to the fibular head.
The sural nerve is usually made up of both medial and lateral sural cutaneous nerves; however, in some patients the sural nerve is derived from only one of these two nerves, usually the medial one.
The Tibial Nerve
The Leg
The tibial nerve runs down the leg in a straight line from the middle of the popliteal fossa, to just posterior to the medial malleolus. This nerve runs deep to the gastrocnemius and soleus muscles, but remains superficial (dorsal) to the deep posterior compartment muscles. In the proximal leg, the tibial nerve runs on, or dorsal to, the tibialis posterior muscle. In the distal leg it runs in a cleft between the flexor digitorum longus medially, and the flexor hallucis longus laterally. The popliteal artery and vein continue with the tibial nerve in the leg, but are renamed the posterior tibial artery and vein. These vessels run on the nerve’s medial aspect, first over the tibialis posterior, then over the flexor digitorum longus.
Posterior to the medial malleolus, the tibial nerve enters the foot by running deep to the flexor retinaculum (lacinate ligament). The flexor retinaculum is a thin ligament that bridges the medial malleolus to the calcaneus, under which passes not only the tibial nerve, but also the posterior tibial artery and veins, and from anterior to posterior, the tendons of the tibialis posterior, flexor digitorum longus, and flexor hallucis longus. This subligamentous, anatomic passage into the foot is called the tarsal tunnel (Fig. 6-3).
Within, or just proximal, to the tarsal tunnel, the tibial nerve bifurcates into the medial and lateral plantar nerves. The tibial nerve also gives a sensory branch to the medial half of the heel just before, or from within, the tarsal tunnel. This branch is called the medial calcaneal nerve.
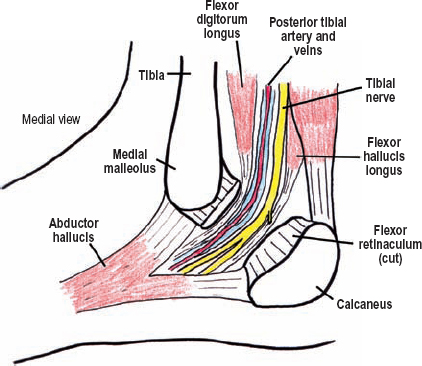
Figure 6-3 The tarsal tunnel. Posterior to the medial malleolus, the tibial nerve enters the foot by running deep to the flexor retinaculum. The flexor retinaculum is a ligamentous band from the medial malleolus to the calcaneus, under which passes not only the tibial nerve, but also the posterior tibial artery, veins, and multiple tendons.
The Foot
The medial plantar nerve is the larger of the two terminal divisions of the tibial nerve, and as its name implies, courses through the medial plantar region (Fig. 6-4). The medial plantar nerve runs between the abductor hallucis and the flexor digitorum brevis, the latter muscle being located in the midline of the sole. As the medial plantar nerve courses down the foot, it progressively bifurcates into digital nerves for the first three and a half toes. Sensory branches to the sole originate quite proximal, just after the medial plantar nerve enters the sole of the foot.
After traversing the tarsal tunnel, the lateral plantar nerve passes across the sole of the foot, deep to the flexor digitorum brevis. Once lateral, it runs anteriorly between the quadratus plantae medially and the abductor digiti minimi pedis laterally. The lateral plantar nerve divides into a superficial sensory and deep motor branch, analogous to the ulnar nerve in the hand. The superficial branch becomes subcutaneous and the deep branch remains deep to innervate the intrinsic foot musculature.
The Common Peroneal Nerve
The Deep Branch
The common peroneal nerve passes around the lateral aspect of the upper fibula, just distal to the fibular head, underneath the posterior fibrous edge of the peroneus longus muscle. Two ligamentous bands in this region form the so-called fibular tunnel: the peroneus longus muscle aponeurosis (deep) and an aponeurosis connecting the soleus and peroneal fascia (superficial). Under the peroneus longus, the common peroneal nerve bifurcates into a superficial and deep branch.
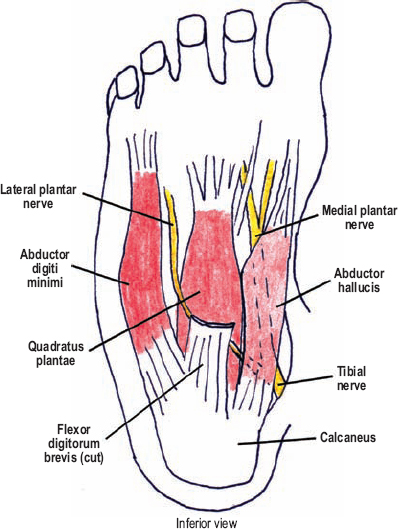
Figure 6-4 Muscle relationships of the plantar nerves in the sole of the foot. The medial plantar nerve runs between the abductor hallucis and the flexor digitorum brevis, the latter muscle being located in the midline of the sole. The lateral plantar nerve passes across the sole of the foot, deep to the flexor digitorum brevis. Once lateral, it runs anteriorly between the quadratus plantae medially and the abductor digiti minimi pedis laterally.
Anterior to the fibula, the deep peroneal nerve dives deep to the extensor digitorum longus muscle, where it joins the tibialis anterior artery to travel down the leg. This neurovascular bundle runs between the extensor digitorum longus anteriorly and the intermuscular septum/lateral tibia posteriorly. In the more distal aspect of the leg, the deep peroneal nerve shifts a little toward the midline, where it runs on the tibia under the tibialis anterior muscle. The deep peroneal nerve passes onto the dorsal aspect of the foot by running under two extensor retinaculums (superior and inferior), a confined anatomical space known as the anterior tarsal tunnel. Once on the dorsum of the foot, the deep peroneal nerve divides into medial and lateral branches. The medial branch passes distally with the dorsalis pedis artery, eventually terminating as a sensory branch to the first web space. The lateral branch innervates the extensor digitorum brevis.
The Superficial Branch
The superficial branch of the common peroneal nerve turns distally after passing around the fibula to run under the peroneus longus. It, however, remains superficial to the extensor digitorum longus. This latter muscle separates the superficial and deep branches of the peroneal nerve. The superficial branch emerges in the distal half of the leg, lateral to the formed tendon of the peroneus longus muscle and still superficial to the extensor digitorum longus. This nerve divides into two sensory branches proximal to the extensor retinaculum. Both of these branches run superficial to the extensor retinaculum; they are called the medial and intermediate, dorsal cutaneous nerves of the foot.
 Motor Innervation and Testing
Motor Innervation and Testing
The Buttock/Thigh Group
Immediately after exiting the pelvis, the sciatic nerve provides two common motor branches to innervate the hamstring muscles (Fig. 6-5). One branch originates from the tibial division; the second comes from the common peroneal division. These hamstring branches pass distally with the sciatic nerve in the buttock region. The sciatic nerve also gives supplementary branches to the hamstring muscles as it passes next to them in the more distal thigh, however, loss of these smaller branches, in general, may not be noticed clinically when the larger, proximal hamstring branches are preserved. Considering the proximal origin of the main hamstring branches, a sciatic nerve injury involving the hamstring muscles would have to be very proximal (e.g., the buttock region).
The tibial portion of the sciatic nerve innervates the medial hamstrings (the semitendinous and semimembranous), as well as the long head of the biceps femoris. The short head of the biceps femoris is the only hamstring innervated by the more lateral common peroneal portion of the sciatic nerve. The hamstrings (L5-S2) are tested with the patient seated, instructing him or her to flex the leg against resistance. The examiner should simultaneously palpate the hamstring tendons in the proximal popliteal fossa (Fig. 6-6). The hamstrings may also be tested with the patient prone. An isolated lesion affecting only the tibial half of the sciatic nerve spares the peroneal innervated short head of the biceps femoris. In this situation, a portion of the lateral hamstrings will continue to function, and its tendon can be palpated during thigh flexion.
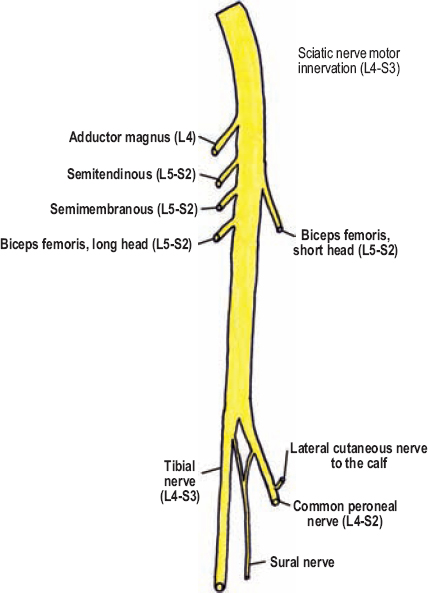
Figure 6-5 Motor innervation from the sciatic (schematic) nerve in the buttock and thigh.
The tibial portion of the sciatic nerve also innervates the ischial half of the adductor magnus (L4 of L2-L4). Test this muscle, along with the other thigh adductors (innervated by the obturator nerve), by having the patient bring the knees together under resistance, either seated (Fig. 6-7) or supine.

Figure 6-6 Hamstring (L5-S2) assessment: The hamstrings are tested with the patient seated. Instruct the patient to flex at the knee against resistance. The examiner should simultaneously palpate the hamstring tendons in the proximal popliteal fossa. The hamstrings may also be tested with the patient prone (lower image).

Figure 6-7 Thigh adduction (L2-L4) assessment: Test thigh adduction by having the patient bring the knees together against resistance, with the patient either seated or supine. (The sciatic nerve provides only L4 contribution; L2 and L3 contribution is carried by the obturator nerve.)
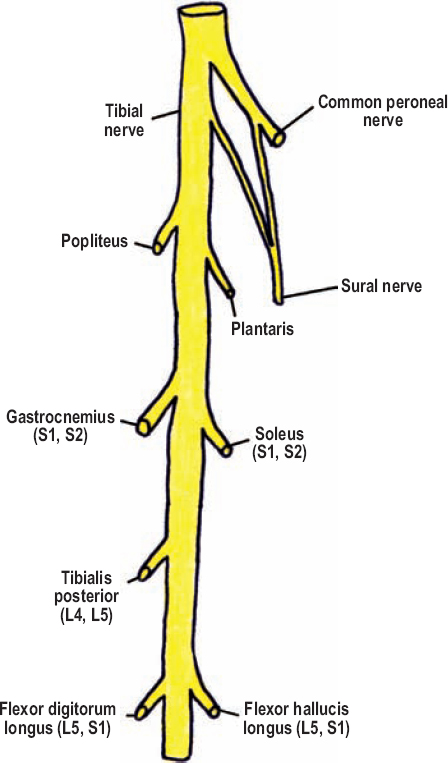
Figure 6-8 Motor innervation from the tibial nerve in the leg (L4-S2).
The Leg
The Tibial Nerve Group
The tibial nerve innervates the posterior compartment muscles of the leg, which control plantar flexion, foot inversion, and toe flexion (Fig. 6-8). Prior to passing deep to the gastrocnemius and soleus (S1, S2), the tibial nerve sends branches to these muscles. Therefore, damage to the tibial nerve deep to these muscles would spare their innervation. Although both the gastrocnemius (medial and lateral heads) and soleus muscles insert into the calcaneus, they have different origins. The gastrocnemius originates from the distal femur and therefore produces plantar flexion with the knee straight. In contrast, the soleus originates from the tibia and therefore can mediate plantar flexion with the knee straight or bent. Because the gastrocnemius is so powerful with the knee straight, soleus-mediated plantar flexion is only dominant when the knee is flexed. With the patient sitting, the gastrocnemius heads can be tested by extending the leg at the knee and having the patient plantar flex the foot against resistance (“pushing down on the gas pedal”)(Fig. 6-9). Gastrocnemius contraction should be palpated. The soleus is tested in near-isolation (gastrocnemius function can never be eliminated) by instructing the patient to go up on his or her toes while seated with the knees flexed (Fig. 6-10). To observe subtle plantar flexion weakness, the patient should attempt to stand on his or her toes, one foot at a time.
Immediately deep to the soleus, the tibial nerve innervates the tibialis posterior (L4, L5). This muscle is the prime inverter of the foot, with its tendon inserting into the tarsal bones both on the medial aspect of the foot, as well as on the lateral aspect, that is after passing underneath the foot. Test the tibialis posterior by having the patient invert the foot against resistance (Fig. 6-11). Toes flexors should remain relaxed to avoid substitution. Alternatively, the patient can place the soles of his or her feet together while in a sitting position.

Figure 6-9 Gastrocnemius (S1, S2) assessment: With the patient sitting, the gastrocnemius heads are tested by having the patient plantar flex the foot against resistance with the knee straight. The examiner’s other hand stabilizes the leg and palpates gastrocnemius contraction. To observe subtle plantar flexion weakness, the patient should attempt to stand on his or her toes, one foot at a time, or even walk on the toes.

Figure 6-10 Soleus (S1, S2) assessment: The soleus is tested in near-isolation by instructing the patient to go up on his or her toes while seated, with resistance placed on the knee tops.
In the posterior leg compartment, the tibial nerve also innervates the flexor digitorum longus and flexor hallucis longus (L5, S1). Tendons from these muscles insert into the most distal phalanges of the toes, and thereby mediate flexion in all the joints they cross. To assess these muscles (along with the similar acting flexor digitorum brevis), one instructs the patient to curl the toes against resistance. Resistance is applied by grasping the foot with both hands, using the fingers to hold the dorsum of the foot while both thumbs force the toes back into extension (Fig. 6-12). The flexor hallucis longus acts on the great toe while the flexor digitorum longus inserts into the rest.
 Together, the long toe flexors, peroneus muscles, and tibialis posterior can substitute for plantar flexion. This substitution, however, mostly flexes the forefoot, not necessarily the ankle. In the distal popliteal fossa, the tibial nerve innervates the popliteus and plantaris muscles. These two muscles have minimal clinical significance.
Together, the long toe flexors, peroneus muscles, and tibialis posterior can substitute for plantar flexion. This substitution, however, mostly flexes the forefoot, not necessarily the ankle. In the distal popliteal fossa, the tibial nerve innervates the popliteus and plantaris muscles. These two muscles have minimal clinical significance.
The Deep Peroneal Nerve Group
The deep peroneal nerve innervates all anterior compartment leg muscles, excluding the peroneus longus and brevis, which are innervated by the superficial peroneal nerve (Fig. 6-13). Immediately after passing deep to the extensor digitorum longus, the deep peroneal nerve gives a motor branch to the tibialis anterior (L4-S1), which is the prime dorsiflexor of the foot. Weakness of the tibialis anterior, with sparing of the peroneus muscles, indicates an injury to the deep peroneal nerve near its origin at the fibula. Contraction of the tibialis anterior can be seen and palpated during muscle testing (Fig. 6-14). The toes should remain relaxed, because contraction of the toes extensors can substitute for foot dorsiflexion.
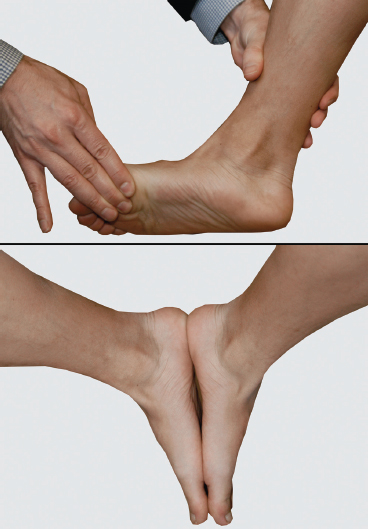
Figure 6-11 Tibialis posterior (L4, L5) assessment: The tibialis posterior is tested with the patient inverting the foot against resistance. Toes flexors should remain relaxed to avoid substitution. Alternatively, the patient can place the soles of the feet together while in a sitting position (lower image).
The deep peroneal nerve innervates the extensor digitorum longus (L5, S1) and extensor hallucis longus (L5). Tendons from these muscles insert into the distal phalanges and are tested by having the patient extend the toes against resistance (Figs. 6-15 and 6-16). Upon contraction, the extensor hallucis longus tendon should readily bowstring proximal to the great toe.

Figure 6-12 Flexors digitorum longus, flexor hallucis longus (both L5, S1), and flexor digitorum brevis (S1, S2) assessment: To assess toe flexion, instruct the patient to curl the toes against resistance. Alternatively, resistance can be applied by grasping the foot with both hands, using the fingers to hold the dorsum of the foot and both thumbs to force the toes back into extension (lower image).
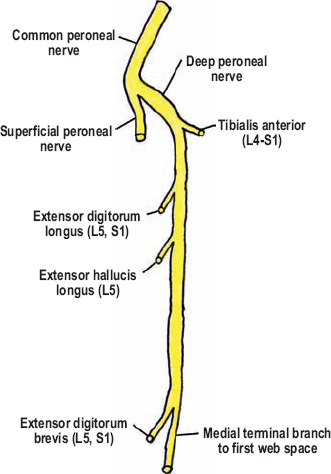
Figure 6-13 Motor innervation from the deep peroneal nerve (L4-S1).

Figure 6-14 Tibialis anterior (L4-S1) assessment: Contraction of this muscle can be seen during foot dorsiflexion. The toes should remain relaxed because the toe extensors may substitute for foot dorsiflexion.

Figure 6-15 Extensor digitorum longus (L5, S1) assessment: Have the patient extend the toes, with or without resistance.

Figure 6-16 Extensor hallucis longus (L5) assessment: Have the patient extend the great toe against resistance. The tendon (arrow) should readily bowstring proximal to the great toe upon contraction.
 The motor branch destined for the extensor hallucis longus passes for a significant distance adjacent to the fibular shaft, and therefore may be selectively injured with fractures and/or surgical procedures in this area.
The motor branch destined for the extensor hallucis longus passes for a significant distance adjacent to the fibular shaft, and therefore may be selectively injured with fractures and/or surgical procedures in this area.
The Superficial Peroneal Nerve Group
The superficial peroneal nerve mediates foot eversion by innervating the peroneus longus and brevis (L5, S1) in the lateral aspect (compartment) of the leg (Fig. 6-17). Both of these muscles originate from the fibula, and insert into the foot after passing around the posterior aspect of the lateral malleolus. The peroneus brevis simply inserts into the undersurface of the fifth metatarsal. The peroneus longus, however, mirroring the tibialis posterior, loops around the undersurface of the foot to insert into the proximal portion of the first metatarsal. The peroneus muscles are evaluated by having the patient evert the foot against resistance (Fig. 6-18). Contraction of these muscles can be observed and palpated. The peroneus brevis tendon bowstrings the skin between the lateral malleolus and its insertion into the fifth metatarsal head.
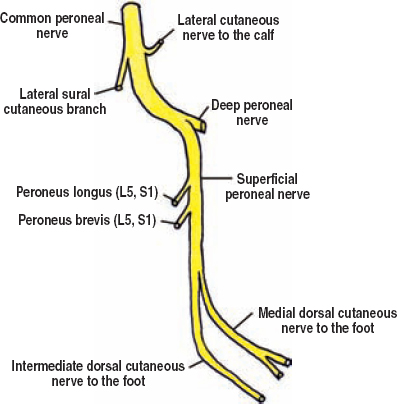
Figure 6-17 Motor innervation of the superficial peroneal nerve (L5-S1).
 Although not present in most people, a lateral extension of the extensor digitorum longus, called the peroneus tertius, may be present. This muscle is innervated by the superficial peroneal nerve (not the deep peroneal nerve that innervates the extensor digitorum longus), and inserts into the fifth metatarsal, mediating “extension” of the foot’s lateral aspect.
Although not present in most people, a lateral extension of the extensor digitorum longus, called the peroneus tertius, may be present. This muscle is innervated by the superficial peroneal nerve (not the deep peroneal nerve that innervates the extensor digitorum longus), and inserts into the fifth metatarsal, mediating “extension” of the foot’s lateral aspect.

Figure 6-18 Peroneus longus and brevis (L5, S1) assessment: The peroneus muscles are evaluated by having the patient evert the foot against resistance. Contraction of these muscles can be observed and palpated. The tendon (arrow) of the peroneus brevis can be observed bow-stringing the skin between the lateral malleolus and its insertion into the fifth metatarsal head.
The Foot
The Medial Plantar Nerve Group
Upon passing between the abductor hallucis and flexor digitorum brevis (S1, S2), the medial plantar nerve innervates these two muscles (Fig. 6-19). The tendons of the flexor digitorum brevis insert into the proximal phalanges of the second through fifth toes, and mediate flexion at the metatarsal-phalangeal joints. More distally, the medial plantar nerve also innervates the flexor hallucis brevis (S1, S2), which likewise flexes the metatarsal-phalangeal joint of the great toe. These muscles are difficult to isolate on examination; however, composite toe flexion can be tested (Fig. 6-20). When the patient curls the arch of the foot medially, the abductor hallucis usually contracts well enough to be tested. When denervated, atrophy of the abductor hallucis may be seen. In contrast, wasting of the flexor digitorum brevis is usually not noticeable because of the thick sole and plantar aponeurosis covering it. The medial plantar nerve also commonly innervates the first lumbrical (L5, S1) of the foot.
The Lateral Plantar Nerve Group
The lateral plantar nerve and its deep branch innervate most of the intrinsic muscles of the foot, analogous to the ulnar nerve in the hand (Fig. 6-19). These muscles include the quadratus plantae, abductor digiti minimi pedis, second to fourth lumbricals all the dorsal interossei, and both heads of the adductor hallucis (all via S1-S3). Foot intrinsic muscles innervated by other nerves include the abductor hallucis, flexor digitorum brevis, and flexor hallucis brevis (medial plantar nerve), as well as two muscles on the dorsum of the foot, the extensors digitorum and hallucis brevis (deep peroneal nerve, see below). One may grossly assess intrinsic motor function by instructing the patient to “cup” the foot (Fig. 6-20). Action of the individual foot intrinsic muscles cannot be readily isolated on physical examination. Chronic, severe intrinsic foot muscle weakness can cause clawing of the toes.
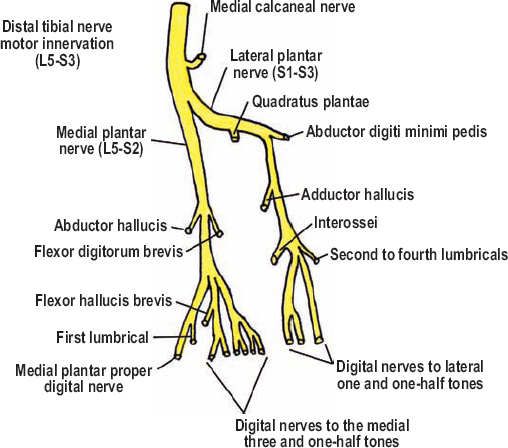
Figure 6-19 Motor innervation from the plantar nerves in the sole of the foot.

Figure 6-20 Cupping of the sole (S1-S3): Grossly assess intrinsic motor function by instructing the patient to “cup” the foot. Alternatively, you can have him or her spread the toes; however, some patients with normal motor function are not able to do this. Action of the individual foot intrinsic muscles cannot be easily isolated on physical examination.
The Deep Peroneal Nerve Group
The lateral terminal branch of the deep peroneal nerve in the dorsum of the foot innervates the extensor digitorum brevis (L5, S1). This muscle extends the toes at the metatarsal-phalangeal joint, a movement that is hard to isolate from the extensors digitorum and hallucis longus. The best way to determine paralysis of the extensor digitorum brevis is to observe and palpate its contraction during composite toe extension (Fig. 6-21).
 The Accessory Peroneal Nerve
The Accessory Peroneal Nerve
The accessory peroneal nerve is a distal branch of the superficial peroneal nerve that is present in approximately 20% of people. This branch carries motor innervation to the extensor digitorum brevis, a muscle that is usually controlled by the deep peroneal nerve. When evaluating electrophysiological and clinical examination results, one should keep this potential transfer of motor innervation in mind when localizing the lesion.

Figure 6-21 Extensor digitorum brevis (L5, S1) assessment: The best way to determine paralysis of the extensor digitorum brevis is to observe and palpate its contraction during toe extension (arrow).
 The accessory peroneal nerve may occasionally branch from the deep peroneal nerve.
The accessory peroneal nerve may occasionally branch from the deep peroneal nerve.
 Sensory Innervation
Sensory Innervation
The sural nerve provides sensory coverage to the lower lateral leg, some lateral heel and ankle, and the dorsolateral aspect of the foot, especially its lateral margin (Fig. 6-22). Because of overlap in sensory coverage of the leg and foot, damage to the sural nerve (e.g., following an excisional biopsy) usually only manifests as numbness along the lateral border of the foot. With time, however, this area of numbness shrinks as the neighboring sensory nerves branch to cover the loss. The sural nerve is composed of two communicating branches, one from the tibial nerve and the other from the common peroneal nerve. The tibial nerve gives the medial sural cutaneous nerve in the popliteal fossa, whose distal continuation becomes the sural nerve proper. The common peroneal nerve in the popliteal fossa yields two sensory branches, the lateral sural cutaneous and lateral cutaneous nerve to the calf. The first of which, as the name implies, carries fibers destined for the sural nerve. The medial and lateral sural cutaneous nerves merge just below the two heads of the gastrocnemius muscle either before or after the medial sural cutaneous nerve pierces the fascia to become subcutaneous.
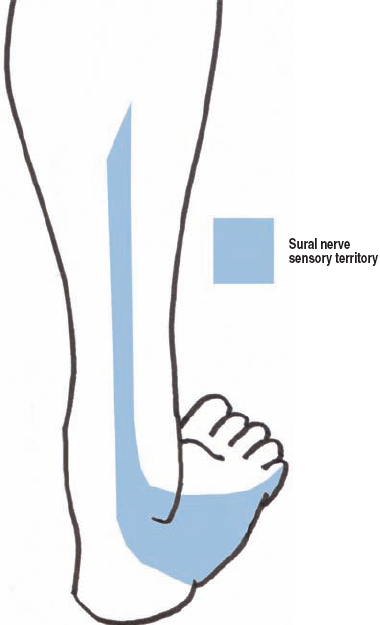
Figure 6-22 The Sural nerve. This nerve provides sensory coverage to the lower lateral leg, some lateral heel and ankle, and the dorsolateral aspect of the foot, especially its lateral margin. Because of overlap in the sensory coverage of the leg and foot, sural nerve damage (e.g., following an excisional biopsy) usually only manifests as numbness along the lateral border of the foot.
The lateral cutaneous nerve to the calf provides sensory coverage of the lateral knee and calf (i.e., the upper lateral aspect of the leg). The remaining lower lateral portion of the leg is covered by either the sural nerve, the lateral sural cutaneous branch, or cutaneous branches off the superficial peroneal nerve. The lateral cutaneous nerve to the calf does not have a consistent autonomous region to test.
Together, the deep and superficial peroneal nerves provide sensation to the dorsum of the foot and anterolateral shin (Fig. 6-23). The superficial peroneal nerve carries the majority of this sensation, except for a small area of skin centered on the web space between the first and second toes, which the deep peroneal nerve covers.
The tibial division of the sciatic nerve carries the most important sensation of the lower extremity, that for the sole of the foot (Fig. 6-24). With numbness in the sole of the foot, minor trauma, or unrecognized, persistent pressure, may cause ulcers, infection, and even amputation. Furthermore, dysesthesias in this region may prevent ambulation and be very problematic. The tibial nerve’s coverage of the foot’s plantar aspect is divided into three zones. The medial calcaneal nerve exits the tibial nerve just prior, or within, the tarsal tunnel, and innervates the medial half of the heel. The medial and lateral plantar nerves provide sensory branches to the medial and lateral sole, respectively. The medial plantar nerve covers a bit more area, including the first three and one-half toes, and the lateral plantar nerve covers the lateral one and a half toes. The plantar nerve’s sensory coverage includes the nails and the skin surrounding the nails on the toes’ dorsal surfaces. A branch of the sural nerve covers sensation on the lateral heel, although this may be inconsistent.
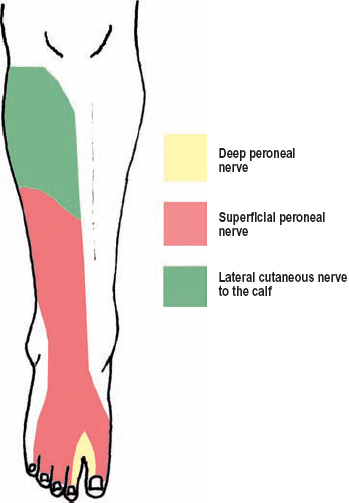
Figure 6-23 Peroneal division sensory territory. Together, the deep and superficial peroneal nerves provide sensation to the dorsum of the foot and anterolateral shin. The superficial peroneal nerve carries the majority of this sensation, except for a small area of skin centered on the web space between the first and second toes, which the deep peroneal nerve controls. The lateral cutaneous nerve to the calf is a branch of the common peroneal nerve prior to its bifurcation.
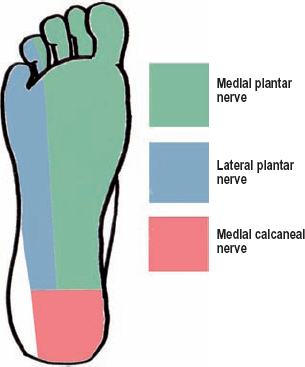
Figure 6-24 Tibial division sensory territory. Three branches from the tibial nerve cover the foot’s plantar aspect. The medial calcaneal nerve exits the tibial nerve just prior, or within, the tarsal tunnel, and innervates the medial half of the heel. The medial and lateral plantar nerves provide sensory branches to the medial and lateral sole, respectively.
 Clinical Findings and Syndromes
Clinical Findings and Syndromes
The Buttock
Trauma, Fractures, and Injections
A complete sciatic nerve lesion is a severe deficit. Sensation to the lateral aspect of the leg and nearly all of the foot is lost. The only sensation remaining in the foot is near the medial malleolus, which is carried by the saphenous nerve. Sensory loss, as mentioned earlier in this chapter, is probably the most dangerous aspect of a severe sciatic nerve palsy. Proper shoes and daily foot checks by the patient are mandatory until enough protective sensation of the sole and foot is recovered. Regarding motor control, all foot and ankle movements are lost, which may preclude useful ambulation without the use of orthotics. Loss of leg flexion at the knee can also occur for complete, proximal sciatic nerve palsies. Hamstring weakness, however, is uncommon because the major branches to these muscles originate from the sciatic nerve quite proximally, sometimes at or within the sciatic notch. For this reason, most sciatic nerve palsies actually spare leg flexion at the knee.
Care must be taken when attempting to differentiate a sciatic nerve injury from an S1 radiculopathy or sacral plexus injury. Making this differentiation is often not possible using only the neurological examination. An S1 radiculopathy frequently involves the gluteal nerves, whereas a sciatic nerve palsy would not. However, depending on the type of injury, the gluteal and sciatic nerves may both be compromised at the sciatic notch. With sacral plexus lesions, the gluteal nerves, pudendal nerve, and posterior cutaneous nerve to the thigh may be affected. Once again, however, a sciatic notch injury may simultaneously involve all of these nerves where they exit the pelvis. The pudendal nerve is the furthest away from the sciatic nerve in the buttock; therefore, a deficit in this nerve may be the strongest evidence on examination of a sacral lesion. For sacral plexus injury patients, imaging and electrophysiological studies are usually required.
One common cause of a buttock-level sciatic lesion is an injection injury. The safest way to administer a buttock injection is to have the patient lie prone, and then place the injection in the upper outer quadrant. Standing bent over a sink or table, or rolling over in bed is not acceptable because the topographical anatomy of the buttock becomes distorted, especially in the elderly, who have reduced amounts of subcutaneous adipose tissue and sagging buttocks. The most dangerous injection quadrant is the superomedial one. Injections injuries are readily diagnosed, considering sciatic pain and deficits characteristically begin immediately after the offending injection. Occasionally, injection injuries can present minutes to hours after an injection; the cause of this delay is uncertain. Some believe it is irritation of the nerve by the offending substance being injected in or near the epineurium. Sciatic nerve injection injuries can cause severe motor and sensory deficits, or more commonly, a mild neurological deficit with persistent sciatica.
Other causes of buttock-level sciatic lesions include hip fractures and orthopedic procedures. This is because the sciatic nerve runs just dorsal to the hip joint, and is only separated from it by a few thin muscles. It is vulnerable to hematomas, adjacent hardware, intraoperative retraction or coagulation, and fracture/dislocations. Of note, when isolated hip fractures injure a peripheral nerve they usually only affect the sciatic nerve. In contrast, pelvic and sacral fractures often involve the sacral plexus. Penetrating trauma can also damage the sciatic nerve in the buttock region, but this is uncommon because the nerve is deep below the gluteus maximus.
Piriformis Syndrome
As described previously, upon exiting the pelvis, the sciatic nerve passes under the pyriformis muscle, which runs from the inner lateral margin of the sacrum to the greater trochanter of the femur (Fig. 6-1). Occasionally, the sciatic nerve runs over, or through, the pyriformis muscle. Definitive confirmation that pyriformis syndrome is a true clinical entity is pending, with many experts doubting its occurrence. Others have suggested pyriformis syndrome be categorized as neurogenic (with objective clinical findings) or non-neurogenic (without objective clinical findings). Patients with pyriformis syndrome have buttock and sciatic nerve distribution pain, usually without objective weakness or sensory loss on examination. Electrodiagnostic testing is usually normal. Many of these patients are originally thought to have lumbar disc herniations; either a normal lumbar spine magnetic resonance image (MRI) scan or failed spine surgery leads to the diagnosis of pyriformis syndrome. A steroid injection into the pyriformis muscle may help ascertain the diagnosis, but is not without risk. Pyriformis syndrome patients can have a history of a short fall and landing on their buttocks. If the patient is a woman and her symptoms are cyclical, one should consider focal nerve compression near the sciatic notch from endometriosis.
The Thigh
Complete and Partial Lesions
Injuries to the sciatic nerve in the thigh region are usually caused by gun shot wounds, and less commonly by lacerations. Femur fractures and/or repairs may also damage the sciatic nerve. Because the main branches to the hamstrings originate in the buttock region, even complete thigh-level sciatic lesions spare leg flexion. Although the tibial and peroneal divisions of the sciatic nerve do not split from one another until the lower third of the thigh, even upper thigh and buttock lesions may predominantly, or solely, involve just one of these divisions. This is because the tibial and peroneal divisions remain separate, even though they share a common epineurium as the sciatic nerve.
Compared with the tibial division, the peroneal division is more susceptible to injury. It is more commonly injured; the degree of injury is characteristically more severe; and recovery is less likely to occur. There are at least six potential reasons for this: (1) the peroneal division lies lateral and more superficial in the buttock region, making it more susceptible to trauma, (2) it is fixed between two anatomical points, the sciatic notch and lateral fibular head, unlike the tibial nerve, which is only fixed at the sciatic notch, (3) it has less blood supply than the tibial division, (4) it has fewer and larger fascicles with less intervening connective tissue (less tensile strength), (5) peroneal-innervated muscles (e.g., peroneus longus and brevis) are themselves concurrently injured with leg trauma, and (6) the peroneal division innervates long, thin extensor muscles, which often require robust reinnervation prior to them functioning.
The Knee/Leg
Tibial Palsy
A tibial palsy manifests as plantar flexion (gastrocnemius, soleus), foot inversion (tibialis posterior), toes flexion (flexor digitorum and hallucis longus, flexor digitorum and hallucis brevis), and foot intrinsic muscle weakness. Sensory loss occurs in the sole of the foot and the medial heel. Depending on the tibial division’s contribution to the sural nerve, its sensory territory may also be affected. The most common causes of knee/leg tibial nerve injury are lacerations (knee level mostly) and tibial/ankle fracture or dislocations. Branches to the gastrocnemius and soleus muscles originate proximal to the tibial nerve’s passage below these muscles. Therefore, when these muscles are weak, the lesion is in, or proximal to, the popliteal fossa. Sparing of the tibialis posterior (foot inversion) helps localize a tibial lesion to the deep posterior compartment of the mid-leg or below. Furthermore, sparing of the flexors digitorum and hallucis longus places the lesion to the lower third of the leg or distal to the tarsal tunnel. Baker’s cysts or other mass lesions can also cause tibial palsies at the knee. Without a history of trauma, the examiner should thoroughly palpate the popliteal fossa for masses.
Common Peroneal Nerve Palsy
The usual type of peroneal nerve damage at the knee/leg is a stretch/contusion injury, usually with a concomitant fracture (usually sports related). Damage to this nerve is not uncommon because it is superficial and in a fixed position at the lateral fibular head. Of note, peroneal nerve palsy is the most common lower-extremity nerve injury occurring after trauma. Tribiofibular joint ganglion cysts, adjacent or even within the common peroneal nerve, may also cause a peroneal division deficit at the knee.
Idiopathic entrapment of the common peroneal nerve occurs below the fibrous edge of the peroneus longus muscle at the fibular head, the fibular tunnel (Fig. 6-25). Diabetics are especially prone to this problem. When this occurs, both the superficial and deep peroneal branches are involved to a variable degree. Sometimes, an isolated palsy to the deep peroneal nerve may occur when this branch passes under the fibrous edge of the extensor digitorum longus muscle. Common peroneal nerve entrapment patients have pain and numbness in a peroneal distribution (i.e., over the dorsum of the foot), radiating down from the fibular head. The lateral cutaneous nerve of the calf is spared because it does not pass through the fibular tunnel. Weakness of foot dorsiflexion (tibialis anterior), foot eversion (peroneus longus and brevis), and toe extension (extensor digitorum longus, extensor hallucis longus, and extensor digitorum brevis) may occur with more severe lesions. A Tinel’s sign is often present at the fibular head. Peroneal entrapment at the fibular head must be carefully differentiated from a L5 radiculopathy. In this situation, an electrodiagnostic consult is especially useful because the tibialis posterior is predominantly innervated by the L5 spinal nerve via the tibial nerve, not the common peroneal nerve.
Strawberry picker’s palsy occurs in persons who spend extended periods in the squatting position, which causes bilateral common peroneal nerve compression at the fibular heads. External trauma affecting the common peroneal nerve at the fibular head may occur more frequently in persons who quickly lose weight (slimmer’s paralysis). This is thought to be because with weight loss the adipose tissue that usually pads the common peroneal nerve is reduced, and furthermore, the patient now is able to cross his or her legs, something that was more difficult when the patient was heavier. Postpartum foot drop is also a known phenomenon, having a variety of causes. These include L5 radiculopathy, pressure upon the lumbosacral trunk where it passes over the bony margin of the sacroiliac joint, external compression of the common peroneal nerve or its branches by the leg holders in the lithotomy position, and in certain developing countries, from prolonged squatting.
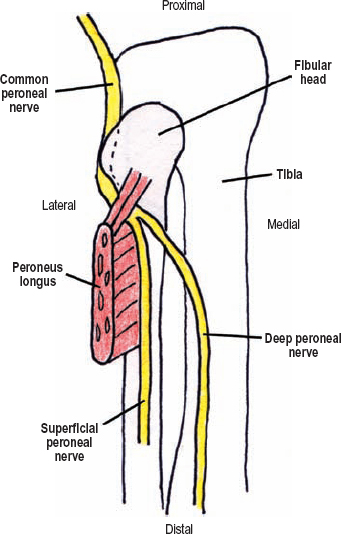
Figure 6-25 Peroneal nerve entrapment at the fibular head. Idiopathic entrapment of the common peroneal nerve may occur at the fibular head when this nerve passes below the fibrous edge of the peroneus longus muscle. Sometimes, an isolated palsy involving the deep peroneal nerve may occur when this branch passes under the fibrous edge of the extensor digitorum longus muscle.
 Posttraumatic compartment syndrome in the leg may involve the anterior, posterior, and/or peroneal (lateral) compartments, producing isolated nerve palsies in the deep peroneal, tibial, and superficial peroneal branches, respectively.
Posttraumatic compartment syndrome in the leg may involve the anterior, posterior, and/or peroneal (lateral) compartments, producing isolated nerve palsies in the deep peroneal, tibial, and superficial peroneal branches, respectively.
The Foot
Foot Drop
Isolated foot drop, or more specifically weakness in the tibialis anterior, extensor hallucis longus, and peroneus muscles, is caused by nerve injury in a variety of locations, including the L5 spinal nerve, lumbosacral trunk, peroneal (lateral) division of the sciatic nerve in the buttock or thigh, and the common peroneal nerve. Although an adequate history may be the most useful way to make the diagnosis, the clinical examination supplemented with electromyography can be confirmatory. For example, both L5 radicular and lumbosacral trunk lesions should cause tibialis posterior and gluteal muscle weakness. However, compared with L5 radicular lesions, patients with lumbosacral trunk damage usually do not have paraspinal muscle denervation on electromyography. Patients with peroneal division sciatic injury should have denervation of the short head of the biceps femoris, with all the other hamstrings being normal. It is rarely possible to observe short head weakness during muscular testing when the long head of the biceps femoris is functioning. In this situation, electromyography is useful.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is an uncommon entrapment involving the medial and lateral plantar nerves where they run under the flexor retinaculum, which is a ligament that connects the medial malleolus to the calcaneus (Fig. 6-3). Patients with this syndrome commonly have a history of regional ankle trauma, and therefore postinjury fibrosis may be a common cause. Other etiologies include systemic disorders (e.g., rheumatoid arthritis and diabetes mellitus). Patients with tarsal tunnel syndrome complain of sole pain, numbness, and/or paresthesias, which are worsened with walking and standing but relieved with rest and elevation. The pain usually is localized to the metatarsals. Heel pain is uncommon. Pinprick, vibratory sense, and two-point discrimination can be abnormal. Complaints of weakness are uncommon, but when present, involve the foot intrinsics. A Tinel’s sign may be present posterior to the medial malleolus, possibly radiating down into the foot. Percussion may also cause pain radiating up the course of the tibial nerve, known as the Valleix phenomenon. Peripheral neuropathy may be differentiated from tarsal tunnel syndrome because the former usually has sensory loss outside the territory of the tibial nerve (e.g., in the sural or saphenous nerves), as well as absent ankle jerks (the foot flexors are innervated proximal to the tarsal tunnel). Nerve conduction studies are used to help confirm the diagnosis of tarsal tunnel syndrome.
Anterior tarsal tunnel syndrome is a very rare cause of distal deep peroneal nerve entrapment under one, or both, extensor retinaculums on the dorsum of the foot (Fig. 6-26). Patients have extensor digitorum brevis muscle mass weakness (and/or wasting) on examination, report a dull ache on the dorsum of the foot, and sometimes have numbness localized to their first web space. A Tinel’s sign may occur. Tight-fitting shoes or local fibrosis following trauma may be causative.
Morton’s Neuroma
Morton’s neuroma is actually not a neuroma, but the chronic irritation of a common plantar nerve, usually the one innervating the third web space. This nerve is usually made up of branches from both the medial and lateral plantar nerves, and is pinched repetitively between the third and fourth metatarsal heads where this nerve runs under the deep transverse metatarsal ligament (Fig. 6-27). Focal swelling of the nerve occurs secondary to intraneural fibrosis.
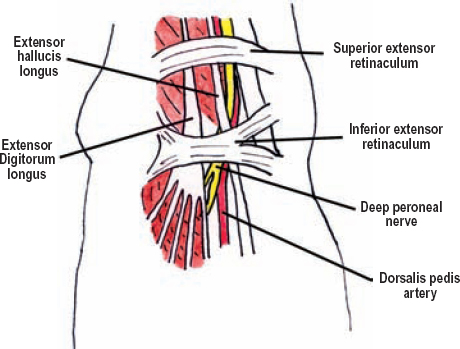
Figure 6-26 Anterior tarsal tunnel anatomy (dorsal view). This syndrome is a very rare cause of distal, deep peroneal nerve entrapment under one, or both, extensor retinaculums on the dorsum of the foot. Patients have dorsal foot discomfort, numbness in the first web space, and possible wasting of the extensor digitorum brevis.
Patients with a Morton’s neuroma have pain between the third and fourth metatarsals, which radiates to the third and fourth toes. The pain is worsened with walking, relieved by rest and elevation, and usually does not occur at night. Squeezing the metatarsals together can cause a shooting pain into the third and fourth toes. A Tinel’s sign may be present. An ultrasound examination can help make the diagnosis.
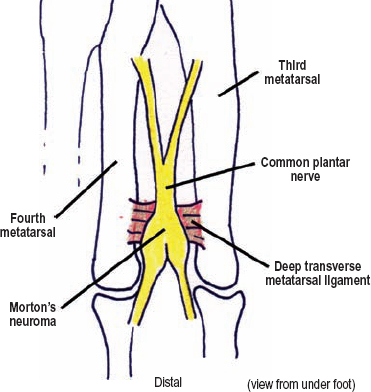
Figure 6-27 Morton’s neuroma. This is actually the chronic irritation of a common plantar nerve, usually the one innervating the third web space, which causes perineural fibrosis, not aneuroma. The affected nerve is pinched repetitively where it runs between the third and fourth metatarsals under the deep transverse metatarsal ligament.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




