Fig. 13.1
Illustration of a drum kymograph
Oscillographs, Drum Kymographs, and Strip Chart Recorder
The string galvanometer was not suitable for making recordings over extended time periods. Oscillographs could also be used with bromide paper but long-duration recordings presented a technical problem. However, another device invented decades earlier could be adapted. A German physiologist named Carl Ludwig invented a “wave writer” or kymograph [3] that utilized a cylinder or drum around which a piece of paper could be attached (see Fig. 13.2). A stylus marked the paper as the drum rotated. Early versions used the stylus to scrape off soot from pre-smoked sheet but eventually ink became the preferred writing medium. In this manner, scientists could make recordings over longer time periods, especially when the stylus traversed a worm screw preventing overwriting after the drum completed a full rotation. An alternative approach involved moving a continuous strip of paper (from a roll or fanfolded) under ink pens at a constant speed. The drive mechanism typically incorporated several gear ratios that could move the paper ribbon or strip with rotating sprockets, pinch rollers, or some other mechanism.
Fig. 13.2
Hans Berger’s string galvanometer
Gibbs and Garceau were able to construct a one-channel EEG machine by adapting the Weston Union Morse Code inkwriting undulator while Albert Grass who was working on earthquake seismographs created a three-channel EEG machine. After 1938, EEG rapidly gained popularity as both a research and clinical tool. Polygraphic recording devices (e.g., the grass model 1) became commercially available (see Fig. 13.3). Groups in both Europe and America applied this new approach to psychiatric and neurologic disorders, describing, documenting, and naming various waveforms. Some recordings were made during sleep by sampling EEG and researchers described periods of low-amplitude mixed-frequency activity alternating with high-amplitude slow waves. Gibbs and Gibbs also remarked that EEG was mostly symmetrical during sleep, except during the low-voltage, mixed-frequency episodes [4].
Fig. 13.3
Grass model I polygraph
Tuxedo Park
Alfred Loomis was an eccentric, and very wealthy, lawyer-turned Wall Street tycoon who established a research center in Tuxedo Park in the 1930s sometimes called the Loomis Laboratories [5]. Loomis excelled at mathematics and had a passion for science. He spent the fortune he made through investments to fund scientific research by the greatest minds in his time (including Heisenberg, Bohr, Fermi, and Einstein). In 1937, Loomis, along with Harvey and Hobart, published the first report from continuous, all-night studies of human sleep [6]. They had constructed an 8-ft.-long, 44-in.-circumference drum recorder (see Fig. 13.4) and monitored up to three channels at a time of signals switched through some sort of selector panel. Recording sites included (midline vertex, midline occiput, behind left and right ears, and just above and to the left of the left eye). They described a fourth channel that could be used to record signal markers, heartbeats , or respiration. They could manage 3.5 h of recording before paper needed changing. They wrote the following “…we have been able to establish very definite states of sleep which change suddenly from time to time, and to correlate these with movements, with dreams, and with external stimuli applied to the sleeping subject.” They described alpha, low voltage, spindles, “random,” and spindles plus random sleep state sequences. Interestingly, they recorded and described eye movement activity but did not establish an eye movement dreaming state of sleep. Their graphical depiction of sleep’s progression across the night looks remarkably similar to our contemporary hypnograms (see Fig. 13.5). Loomis invited Harvard professor Hallowell Davis and his wife Pauline to TuxedoPark and offered to fund his clinical EEG research. Davis accepted the offer. Loomis had a hopeful but ultimately misguided belief that EEG could be applied to psychological and psychoanalysis and he invited many distinguished psychiatrists to his laboratory. When World War II broke out, the Loomis Laboratories changed direction to help in the war effort. He helped by bankrolling the development of high-powered radio detection and ranging (RADAR) and Loomis radio navigation (LRN), later renamed long range navigation (LORAN); technologies that ultimately helped win the war (Fig. 13.6).
Fig. 13.4
Loomis’s drum recorder designed to conduct sleep studies
Fig. 13.5
Hypnogram as depicted by Loomis and colleagues
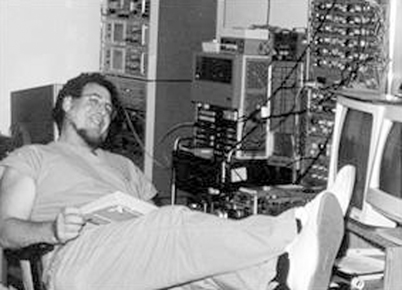
Fig. 13.6
Present author with sleep analyzing hybrid computer
Discover of REM Sleep
In 1953, Aserinsky and Kleitman published data showing dreaming occurred during the sleep stage associated with low-voltage, mixed-frequency activity [7]. Furthermore, rapid eye movement (REM) accompanied these events. In his book Sleep and Wakefulness, Kleitman describes the discovery in the following manner: “…we literally stumbled on an objective method of studying dreaming while exploring eye motility in adults…” [8]. He further noted that Ladd (in1892), based only on introspection, posited eye movements during dreaming and Jacobson (in 1937) had written “When a person dreams…most often his eyes are active.” Nonetheless, the electrophysiological evidence in their landmark paper officially ushered in a key step toward more fully describing sleep. Meanwhile, Jouvet found his cats lost muscle tone during “paradoxical sleep” episodes which completed our picture of stage REM sleep [9]. These discoveries also marshaled the beginning of multichannel electrophysiological recording of EEG, electrooculogram (EOG), and sometimes electromyogram (EMG) for studying sleep.
Exploring REM sleep and comparing its mental and physiological correlates to other stages of sleep became a standard paradigm. Dream content, both spontaneous and provoked, during REM represented a very hot topic. After all, Freud had called dreaming the royal road to the unconscious mind [10]. Sleep studies targeting stage REM now provided a laboratory tool to explore the unconscious processes. Concomitant recordings of respiration, heart rhythm, electrodermal activity, paved the way toward what we now call PSG .
The Standardized Manual
As more investigators began researching sleep phenomena, scientists realized that a standardization of techniques could immensely facilitate communication and possibly progress. After REM sleep’s discovery, summarizing sleep integrity, continuity, and architecture required more sophistication that the Loomis system offered. Thus, research groups created their own terminology and scoring rules. Dement and Kleitman evolved a system to classify sleep according to EEG criteria [11]. Essentially, a time domain of the set duration was established and the dominant activity within that time-frame-dictated classification . This time domain, called an epoch, could be classified as sleep stage 1, 2, 3, or 4 or awake according to EEG characteristics. When REMs occurred during stage 1 sleep, the stage was designated REM sleep. However, recording technique and terminology differed between sleep laboratories. REM sleep was also called paradoxical sleep, desynchronized sleep, active sleep, D sleep, and even unorthodox sleep.
Ultimately, an ad hoc committee was formed to develop “A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects.” [12] Chaired jointly by Drs. Allan Rechtschaffen and Anthony Kales the committee was a who’s who of sleep experts, including William C. Dement, Michel Jouvet, Bedrich Roth, Laverne C. Johnson, Howard P. Roffwarg, Ralph J. Berger, Allan Jacobson, Lawrence J. Monroe, Ian Oswald, and Richard D. Walter. The group standardized procedures, scoring rules, and terminology. More important, they reached consensus and thereafter used the procedures (for the most part) to conduct human sleep research. In essence, this was the real key to R&K (as it was called after the chairmen’s initials) successes. My understanding from stories I have been told by various participants indicated there were very strong (verging on violent) disagreements, shouting arguments, and name calling. In the heat of one less than civil debate, reportedly one of the chairmen barred the doors, decreeing that no one could leave until consensus was reached. Ultimately, consensus was reached and this is why R&K succeeded.
PSG, at least for sleep staging was established!
Psychophysiological Study of Normal Sleep
This new field, PSG , was ripe for discovery. In 1961, a research society emerged called the Association for the Psychophysiological Study of Sleep (APSS) and annual meetings were held to discuss research findings. The meeting proceedings were originally published in the Psychophysiology (the journal for the Society for Psychophysiological Research) which sported the image of a PSG tracing on its cover. Research laboratories at major universities, at US Naval and Army research centers, in European research institutes, and large medical centers began recording human sleep to describe its biology and to try to understand its underlying process. Whether a particular line of inquiry aimed to elucidate the function of sleep or to derive the intricacies of its process, progress, and some breakthroughs were being made. Sleep deprivation was a popular paradigm in the attempt to infer function. The examination of sleep stage rebound in response to selective stage deprivation provided a model to explore sleep’s homeostatic regulation. The military was interested in the adverse effects sleep deprivation had on behavior, attention, cognition , and physical ability.
Many studies focused on REM sleep phenomena. Obviously, dreaming represented a very seductive and intriguing topic; however, no unified theory of dreaming grew out of PSG research. Nonetheless, scientists found the eye movements generally corresponded to direction of gaze in the dream sensorium, middle ear muscle activity concorded with dreamt sounds, and nocturnal erections accompanied REM sleep but did not correspond to sexual dream content. Physiologic events associated with PSG stages other than REM sleep included timing and release of growth hormone during slow-wave sleep , slow-wave activity as a marker for homeostatic drive, other endocrine secretions in sleep, and physiological stability of cardiopulmonary functions during non-REM (NREM) sleep. Note the intuitive appeal of referring to sleep as REM and NREM. However, this terminology highlights how enamored polysomnographers were with REM sleep. REM sleep is the minor partner in sleep, yet we label the majority of sleep as not REM. Perhaps we should refer to wakefulness as non-sleep.
Sleep Latency Tests
Multiple Sleep Latency Test
The sleep studies performed in the Stanford summer sleep camp on children and teenage as well as other studies performed on college students and patients with sleep disorders led to conceptualization of daytime sleep latency as a biomarker for sleepiness. The studies in children were part of Mary A. Carskadon’s doctoral dissertation “Determinants of Daytime Sleepiness: Adolescent Development, Extended and Restricted Nocturnal Sleep (1979).” Carskadon and Dement [13] described multiple sleep latency changes across the day during an experimental 90-min sleep–wake schedule in Sleep Research. Sleep Research, at the time, was a major vehicle for sharing information in the sleep community. Their subjects had 16 opportunities to fall asleep (and were instructed to “close your eyes, lie quietly, and try to fall asleep”) over each 24-h period as they underwent baseline, sleep deprivation, and recovery periods. PSG recordings from these studies helped form procedures later used in multiple sleep latency test (MSLT). The following year, Richardson et al. [14] published daytime sleep latency findings for patients with narcolepsy and controls. Sleep latency as a biomarker for sleepiness validation came soon after with experimental studies of acute sleep deprivation, chronic sleep restriction, and concordance with other performance measures [15, 16].
The PSG and operational procedures for conducting and analyzing the MSLT were extremely well thought out and effective right from the start. Methods quickly became standardized and a coherent body of literature emerged. A research version (minimizing accumulated sleep) and a clinical version (providing 15 min of sleep to permit REM occurrence) evolved. MSLT’s utility for objectively measuring sleepiness and confirming narcolepsy (by REM occurrence) made MSLT an essential part of sleep research and sleep medicine. Guidelines for MSLT were formally adopted in 1986 in the journal Sleep [17]. Current clinical guidelines continue to endorse MSLT for diagnosing narcolepsy [18] and research projects still turn to the MSLT when they need an objective measure for sleepiness.
Maintenance of Wakefulness Test
While the ability to fall asleep depends on underlying sleep drive, the ability to remain awake in the face of sleepiness involves additional factors. The inability to volitionally maintain wakefulness in soporific circumstances became the focus of many sleep researchers, clinicians, and regulators. The role of sleepiness in fatigue-related accidents needed definition. The failure of the brain’s alertness system in sleep restricted, deprived, or impaired individuals contributes to fatigue in a manner that cannot be engineered away by human factors or ergonomic improvements. Mitler et al. developed maintenance of wakefulness test (MWT) using procedures similar to MSLT but changed the instructions from “try to fall asleep” to “try to remain awake.” Criterion group validation in patients suffering from sleepiness succeeded [19, 20]. MWT is a powerful tool (the US Federal Aviation Administration endorsed its use) but methodology varied from study to study, sometimes making it difficult to compare results. A critical variation is test session length which ranges from 20 to 60 min. After a normative data trial [21], test session length settled on 40 min. Current clinical guidelines published in 2005 endorse 40-min sessions, provide standard procedures, and stipulate clinical indications for use [18].
Clinical PSG
Exploration, Biomarkers, and Diagnostics
Just as EEG proved useful in clinical applications, PSG held similar promise. Robert L. Williams was a pioneer and unsung leader in sleep medicine. He explained to me that understanding sleep disorders first required characterizing normal human sleep. Beginning in 1959, his sleep laboratory at the University of Florida, College of Medicine in Gainesville began making continuous all-night sleep recordings in normal, healthy male and female children, adolescents , teenagers, young adults, adults, and seniors. A decade and a half later these “norms” were published in The EEG of Human Sleep [22].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





