INTRODUCTION
Efficient early detection of cognitive decline and dementia is becoming increasingly important. A large number of screening instruments are available, but they vary greatly in their ease of use, psychometric properties and validity in differing cultural contexts, as well as in the presence of co-morbid conditions. In addition, there is a need for cost-effective screening tests which can be administered to large populations across a variety of mediums (orally, paper and pencil, by mail, by telephone, or by computer).
The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) is a brief questionnaire for the assessment of change in cognition which shows very good psychometric properties, has been validated across multiple cultural contexts, and which can be used in clinical practice as well as in large-scale epidemiological studies.
The IQODE was developed to assess cognitive decline from a pre-morbid level based on informant reports1. The parent instrument was composed of 39 interview questions assessing memory function (acquisition and retrieval) and intelligence (verbal and performance). Informants were asked to rate the magnitude of change over the previous 10 years in these domains. After initial evaluation, the number of items was reduced to 26 which correlated well together and were relatively easy to rate. The questionnaire was formatted for selfcompletion and named IQCODE. In its present form the IQCODE requires each item to be rated on a 5-point scale from 1, ‘much improved’ to 5, ‘much worse’2. The questions are framed in the form: ‘Compared to 10 years ago, how is this person at…’ (e.g. remembering things about family and friends such as occupations, birthdays, addresses, etc.).
A short version of the IQCODE consisting of 16 items has been developed2. It was found to correlate highly (0.98) with the full version and to have equivalent validity against clinical diagnosis. Consequently there is little advantage in using the longer version.
Versions of the IQCODE have been developed and validated in other languages (Chinese, Dutch, Finnish, French, Canadian French, German, Italian, Japanese, Korean, Norwegian, Persian, Polish, Portuguese, Spanish, and Thai) and copies are available for download at cmhr.anu.edu.au/ageing/iqcode.
Other variations on the IQCODE have also been produced, including questionnaires based on shorter3,4 or more flexible5 retrospective time frames, as well as short forms in Spanish6, Chinese7, Portuguese8 and in other languages (which to our knowledge have not been validated).
Scoring the IQCODE involves summing the items and dividing by the number of items, thus producing a measure ranging from 1 to 5, however, some investigators have preferred adding up all items. Norms have been developed by Jorm and Jacomb9 for five-year age groups from 70 to 85+ years, but in practice individual researchers have generally chosen to use an absolute cut-off ranging from 3.3-3.6 in community samples to 3.4-4.0 in patient samples. A practical strategy to choose a cut-off is to identify studies (e.g. in Table 28.1) with characteristics most similar to the target population and select their cut-offs.
The IQCODE is a pen and paper test which takes between 10 and 25 minutes to complete, depending on the form chosen (long/short) and is generally perceived as relatively easy to answer. It can be mailed to informants and could potentially be administered by telephone or by computer (although we are not aware of any validation data with these administration media). The IQCODE can also be used as an alternative screening test when individuals are not able to complete another test such as the Mini-Mental State Examination (MMSE). In a survey of 839 community-based older individuals, Khachaturian et al.10 found 74 subjects who were unable to complete the 3 MS but the IQCODE could be completed by an informant. Seventy-one of these were subsequently diagnosed with dementia. In addition, Cherbuin et al. 11 reviewed the literature to assess the suitability of dementia screening instruments for self-or informantassessment, particularly in an electronic format (local computer or web-based). They concluded that the IQCODE was one of three most
Table 28.1 Performance of the Mini-Mental State Examination (MMSE), and the long and short versions of the IQCODE as a screening test for dementia47-51
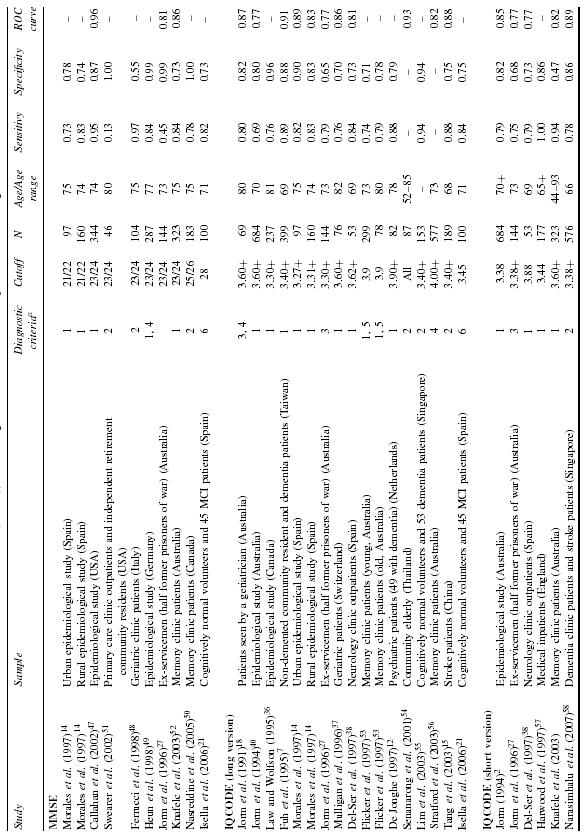
al = DSM-IIIR dementia; 2 = DSM-IV dementia; 3 = ICD-9; 4 = ICD-10 dementia; 5 = Clinical diagnosis; 6 = Mild cognitive impairment (Petersen 1996 criteria).
promising tools and they recommended further validation studies for these delivery platforms.
The IQCODE’s reliability and validity have been extensively researched. A number of studies have assessed the internal consistency of the scale using Cronbach’s alpha. Alpha was found to range between 0.93 and 0.97 across nine studies1,7,9,12-17 which can be regarded as excellent. The stability of scores over short periods was found to be high, with test-retest reliability showing correlations of 0.96 over three days and 0.75 over one year9,18.
Other studies have conducted factor analyses to investigate the factor structure of the IQCODE. They all found a large main factor accounting for 42-73% of the variance which is thought to represent ‘cognitive decline’, while other factors were generally small with the second factor explaining less than 10% of the variance7,9,13,14,17,19.
VALIDATION AGAINST CLINICAL DIAGNOSIS
Many studies have assessed the validity of the IQCODE against clinical diagnosis. Table 28.1 contrasts measures of sensitivity and specificity of the long and short forms of the IQCODE and the MMSE11,20 and shows comparable findings for the two tests, confirming that the IQCODE is a valid screen for dementia. However, moderate correlations between the IQCODE and the MMSE in 15 studies ranging from -0.37 to –0.7820 with a sample size weighted average of -0.58 suggest that these two tests, although largely overlapping, each have some unique variance. As a consequence, a number of studies have investigated whether the concurrent administration and scoring of the IQCODE and the MMSE improves dementia detection. They generally reported somewhat increased sensitivity and/or specificity of the combined tests, but cost-benefits of this combination varied depending on the methodology or the type of sample used20. The IQCODE has also been investigated as a predictor of conversion to mild cognitive impairment over three years and was found to be as sensitive as the MMSE for this population (sensitivity 0.82, specificity 0.71 for a cut-off of 3.19)21.
In addition, the IQCODE has been shown to be a predictor of incident dementia in stroke patients22 and in non-demented hospital inpatients23 over 2-3 years follow-up. However, application of the IQCODE to complex clinical populations should be considered carefully, as one study found that the IQCODE and the MMSE were poor at detecting dementia in a sample of first-ever stroke patients24.
VALIDATION AGAINST NEUROPATHOLOGY AND NEUROIMAGING
Diagnoses of dementia based on post-mortem histological examinations have been compared to pre-mortem IQCODE scores in two studies. Using a cut-off of 3.7 and a neuropathological diagnosis of Alzheimer’s disease, Thomas et al.25 found the IQCODE to have a sensitivity of 73% and a specificity of 75%. While Rockwood et al.26, with a cut-off of 3.42 and a diagnosis of Alzheimer’s disease, vascular or mixed dementia, reported a sensitivity of 97% and a specificity of 33%. Another six studies found associations between neuroimaging measures and the IQCODE. Jorm et al.27 found significant associations between the IQCODE and the width of the third ventricle (r = 0.29), and infarcts in the left (r =
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




