Chapter 3
The Hypertonicity Intervention Planning Model for Upper Limb Neurorehabilitation
Chapter objectives
- Describe the many factors that influence clinical reasoning and decision-making in relation to upper limb hypertonicity.
- Identify the different types of knowledge (theory-, practice- and research-based) and associated reasoning styles that clinicians have access to during clinical decision-making, and describe how they contribute to ‘evidence-based practice’.
- Describe strategies for integrating or translating knowledge into rehabilitation practice.
- Introduce and describe the Hypertonicity Intervention Planning Model (HIPM) for structuring clinical decision-making in relation to the upper limb affected by hypertonicity.
Abbreviations
| EBM | Evidence-based medicine |
| EBP | Evidence-based practice |
| HIPM | Hypertonicity Intervention Planning Model |
| HGF | House, Gwathmey and Fidler Thumb Classification |
| MASMS | Modified Ashworth Scale of Muscle Spasticity |
| MCP | Metacarpophalangeal (joints) |
| MTS | Modified Tardieu Scale of Muscle Spasticity |
| OCEBM | Oxford Centre for Evidence-Based Medicine |
| PBE | Practice-based evidence |
| RCT | Randomised controlled trial |
| SCED | Single case experimental design |
| UMNS | Upper Motor Neuron Syndrome |
| Z&Z | Zancolli and Zancolli Hand Classification |
3.1 Decision-making in clinical practice
Making decisions in clinical practice is rarely straightforward or simple, yet the decisions made by health professionals often greatly impact clients and their families at a time when they may be most vulnerable and dependent on professional guidance. The nature of clinical practice is that it takes place in dynamic, changing, unpredictable situations that often require clinicians to ‘think on their feet’ while seeking to offer a best practice service to their clients. Increasing complexity is evident in practice settings in terms of new knowledge and technologies, greater role specialisation, service provision in interdisciplinary teams, changing client demographics (for example, ageing and increasingly multicultural populations), and financial and political constraints. In recognition of such complexity, clinical reasoning has been described as
… a process by which the therapist seeks to understand, explain, and predict organisation, structure and patterns within “messy” and multifaceted real-world situations [1, p. 42].
There are typically a variety of factors that influence the process of clinical reasoning and its outcomes, clinical decisions. Taking all these factors into account and discerning how to weight each one to suit individual circumstances can be a difficult balance to maintain and a complex process to negotiate. Thus, the clinician’s task involves seeking and integrating a large amount of information relevant to the client, as well as the clinical environment, in order to make effective clinical decisions and intervention recommendations.
3.1.1 Factors influencing decision-making
Clinical decision-making is influenced by many factors related to the client, the clinical environment and the clinician. Examples of these factors include the attitudes, beliefs and priorities of both the client (together with his or her family and friends) and the clinician, professional experience and knowledge, the perspectives of colleagues and multidisciplinary team members, and organisational expectations and resources. Rogers and Masagatani [2] described these diverse factors as being either intrinsic (related to the client) or extrinsic (related to the clinical context or environment and to the clinician). A number of consistent influences on clinical decision-making have been identified across different settings and client diagnostic groups (Table 3.1).
Table 3.1 Intrinsic and extrinsic factors influencing clinical decision-making.
| Category | Factor |
| Intrinsic Client-related |
|
| Extrinsic Environmental, contextual |
|
| Extrinsic Therapist-related |
|
What do we know about the decision-making and intervention choices of clinicians working with children and adults with stroke, traumatic brain injury or cerebral palsy? Several studies have found that it is the intrinsic, client-related factors related to the person’s condition (including neuromuscular impairment-level components, such as spasticity, muscle weakness or contracture and joint changes, atypical or stereotyped posturing, acuteness or chronicity of the condition, and sensory or cognitive performance problems) that are most likely to influence decision-making in neurological settings [9, 27].
A qualitative study with expert clinicians identified two additional types of client-related factors as influencing decision-making and intervention choice. These included the client’s personal attributes, such as age, attitudes to participating in therapy, and living situation (for example, in a metropolitan or non-metropolitan area, in one’s own home or a residential setting), as well as the client’s particular daily performance needs, such as being able to answer a telephone at work, or to produce written work at school. In the same study, an extrinsic factor was found to include clinicians’ embodied knowledge regarding the ‘feel’ of a person’s limbs and joints when affected by different severities of hypertonicity. In particular, clinicians indicated that extensive experience working with similar clients was essential for guiding their decision-making, given the limited availability of research evidence that supported the use of one treatment approach or technique above another. It was also evident that clinicians demonstrated personal preference for particular types of intervention options, based on confidence and personal convictions relating to the perceived efficacy of certain techniques [27]. Level of expertise is a further clinician-related factor identified as influencing decision-making, with clinicians who have a higher level of expertise in neurological practice demonstrating more consistency in decision-making and greater capacity for discrimination between client characteristics. Interestingly, in this and another study, level of expertise was not found to be related to length of practice [10, 28].
Work settings and organisational policies are also reported to influence clinical decision-making. Rassafiani et al. [9] found that treatment choice for children with cerebral palsy and upper limb hypertonia was strongly correlated with the setting in which the clinician worked. Using the same case vignettes, clinicians working in educational settings were most likely to choose splinting as the appropriate treatment choice, clinicians working in a hospital context were most likely to choose Botulinum toxin injections, while in community settings the preferred choice was upper limb casting. It is interesting to note that despite their different clinical decisions, there was no difference between these clinician groups in terms of the factors they considered in the case vignettes when making treatment decisions. The authors explained the findings in terms of the influence on decision-making of different organisational policies across settings, that is, a more disease- focused approach in hospital settings compared with a less medical approach in community and educational settings.
3.1.1.1 Using different types of knowledge for decision-making
Clinical experience, embodied knowledge, personal preference, scientific and theoretical knowledge, and level of expertise are described in 3.1.1 as extrinsic, clinician-related factors that influence decision-making in upper limb rehabilitation. These factors are all knowledge-related, either personal (experience, expertise, embodied/practical knowledge, personal preference) or public (shared, external, scientific/theoretical). Research indicates that clinicians use different types of knowledge when thinking or reasoning about different aspects of the clinical situation or the clinical problem, although they have trouble describing the knowledge and processes that they are using because they have become ‘tacit’, that is, unconscious or implicit within daily practice [23].
Mattingly and Fleming’s [23] seminal occupational therapy research identified procedural, interactive, conditional and narrative modes of reasoning, while other authors have referred to ethical [29–31], diagnostic [6, 32], scientific, pragmatic [33] and generalisation reasoning [34]. When using procedural, diagnostic or scientific reasoning, the clinician relies on theoretical, scientific (research-based) and technical knowledge. Narrative, interactive and conditional reasoning styles make use of storytelling, interpersonal, philosophical and psychological knowledge, while pragmatic reasoning is grounded in situational or contextual knowledge. Ethical reasoning relies on both interpersonal knowledge and interactive reasoning, by which the clinician understands the client’s illness or disability experience and can determine “what ought to be done [in order to facilitate achievement of] the patient’s valued goals” [29, p. 601]. In general, it is agreed that decision-makers use different knowledge and reasoning styles for different purposes, for example, to form a relationship with the client, to understand his or her story, or to predict whether a certain intervention will have a positive outcome [35, 36]. As such, clinicians move between reasoning styles during a single interaction with a client [37].
Higgs, Titchen and Neville [38] have similarly described clinicians as using three different types of knowledge when making clinical decisions. These include scientific knowledge (from research evidence or theory), professional craft knowledge (from previous clinical experience), and personal knowledge (about oneself and one’s relationships with others). Integrating and applying different types of knowledge is recognised as a challenge in rehabilitation practice [39–41], particularly in light of the evidence-based practice (EBP) movement which questions “expert judgment as an admissible type of evidence” [42, p. 160].
3.2 Evidence-based practice: What it is and what it isn’t
Evidence-based practice has increasingly become recognised as essential to all areas of rehabilitation, including upper limb neurorehabilitation. Its purpose is to promote client outcomes by reducing subjectivity and variation in clinical reasoning and decision-making [43]. The most commonly accepted definition of EBP was originally developed to define evidence-based medicine or EBM. It emphasises the integration of a number of types of knowledge and sources of information, including research evidence, clinical expertise, and client values and preferences:
Evidence-based [practice] is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients. The practice of evidence based [rehabilitation] means integrating individual clinical expertise with the best available external clinical evidence from systematic research. By individual clinical expertise we mean the proficiency and judgment that individual clinicians acquire through clinical experience and clinical practice… By best available external clinical evidence we mean clinically relevant research, often from the basic sciences of medicine, but especially from patient centered clinical research … Good [clinicians] use both individual clinical expertise and the best available external evidence, and neither alone is enough [44, pp. 71, 72].
Although this definition supports the integration of different types of knowledge and presents clinical expertise as a valuable aspect of EBP, expertise (sometimes termed mechanism-based reasoning, see Section 3.2.2) has typically been either omitted or placed in the bottom level of evidence hierarchies (Figure 3.1). In contrast, blinded, randomised controlled trials (RCTs) are viewed within the EBP paradigm as providing ‘gold standard’ evidence and are therefore placed at the top of the evidence ranking hierarchy, together with meta-analyses and systematic reviews of RCTs [42, 45]. Although EBP supports the integration of different types of knowledge, the process of doing this has not been operationalised [46].
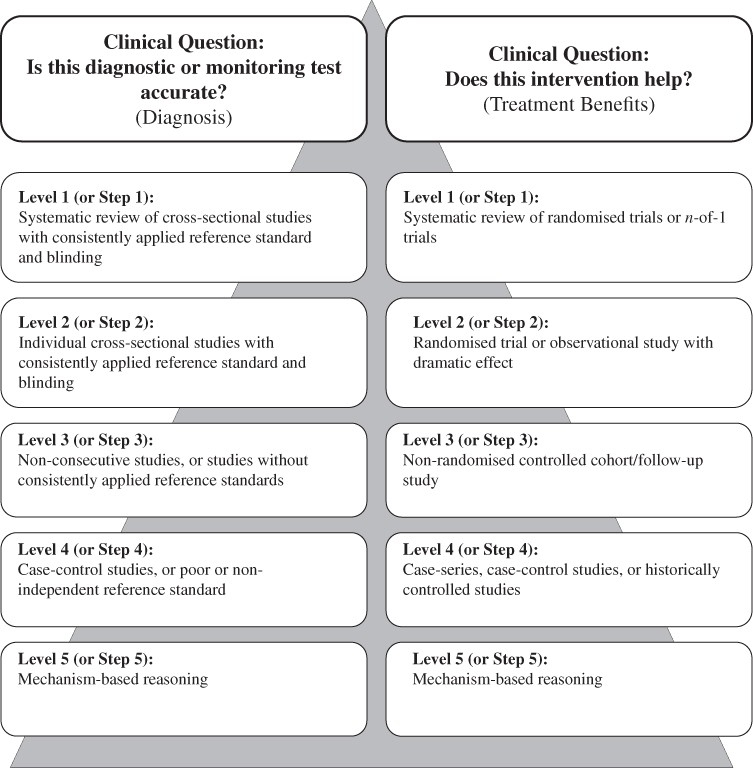
Figure 3.1 Evidence-based medicine hierarchy, extract (diagnostic test accuracy and treatment benefits) based on the Oxford Centre for Evidence-Based Medicine’s levels of evidence [45]. (See Box 3.1 for further explanation regarding revised levels of evidence).
How then, should clinicians use different types of knowledge in their practice of rehabilitation for the upper limb affected by hypertonicity? Similarly, how should clinicians determine what constitutes ‘evidence-based practice’, and what does not?
3.2.1 Practice-based knowledge: knowing how
Practice-based knowledge or ‘knowing how’ is a highly valued skill in therapy-based rehabilitation practice that develops out of familiarity with, and repeated performance in, particular clinical situations. Prolonged contact with similar client groups within those clinical situations leads to the construction of domain-specific, contextualised knowledge and, ultimately, to expertise [38, 47]. Experienced clinicians develop internal representations, or stereotypical images or ‘scripts’, of frequently encountered clinical problems, allowing recognition and naming of meaningful patterns or clusters of cues, signs or features. This personal, contextualised ‘body of knowledge’ enables the clinician to make fine discriminations between cues that are typical, atypical, expected, unexpected or missing in clients with particular conditions. Pattern recognition is then proposed to lead to the almost automatic generation of potentially useful assessments, interventions, goals, and predictions concerning possible client outcomes, based on past experiences with successful (or unsuccessful) interventions [48–50].
However, although EBP (and its medical counterpart, EBM) are typically described as the integration of high quality research evidence with clinical expertise [44, 51], reliance on experience and expertise is also described as resulting in biased and sub-optimal clinical decision-making [52]. In an attempt to clarify the place of expert clinical judgment in EBM, Howick [42] differentiates between different types and roles of clinical judgment and expertise. General clinical judgment is considered unreliable as a source of evidence and is therefore appropriately placed at the bottom of, or omitted from, evidence hierarchies. However, recommended roles for clinical experience within EBP include the integration of information about intervention effectiveness with client values and circumstances (described as integrating expertise), maximising the benefit of interventions through ‘therapeutic use of self’ (described as therapeutic expertise), and performing tasks that involve tacit knowledge, such as recognising signs and features (described as clinical expertise).
The notion of reliance on explicit (external) knowledge as more reliable than tacit (internal) knowledge lies at the heart of the EBP movement’s assumptions about what constitutes knowledge (or epistemology). Thus, the EBP movement assumes that “the best available external clinical evidence from systematic research” [44, p. 70, italics added] provides more reliable knowledge on the basis of the methodological design of clinical research trials, than does internal, tacit knowledge learned through experience. This assumption that experimental research methodologies are more reliable and always provide greater ‘strength of evidence’ for clinical practice is increasingly being called into question, since clinical judgment and the knowledge gained through experience are acknowledged as being inextricably linked with clinical decision-making, even in research trials [42, 53, 54]. For example, if a clinical trial is comparing the use of resting hand splints to manual stretches to reduce spasticity, then clinical experience is still being relied upon to make decisions about how the stretches will be provided, how it will be implemented, how the splint will be made and when it is worn, how long after splint removal outcome measures will be taken and so on. The credibility of practice-based knowledge is recognised as having a valuable contribution to make in medical as well as therapy settings. For instance, expert knowledge and clinical know-how are judged to be reliable for decision-making and diagnosis in situations of medical uncertainty, and for teaching and mentoring of both medical and therapy students and novice clinicians [36, 55–58]. Practice-based knowledge is also recognised as having an essential role in translating statistical, population-based research findings to individual clients [42, 45, 53, 59, 60].
In addition to practice-based, embodied knowledge, expert clinicians in occupational therapy, physiotherapy, medicine and nursing have been shown to have access to specialised, domain-specific knowledge that includes a combination of theoretical/scientific knowledge and technical skill [50, 61–65]. The organisation of this diverse (but highly individual) body of knowledge helps differentiate between more and less experienced clinicians [21, 38, 66, 67].
3.2.2 Science- and theory-based knowledge: knowing that
Science- and theory-based knowledge is concerned with facts. Theory provides clinicians with principles and assumptions for defining function and dysfunction in relation to particular conditions or diseases [38]. Such knowledge assists clinicians to view (or ‘frame’) each client’s situation as an example of a general category. Relevant knowledge is used as a ‘conceptual lens’ through which to interpret presenting cues and to plan actions accordingly [68, 69]. However, within evidence hierarchies, reliance on theory and knowledge of underlying mechanisms is reduced in importance, and reliance on science takes precedence [70, 71].
In recent rehabilitation practice (during the growth of the EBP movement), science-based knowledge has been predominantly equated with that generated from research using empirical, quantitative methods. Thus, practice described as ‘evidence-based’ has placed greatest value on research methods that promote the highest internal validity (that is, identification of the ‘true’ causes of observed outcomes), primarily through blinding of researchers and/or participants, and randomisation to either a control or experimental participant group [72, 73]. However, research evidence that is generated by traditional experimental methodologies and that describes outcomes in terms of average, group-level statistical models is beginning to be viewed as having limitations in rehabilitation settings. In particular, such models are not designed to represent the complexity of clinical practice that is influenced by many factors (including heterogeneity or diversity of client presentation) or to evaluate the effectiveness of interventions for individual clients [74–77]. The assumption that higher ‘internal validity’ automatically leads to high generalisability (that is, to high external validity) has been criticised, particularly in regard to translating results to real-life clinical situations that are typically influenced by many uncontrollable factors or variables [73, 78]. Group-level research focuses on the average results of ‘typical’ groups of people. Therefore, another criticism of sole reliance on RCTs as evidence in rehabilitation is that the causes of within-group variability for both research and control groups cannot be clarified (this is sometimes described as a ‘black box’ research model because only the inputs and outputs are known, whereas what goes on inside the ‘box’ cannot be known). Once again, translating study results to different populations becomes problematic [70, 78]. In such situations, clinicians are encouraged by some academic/researchers to adopt alternative research designs to augment findings from controlled designs [75], to use reasoning based on knowledge about pathophysiological mechanisms and effects to translate study results to individual circumstances (mechanism-based reasoning), or to understand the possible reasons for study results [79].
In clinical practice, mechanism-based reasoning is defined as making an inference “from (supposed) knowledge of the relevant mechanisms to claims that treatments have patient-relevant effects” [42, p. 126, original italics]. Thus, in rehabilitation practice, for example, mechanism-based reasoning might link an intervention (such as serial casting) with a clinical outcome (such as reduced muscle contracture) and/or an individual client goal (such as improved ability to push one’s arm through a sleeve), based on knowledge about relevant mechanisms (the sliding filament model of actin and myosin muscle components, Section 2.1.2.1). Mechanism-based reasoning is placed on the lowest level of the OCEBM 2011 Levels of Evidence hierarchy [45]. However, in addition to using mechanism-based reasoning for generalising the results of clinical trials to individual clients, it has recently been recommended for use as evidence for defending clinical diagnoses and intervention efficacy [42, 70].
Based on the clinician’s knowledge and understanding of relevant pathophysiology, mechanism-based reasoning is described as having a role in diagnosis, where the clinician is able to determine a problem based on the features or cues that are present, and also in treatment, where the clinician predicts that the effects of an intervention will address the identified mechanism-based problem. Similarly, mechanism-based knowledge is suggested as useful for applying population-based statistical results or EBP guidelines that are derived from such results, in circumstances of multiple co-morbidities affecting a person’s functioning, or where the individual’s circumstances are distinctly different from the participant and/or contextual circumstances in the relevant clinical trial [42, 70, 79, 80]. This type of knowledge, about the potential effects of an intervention in individual circumstances on the basis of pathophysiological, mechanism-based reasoning, is described by Andersen [70] as expertise, built up over time through repeated clinical experience and reflection, and therefore valuable in the provision of EBM. As noted previously, Howick [42] described this capacity for generalisation as integrated (medical) expertise. In contrast to the medical literature, the use of pathophysiological or mechanism-based knowledge by therapists would typically be described as scientific/theoretical reasoning, that is, reliance on knowledge drawn from known or generally assumed facts about how a part of the body operates (Section 3.1.1.1). This discrepancy between how ‘mechanism-based’ reasoning is perceived in medical, compared with therapy practice, suggests that the typical EBM hierarchies are not as easily extrapolated to therapy-based rehabilitation as is typically supposed.
3.2.3 Research questions and study designs
The way in which knowledge is understood or believed to be created shapes the types of questions that researchers seek to answer, as well as the study design that is chosen as appropriate for investigating those questions [81, 82]. The EBP movement is grounded in the logical-positivist paradigm where knowledge is assumed to develop out of logical deductions that are grounded in observable facts. This approach includes a belief in empiricism which emphasises evidence as discovered in experiments. Thus, the EBP movement in healthcare (initiated within the biomedical, rather than therapy/rehabilitation, sciences) is concerned with questions related to intervention effectiveness and causal relationships, and advocates quantitative, experimental research designs (clinical trials) as producing the highest level of evidence (see Figure 3.1). In contrast, the interpretive-constructivist paradigm assumes that knowledge develops out of (or is constructed out of) the interpretations, values and experiences that occur during social interactions. Knowledge is therefore viewed as diverse, shaped by perceptual, social and environmental circumstances [82]. The aim of research in this approach is to describe and explain experiences within social contexts. Thus, research designs focus on idiographic (contextualised) research, using qualitative methodologies [83].
These different approaches to scientific inquiry, and the focus within the EBP movement on traditional empirical research designs, have caused tension among researchers as well as clinicians whose focus is on delivering services to individual clients [36, 75, 84]. Grimmer and colleagues [85, p. 189] describe the situation faced by allied health clinicians as they try to integrate ‘best evidence’ from both logical-positivist (empirical/quantitative knowledge and evidence) and interpretive-constructivist (experiential/practical/qualitative knowledge and evidence) approaches into their clinical practice as “the ‘therapies’ dilemma”. There is now a growing recognition of the need to accept a diversity of study designs that complement findings from traditional research designs while promoting the investigation of intervention effectiveness for individual clients [73, 75, 80, 86–91]. For example, although RCTs have the greatest capacity for minimising risk to internal validity through random allocation of participants, well-conducted non-RCTs that use control strategies such as paired observations and stratified sampling reduce sampling error satisfactorily to produce credible evidence [92]. Further, single case experimental designs (SCED) are designed to answer causal questions of effectiveness, and are regarded as especially appropriate for use in clinical settings [93]. They are now recognised as producing Level 1 evidence for patient treatment decisions, equivalent to the evidence provided by the systematic review of multiple RCTs [45] (see Box 3.1). This shift reflects the understanding that, for many conditions (including brain injury), some problems occur too infrequently to enable large sample sizes for research, and also that client heterogeneity is a barrier both to undertaking RCTs and transferring their findings to clinical practice [94].
The finding that there is little difference between the treatment effects and effect sizes found in RCTs and observational studies has also led to the use of practice-based evidence methodology (PBE) as a reliable alternative to RCTs in rehabilitation practice. The strengths of the PBE methodology (which uses an observational cohort design) include careful attention to patient characteristics to reduce bias, detailed standardised documentation for measuring the intervention process, patient diversity to improve generalisation or external validity, and the use of multivariate statistics to evaluate associations between factors and the effectiveness of intervention outcomes [79]. In relation to clinical evaluation research, occupational therapists working with children similarly described valuing the use of ‘practice-generated evidence’, which they used to refer to information generated from the documentation and evaluation of client programmes. The therapists identified that practice evidence could be generated at both individual and whole service levels. Individual level evidence referred to clinicians evaluating client outcomes on a case-by-case basis, while the whole service level involved evaluation of service processes and outcomes [96]. The importance of generating practice-based, clinical research using designs appropriate to answering genuine clinical questions is progressively being acknowledged as necessary in therapy-based rehabilitation [39].
In summary, then, rather than strict adherence to the notion of a single-hierarchy approach to developing and appraising research-based evidence in rehabilitation practice, a diversity of study designs suitable for answering clinical questions is becoming recognised as appropriate in therapy-based rehabilitation [39, 73]. In addition, rather than current approaches, where practice is driven by evidence generated by means of a traditional experimental research model, a pragmatic approach where practice is informed by research-based evidence generated through diverse models and combined with domain-specific clinical knowledge and client preferences, is increasingly advocated as having the best capacity for promoting client-centred rehabilitation outcomes [59,73,76,88,97–99]. While such an approach echoes the most commonly used definition of EBP (Section 3.2), it is different in that it values equally diverse ways of knowing (research-based evidence, clinical knowledge). In this approach, EBP does not involve a standard protocol applied to all clients and research knowledge is not prioritised above other forms of evidence. Although there may be protocol-driven elements in the procedures used once intervention decisions are made, for example, using a standard casting process, the application of the intervention is still likely to be individualised based on unique client characteristics, context and goals. It follows then, that EBP can best be described as the logical, systematic and transparent documentation/explanation of one’s clinical decisions. This includes the ability to cite the sources of information used to reach the decision, as well as the individual client factors taken into consideration to ensure that the decision is client-centred.
3.3 Clinical reasoning: A process of integration and differentiation
The implementation of EBP advocates the integration of practice-based and research evidence-based knowledge (see Section 3.2). There is, however, little guidance on how to achieve this integration. Barriers have been identified, leading to a gap between ‘science’ and ‘practice’ [100, 101]. Different reasoning styles and the knowledge associated with each have been identified in clinical practice (see Section 3.1.1.1). An understanding of how clinical reasoning occurs in different situations, in response to the content and characteristics of the reasoning task at hand, assists the clinician to most appropriately apply theory-, research- and experience-based knowledge for each clinical decision [102].
3.3.1 The dual-process model of clinical reasoning and decision-making
The dual-process model of clinical reasoning and decision-making proposes two types of processing (Type 1 and Type 2) that are employed in response to the reasoning environment and task, and which make use of distinctive cognitive systems. For example, neuroimaging studies have found that different regions of the brain are activated with reasoning and decision-making tasks attributed to either Type 1 or Type 2 processing [103].
The Type 1 or heuristic reasoning process is characterised by pattern matching (schema or scripts). It is intuitive, fast, situation-specific and flexible (many autonomous processes can take place at the same time, in parallel). It encompasses unconscious, tacit, practice-based knowledge, typically used in familiar settings. In contrast, the Type 2 or reflective reasoning process is slow, conscious, deliberate, rule-based, generalisable, often language-based, demanding of working memory, and tends towards sequential processing (although it still includes several cognitive processes). It relies on explicit, shared knowledge and is able to generate intentional or future actions, while Type 1 processing tends to generate routine, habitual behaviour. Type 2 processing is used when reasoning about abstract, hypothetical, novel or difficult problem or situations, and it is able to override Type 1 processes if necessary. Although there are ‘typical’ or ‘common’ features attributed to each of the reasoning modes, individual, personal differences are evident between reasoners, with intelligence and working memory particularly influencing Type 2 processing. Metacognition (thinking about thinking) and emotions are also known to influence reasoning processes [104–107].
Experienced clinicians are known to move between the different clinical reasoning styles, relying on the knowledge common to each, in a dynamic, fluid way in response to task content [34, 37]. The dual-process theory of clinical reasoning and decision-making supports the notion of integrating different types of knowledge, that is, practice-based (tacit, embodied, individual) and theory- and research evidence-based (external, shared) knowledge, depending on the reasoning or decision-making task and its situational or contextual circumstances. Although clinicians may feel hesitant about relying on ‘soft’ knowledge (learned through experience), especially in the light of the EBP movement’s focus on the certainty provided by ‘hard’ research-based evidence, Blair and Robertson [108] propose that clinicians should accept that some aspects of practice will be characterised by uncertainty, that is, that research evidence will not be sufficient to provide clarity and direction for every practice decision. Plsek and Greenhalgh [102, p. 627] agree, and suggest that for those aspects of the clinical situation where there is general agreement and certainty about decisions or directions, the clinician is justified in thinking “in somewhat mechanistic (that is, rule-based, scientific) terms” and applying a relatively straightforward research evidence-based solution. In contrast, for other aspects of the clinical situation where the ‘next steps’ are not as obvious, for example where research evidence is not available or the situation is influenced by many interacting variables, the clinician is recommended to think adaptively, and to rely on experience, practice-based knowledge and reflective practice [109]. How do clinicians achieve this integration in practice?
3.3.2 Knowledge integration during clinical reasoning
Until recently it was assumed that once research evidence became accessible to clinicians, it would quickly and easily be incorporated into practice. However, as the availability of research evidence has grown, difficulties with translating (also described as integrating, transferring or implementing) findings to practice have become evident. Strategies for integrating research evidence into practice include purposeful differentiation of clinical reasoning tasks [102], development of domain-specific knowledge [110], the use of conceptual models or frameworks at an organisational level [56, 111, 112] and the use of clinical ‘decision aids’ during practice [113–115].
3.3.2.1 Differentiating between clinical reasoning tasks
Expert and novice reasoners are recognised as using different types of knowledge and cognitive strategies in their clinical practice [62, 116–119]. The process of developing expertise in clinical settings has been described as the progression along a continuum from more explicit verbally-based knowledge to highly tacit, embodied and perceptual knowledge or, in the language of the dual-process model of clinical reasoning, from greater dependence on Type 2 knowledge and decision making to that of Type 1 [63, 116, 120–122]. Thus, novice clinicians depend on theory and an analytical, rule-based mode of reasoning to guide practice in every clinical situation [26, 62, 116]. In contrast, expert reasoners display flexibility in practice based on perceptual knowing, reflection and the use of short cuts such as pattern recognition, heuristics (‘rules-of-thumb’) and case experiences. They identify problems or situations in terms of typicality and are able to discern slight differences between them [63, 64, 120, 123].
In addition to being influenced by expertise, reasoning mode is also influenced by the reasoning task and environment. Thus, Type 1 (tacit, embodied) reasoning is more likely to be used in familiar or routine decision-making tasks, while Type 2 (analytical, deliberate) reasoning is more likely in new, unfamiliar or complex tasks [104]. For example, even experienced clinicians will seek assistance from colleagues and/or relevant treatment guidelines before embarking on treatment in a new area of practice, or when they have never encountered a condition before (that is, Type 2 reasoning and decision making would be chosen). Differentiating the type of decision-making task that one is faced with, that is, either familiar/routine or new/unfamiliar/complex, assists the clinician in choosing an appropriate reasoning style and associated knowledge, either practice- or theoretical/research evidence-based.
3.3.2.2 Developing and using domain-specific knowledge
Over time, clinicians develop a body of domain- specific knowledge that can be described as
an associative network [of] interconnected knowledge parts including, for example, theoretical intervention models, pathophysiological mechanisms, clusters of disease cues or signs and features, treatment techniques and contextual information [58, p. 198].
This description includes both practice- and research evidence-based knowledge that utilises Type 1 and Type 2 clinical reasoning and decision-making processes. Development of a personalised, domain-specific body of knowledge provides the clinician with flexibility in responding to routine and familiar situations, promoting the ability to ‘think on one’s feet’.
An example of the integration of knowledge and information sources used is provided by an expert clinician working in a community setting with children with complex needs and varied diagnoses, such as autism, cerebral palsy and developmental delay [124]. The knowledge (and sources of that knowledge) that were drawn upon by the clinician included theoretical (acquired from text books), research evidence-based (peer-reviewed journals) and practice-related (professional development activities, experience) knowledge (Figure 3.2). However, the clinician appeared to privilege client-related information, acquired through interview and clinical assessment, when making intervention decisions. A linear process of research utilisation has been described by some authors, where the clinician is prompted to seek information from research to support decisions on a client by client basis as needed [125, 126]. However, in familiar clinical situations reliance on already-internalised practice- and research-evidence based knowledge is more likely [41] (that is, Type 1 reasoning is most likely to be utilised). Thus, in this case, the clinician drew from her domain-specific body of knowledge, progressively developed and expanded through ongoing exposure to research-based evidence, professional development activities and clinical experience. The immediate clinical concerns of the client were foregrounded (used as a ‘lens’ through which to view the clinical situation) and the clinician’s body of knowledge indirectly informed on-the-spot decision-making regarding therapeutic action during the therapy sessions. This consistent commitment to client-centred practice is reported to be a characteristic of expert clinicians [25, 61, 127].
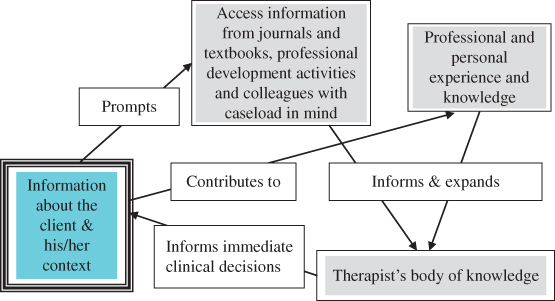
Figure 3.2 Use of a clinician’s body of knowledge in practice [124]. Reprinted with permission of CAOT Publications ACE.
In upper limb neurorehabilitation, when the clinician is making an intervention recommendation for the client’s consideration, an internal process of appraisal and interpretation of relevant knowledge (theory and research-, client- and context-related) appears to take place. The clinician uses his or her integrated body of knowledge to form a “temporary picture of the whole clinical situation” [3, p. 1492] that includes prediction of potentially realistic goals and interventions that are likely to assist in goal achievement. That is, rather than interpreting research-based intervention options as being relevant and applicable to all clients with a specific diagnosis or set of characteristics, clinicians integrate and sift their knowledge to understand the client’s needs, build a therapeutic relationship, organise assessment information, choose (aspects, or combinations of, potentially relevant intervention approaches and techniques) and negotiate appropriate interventions [1, 3, 22, 96].
3.3.2.3 Incorporating research-based evidence at an organisational level
As the process of EBP implementation matures, it is becoming apparent that integrating research evidence-based knowledge into clinical practice is a complex process that is not easily achieved. For example, while clinicians’ skills and attitudes have tended to be the focus of reports related to the research-practice gap, the need for active collaboration between researchers and ‘end users’ (clinicians, managers, policy-makers etc.) is now being recognised. Such collaboration is advocated in order to develop research programmes that address clinically-relevant questions and use appropriate research designs [56, 112, 128]. For instance, rather than using single interventions, clinicians report that they often adapt or combine interventions based on the environment and the client’s individual characteristics, reactions and goals in a responsive manner [1, 96, 124]. Yet, RCTs require that single interventions be implemented in a standardised manner that does not reflect the variability of clinical practice. Thus, the use of a conceptual model or framework, tailored to suit the needs of individual organisations, is recommended for more successfully guiding the integration of research evidence-based knowledge into practice. Examples of such frameworks, as well as strategies that can be used by organisations to support the integration of research evidence-based knowledge into practice, are available elsewhere [96, 129].
3.3.2.4 Incorporating clinical ‘decision-making aids’ into practice
Children and adults with upper limb dysfunction due to brain injury commonly display some similarities in presentation (Section 2.5.1), nevertheless, clinicians describe each person’s situation as subtly different [13, 41]. Hagedorn [130, p. 127] describes the clinician’s task during each new therapeutic encounter as one of “mak[ing] sense of [that particular] case”. Making sense of each particular ‘case’ requires the clinician to perceive and interpret relevant cues or characteristics about the person and his or her situation (using practice-based knowledge) and then, on the basis of those cues and relevant knowledge (either practice- or theory/research-based), to choose the treatment technique that is most likely to facilitate goal achievement. The use of decision-making aids or tools such as algorithms, clinical protocols, classification systems and taxonomies provides clinicians with an external framework or structure for organising complex, unfamiliar or unstructured clinical problems. The tools do this by identifying relevant cues, categorising or stratifying them, and then outlining key steps and decision points in the decision-making process [113, 115]. Decision aids are also reported to promote consistency by helping clinicians to develop ‘shared mental models’, that is, a shared understanding or representation of a situation or problem [131, 132].
Decision-making aids that categorise or stratify clinical factors or cues are common in neurorehabilitation practice. For example, the hand classification tool developed by Zancolli and Zancolli [133] (Z&Z, Section 2.5.1.3) can be used to systematically discriminate the characteristics (or cues) that are influencing the client’s positioning or movement (that is, identify and frame the problem characteristics), retrieve relevant knowledge (research- and/or practice-based), and choose an intervention that targets those particular characteristics [134, 135]. In particular, this hand classification tool identifies the impairment-level factors that are influencing wrist and hand positioning, allowing the clinician to discriminate between positive (excessive) features that need to be reduced, and negative (insufficient or missing) features of upper motor neuron syndrome (UMNS, see Section 2.4) that need to be strengthened or supported through intervention in order to promote function. Classification tools are also reported to promote pattern recognition, a strategy used to solve new problems by recalling patterns formed on the basis of previous experience with similar problems (Section 3.2.1) [5,64].
Decision-making aids have been incorporated into the EBP movement as ‘evidence-based clinical practice guidelines’, ‘clinical protocols’ and ‘treatment algorithms’. Their purpose is to promote the effectiveness, efficiency and standardisation of intervention recommendations for particular health conditions or in specific clinical situations [114]. Clinical practice guidelines are usually developed by committees or panels, comprised of clinical experts, researchers and relevant organisations or special interest groups, on the basis of available evidence and agreement regarding ‘best’ clinical practice [136]. Consensus statements are proposed to differ from clinical practice guidelines in that the former
“synthesise the available evidence, largely from recent or ongoing medical research, that has implications for re-evaluation of routine medical practices. They do not give specific, detailed practice algorithms [137].”
The Clinical Guidelines for Stroke Management 2010 (Australian National Stroke Foundation) [138] provide an example of an evidence-based clinical guideline, while an example of a consensus statement is Botulinum toxin assessment, intervention and follow-up for paediatric upper limb hypertonicity: international consensus statement [139].
The Hypertonicity Intervention Planning Model for upper limb neurorehabilitation (HIPM) is a clinical reasoning and decision-making aid that aims to guide clinicians through the complex process of choosing the most suitable intervention to maintain the long-term health and function of the upper limb affected by hypertonicity [140]. It was developed on the basis of both practice- and theory/research evidence-based knowledge, and is described in greater detail in the remainder of this chapter. The HIPM is different to the guidelines mentioned previously, which are limited to providing recommendations for interventions that have the highest level of research-based evidence, and which do not detail how to choose interventions for individual clients. The purpose of the HIPM is to guide the selection of clients who are most likely to benefit from a particular intervention on the basis of their upper limb characteristics, or, to put it another way, to make recommendations about suitable interventions according to individual upper limb features and movement patterns. This approach is supported within the literature as an important aspect of evidence-based practice [141]:
“EBM involves more than merely selecting the best therapy. It especially involves selecting the right patients, whose functional prognosis makes them suitable candidates for a specific therapy [141, p. 138].”
The HIPM adds to the decision-making aids already available in that it provides a single model suitable for guiding practice related to upper limb hypertonicity across settings, age groups and diagnoses. Rehabilitation research has indicated a need for this type of model, as expert clinicians have reported a consistency of factors influencing clinical decision making across hospitals, schools and community-based settings, for clients with cerebral palsy, stroke and traumatic brain injury, but a lack of support for deciding which intervention techniques to use in particular circumstances [27].
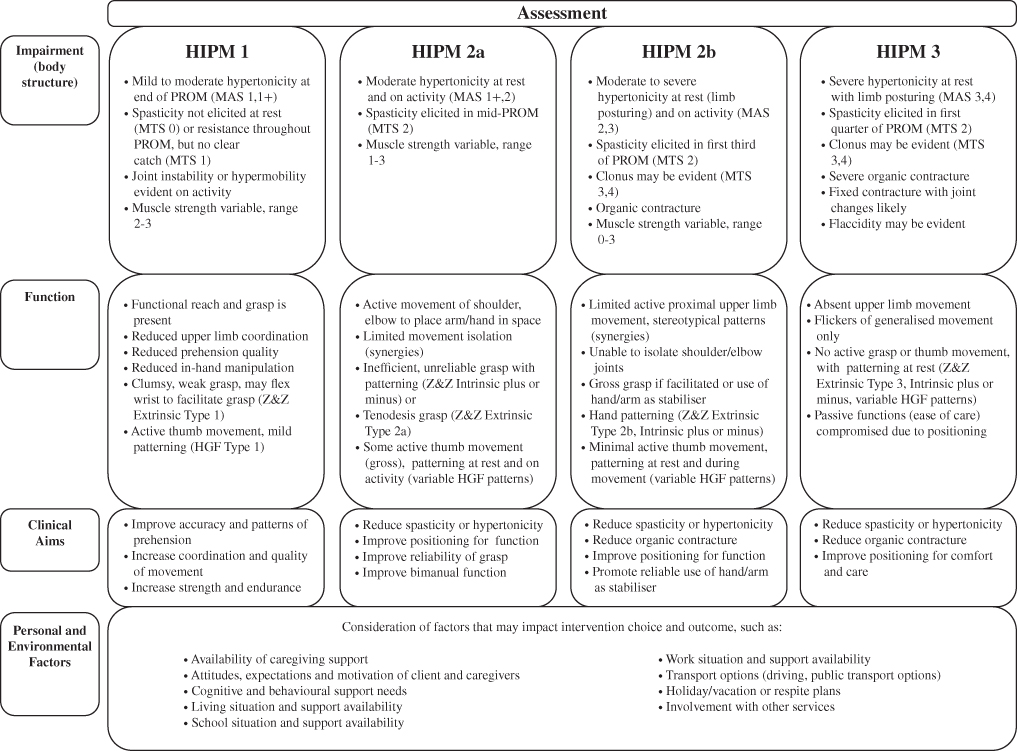
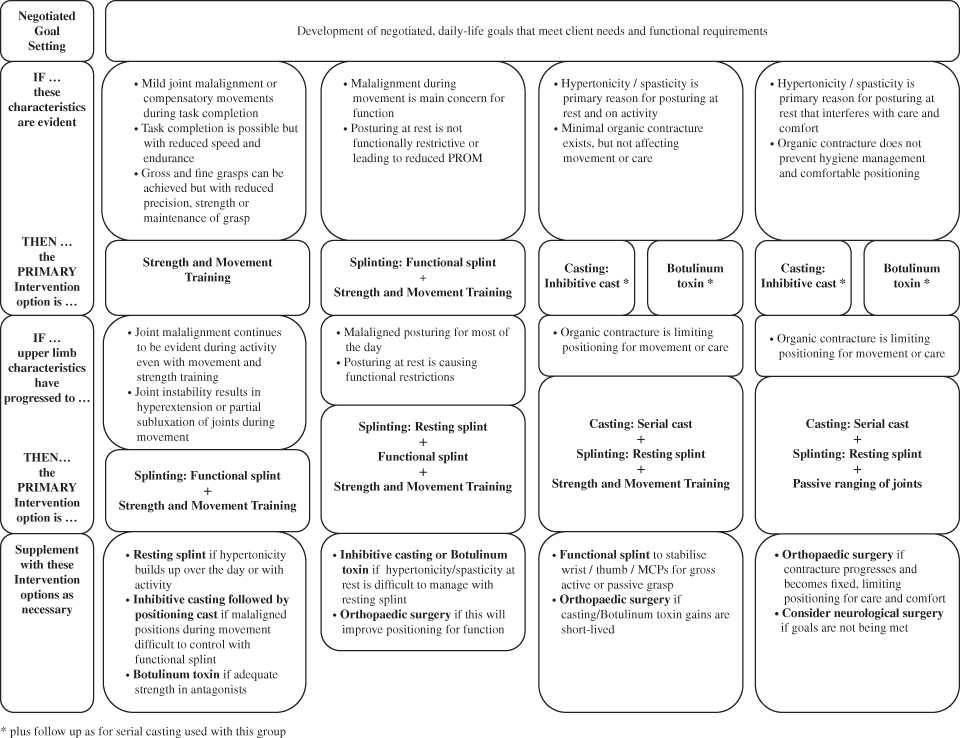
3.4 The Hypertonicity Intervention Planning Model for upper limb neurorehabilitation
The purpose of the HIPM (Table 3.2) is to provide structure to the process of managing upper limb hypertonicity by guiding the systematic application of theory/research evidence- and practice-based knowledge. The model seeks to identify and classify the impairments, adaptations and compensations underlying each client’s upper limb movement patterns and, in light of that assessment information, to negotiate individualised client goals and select appropriate intervention(s). This is achieved by structuring the model around the rehabilitation process (assessment/cue perception, problem identification, selection of intervention approaches or practice models, selection of intervention technique(s), clinician/client negotiation of goals, intervention implementation and intervention evaluation).
Table 3.2 The hypertonicity intervention planning model (HIPM) for upper limb neurorehabilitation.
The model emerged over time out of the authors’ combined experiences of teaching (at undergraduate and postgraduate university level courses, and at professional development workshops across different countries), clinical practice (with children and adults, in community and hospital settings, and in both private and public practice), and reflection-in-action (that is, during practice) as well as reflection-on-action (in many discussions together and with colleagues) [47]. Thus, the model is well-grounded in practice-based knowledge, occupational therapy theory (for example, the principles of client-centred practice and goal setting), and rehabilitation theory (for example, practice approaches), while research evidence is accumulating (see Section 3.4.5).
The HIPM has been well received by clinicians as a framework for directing assessment at relevant aspects of upper limb characteristics, for identifying and categorising upper limb capacity, and for guiding the selection of appropriate interventions [1]. The focus on “hypertonicity” in the title could be interpreted as promoting a focus on a positive feature of the UMNS (spasticity/hypertonicity), thus disregarding currently accepted neurological knowledge that negative features (paralysis or weakness, slowness of movement, loss of coordination and dexterity) and secondary adaptive changes (increased tissue stiffness, length-associated changes in muscles) are more disabling. However, this interpretation reflects a misunderstanding of how the HIPM is intended to be applied in practice. It categorises residual upper limb movement according to both positive and negative features of the UMNS. While it does focus clinicians’ attention on the secondary adaptive changes affecting Groups 2a, 2b and 3, this is because the development of contracture and spasticity “is an ever-present threat” [142, p. 194] for children and adults with little or no movement recovery. Research indicates that upper limb contracture is evident in 66% of people with moderate to severe stroke, with 29% of those having an affected wrist/hand [143]. This finding is confirmed by the results of a community clinic study where 69% of clients had upper limb contracture (wrist and/or elbow). This increased to 72% for clients with moderate to severe hypertonicity [4]. Unless clinicians are able to effectively prevent and/or manage contracture and spasticity, the potential effect on clients’ lives in terms of pain and discomfort is likely to be significant.
3.4.1 Description
The layout of the HIPM aims to assist the clinician to view the clinical situation with each client as a ‘whole’, while directing attention to salient upper limb-related information as well as critical decision points within the therapy process. It has nine sections, namely, assessment, group, impairment, functional abilities, clinical aims, personal and environmental factors that may affect the choice and outcome of intervention, negotiated (client-centred) goals, primary intervention options and supplementary intervention options.
The purpose of the first phase of the rehabilitation process, and therefore the top half of the model (encompassing assessment through to personal and environmental factors), is to develop a comprehensive picture of the individual’s functional performance status and to understand the changes that may be desirable and attainable. The aim of the assessment section is to facilitate the development of a clinical picture, and this is achieved by using assessment data to describe upper limb impairments and performance (or function). Identified upper limb problems (impairments and performance limitations) are grouped along a continuum, forming four groups, or clusters, of characteristics, grouped according to the severity of the impairments and their effect on upper limb performance. The aim of grouping upper limb characteristics in this way is to identify general patterns of upper limb performance against which individual clients can be compared [23].
Clinical (or clinician-identified) aims are developed on the basis of the particular upper limb impairments and functional abilities within each group. The purpose of developing clinical aims (see Box 3.2) is to facilitate links between identified upper limb problems and intervention objectives, as well as between problems and the most appropriate theoretical intervention approach or practice model for addressing the identified problems. Personal and environmental factors play a significant role in determining whether outcomes from intervention are sustained over time. While these variables are unique to each person, the purpose of this section is to prompt the clinician to consider all aspects of the person’s life that are relevant to achieving and sustaining a successful intervention outcome (keeping in mind that hypertonicity management is a long-term endeavour).









