FIGURE 20.1 Section through the medulla at the level of the decussation of the medial lemniscus.
The hypoglossal fibers gather into two bundles, which perforate the dura mater separately, pass through the hypoglossal canal, and then unite. The nerve descends through the neck to the level of the angle of the mandible, then passes forward under the tongue (hence its name) to supply its extrinsic and intrinsic muscles (Figure 20.2). In the upper portion of its course, the nerve lies beneath the internal carotid artery and internal jugular vein, and near the vagus nerve. It passes between the artery and vein, runs forward above the hyoid bone, between the mylohyoid and hypoglossus muscles, and breaks up into a number of fibers to supply the various tongue muscles. The nerve sends communicating branches to the inferior vagal ganglion and to the pharyngeal plexus. At the base of the tongue, it lies near the lingual branch of the mandibular nerve, which provides touch sensation to the anterior two-thirds of the tongue.
The branches of the hypoglossal nerve are the meningeal, descending, thyrohyoid, and muscular. The meningeal branches send filaments derived from communicating branches with C1 and C2 to the dura of the posterior fossa. The descending ramus join with fibers from C1, sends a branch to the omohyoid, and then joins a descending communicating branch from C2 and C3 to form the ansa hypoglossi (Figure 20.2), which supplies the omohyoid, sternohyoid, and sternothyroid muscles. The thyrohyoid branch supplies the thyrohyoid muscle. The descending and thyrohyoid branches carry hypoglossal fibers but are derived mainly from the cervical plexus.
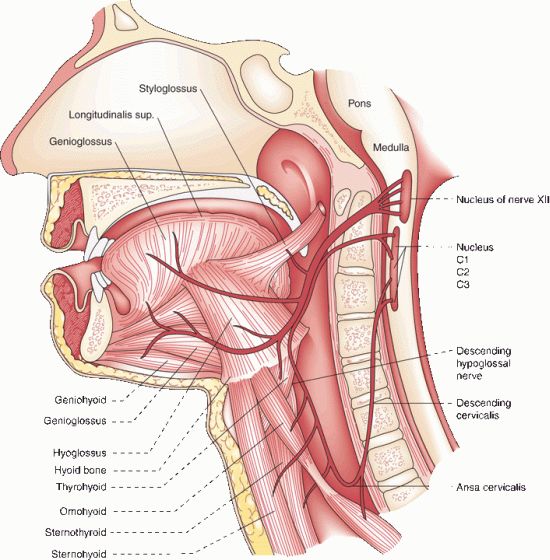
FIGURE 20.2 Ansa hypoglossi and muscles supplied by the hypoglossal nerve.
The muscular, or lingual, branches constitute the real distribution of the hypoglossal nerve. The tongue has extrinsic and intrinsic muscles. CN XII supplies the intrinsic muscles, and all of the extrinsic muscles of the tongue except the palatoglossus, and possibly the geniohyoid muscle. The paired extrinsic muscles (genioglossus, styloglossus, hyoglossus, and chondroglossus) pass from the skull or hyoid bone to the tongue. The genioglossus is the largest and most important of the extrinsic tongue muscles. It originates from the chin (Gr. geneion “chin”) and inserts into the tongue. The intrinsic muscles (superior and inferior longitudinales, transversus, and verticalis) arise and end within the tongue. The extrinsic muscles protrude and retract the tongue and move the root up and down. The intrinsic muscles change the length, the width, the curvature of the dorsal surface, and turn the nonprotuded tip from side to side. The actions of the tongue muscles are summarized in Table 20.1.
TABLE 20.1 Actions of the Extrinsic and Intrinsic Tongue Muscles
The cerebral center regulating tongue movements lies in the lower portion of the precentral gyrus near and within the sylvian fissure. The cortical representation of the tongue in humans is huge compared with other mammals and even other primates. In a patient with a small cortical lesion causing obvious tongue deviation, the lesion by MRI was located lateral to the precentral knob, a reliable anatomical landmark for the motor hand area. Therefore, the lesion involved the most lateral part of the precentral gyrus, lateral to the precentral knob.
The supranuclear fibers run in the corticobulbar tract through the genu of the internal capsule and through the cerebral peduncle. Some corticolingual fibers shift to the medial lemniscus in the pons. Other fibers leave the main ventral pyramidal tract and cross the midline at the pontomedullary junction to enter the hypoglossal nucleus from the lateral aspect. Supranuclear control to the genioglossus muscle is primarily crossed; supply to the other muscles is bilateral but predominantly crossed. Some authorities feel the entire supranuclear pathway is crossed.
The suprahyoid muscles also influence tongue movement by changing the position of the hyoid bone. The geniohyoid is supplied by C1 fibers traveling in the hypoglossal nerve. The other suprahyoid muscles are the mylohyoid and anterior belly of the digastric, innervated by CN V; and the stylohyoid and posterior belly of the digastric, innervated by CN VII.
Afferents in the hypoglossal nerve are primarily proprioceptive, but there may be some lingual somatic afferents present as well. The neck-tongue syndrome, consisting of pain in the neck and numbness or tingling in the ipsilateral half of the tongue on sharp rotation of the head, has been attributed to damage to lingual afferent fibers traveling in the hypoglossal nerve to the C2 spinal roots through the atlantoaxial space.
CLINICAL EXAMINATION
The clinical examination of hypoglossal nerve function consists of evaluating the strength, bulk, and dexterity of the tongue—looking especially for weakness, atrophy, abnormal movements (particularly fasciculations), and impairment of rapid movements. For videos of tongue fasciculations, see http://www.youtube.com/watch?v=gZZayxWWC5s and http://www.youtube.com/watch?v=RJ09XKb03Ck. Some use the term fibrillations rather than fasciculations when referring to the tongue, but this term is falling out of favor. After noting the position and appearance of the tongue at rest in the mouth, the patient is asked to protrude it, move it in and out, from side to side, and upward and downward, both slowly and rapidly. Tongue dexterity can be tested by having repeat lingual sounds, as in la-la-la, or use words with the t or d phoneme. For a demonstration of slow tongue movements and difficulty with labials, see http://www.youtube.com/watch?v=zh0xmb_qqzo&NR=1. Motor power can be tested by having the patient press the tip against each cheek as the examiner tries to dislodge it with finger pressure. The normal tongue is powerful and cannot be moved. For more precise testing, press firmly with a tongue blade against the side of the protruded tongue, comparing the strength on the two sides.
When unilateral weakness is present, the tongue deviates toward the weak side on protrusion because of the action of the normal genioglossus, which protrudes the tip of the tongue by drawing the root forward (Figure 20.3). Because the tip of the tongue is pushed out of the mouth, it deviates toward the paretic side. There is impairment of the ability to deviate the protruded tongue toward the opposite side. The patient cannot push the tongue against the cheek on the normal side but is able to push it against the cheek on the side toward which it deviates. At rest, it may deviate or curl slightly toward the healthy side because of unopposed action of the styloglossus, which draws the tongue upward and backward. There is impairment of the ability to deviate the protruded tongue toward the nonparetic side and of the ability to push it against the cheek on the sound side, but the patient is able to push it against the cheek on the paralyzed side. Lateral movements of the tip of the nonprotruded tongue, controlled by the intrinsic tongue muscles, may be preserved. Because of the extensive interlacing of muscle fibers from side to side, the functional deficit with unilateral tongue weakness may be minimal. There may be difficulty manipulating food in the mouth and an inability to remove food from between the teeth and the cheeks on either side. With either weakness or incoordination, rapid tongue movements may be impaired.
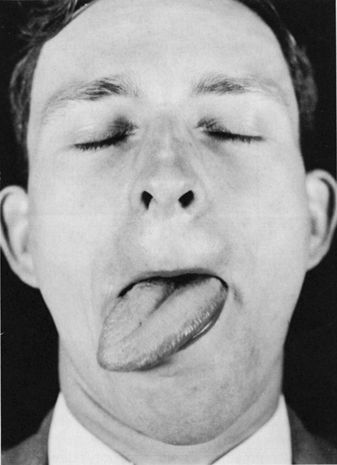
FIGURE 20.3 Infranuclear paralysis of muscles supplied by the hypoglossal nerve: Unilateral atrophy and deviation of the tongue following a lesion of the right hypoglossal nerve.
Facial muscle weakness or jaw deviation makes it difficult to evaluate deviation of the tongue. Patients with significant lower facial weakness often have distortion of the normal facial appearance that can produce the appearance of tongue deviation when none is present. Protruding the tongue may cause an appearance of deviation toward the side of the facial weakness. Because of the lack of facial mobility, the corner of the mouth does not move out of the way and the protruded tongue lies tight against it, making it look as though the tongue has deviated. Manually pulling up the weak side of the face eliminates the “deviation.” It may also be helpful to gauge tongue position in relation to the tip of the nose or the notch between the upper incisors.
If the paralysis is not accompanied by atrophy, the tongue may appear to bulge slightly and to be higher and more voluminous on the paralyzed side. When atrophy supervenes, the loss of bulk is first apparent along the borders or at the tip, and the tongue may take on a scalloped appearance (Figure 20.4). The normal slight midline groove may become accentuated. With advanced atrophy, the tongue is wrinkled, furrowed, and obviously smaller. The epithelium and mucous membrane on the affected side are thrown into folds. As the paralyzed side becomes wasted, the protruded tongue may curve strikingly toward the atrophic side, assuming a sickle shape. In bilateral paralysis, the patient may be able to protrude the tongue only slightly or not at all. Unilateral tongue atrophy can sometimes be confirmed by palpation.
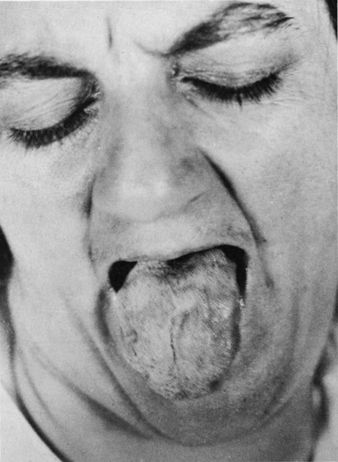
FIGURE 20.4 Nuclear paralysis of muscles supplied by the hypoglossal nerve. Atrophy and fasciculations of the tongue in a patient with amyotrophic lateral sclerosis.








