The Internal Carotid Artery
Key Points
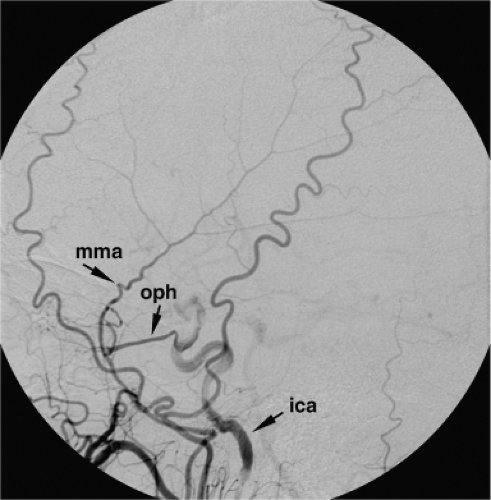
The extracranial and ophthalmic branches of the internal carotid artery exist in a state of actual or potential exchange with distal branches of the external carotid artery. During endovascular interventions one must be ever attentive to the possibility of inadvertent reflux of embolic material in the wrong direction through these routes. The greatest of these risks is with the ophthalmic artery.
Minor or rare variants of the branches of the internal carotid artery are important to recognize in every patient so that catastrophic surgical and endovascular calamities can be avoided.
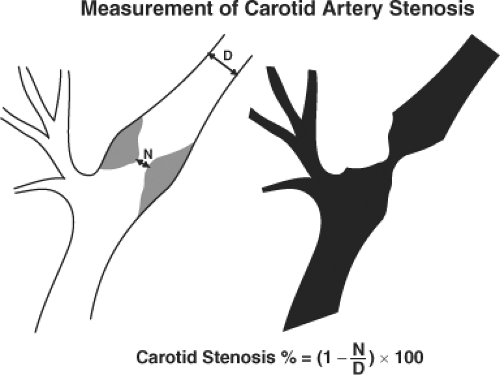
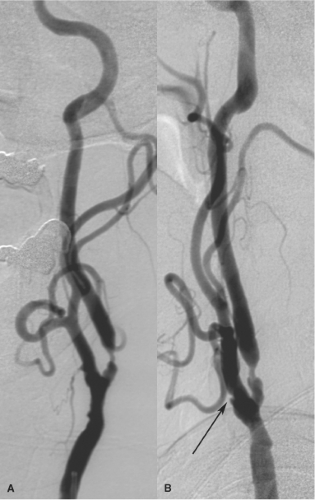
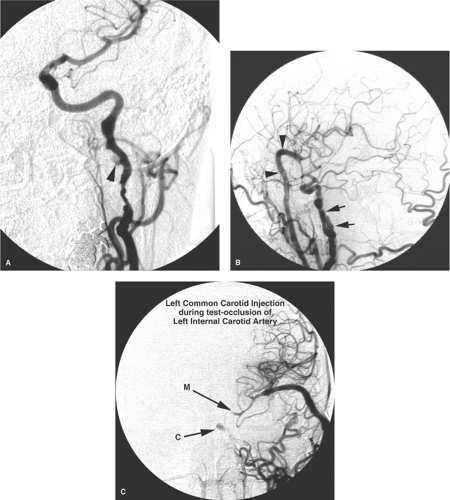
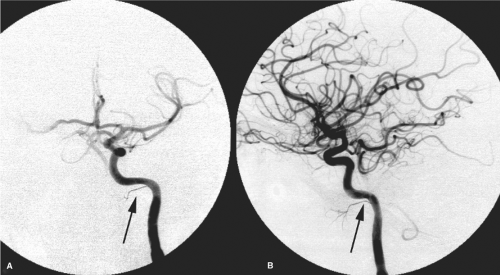
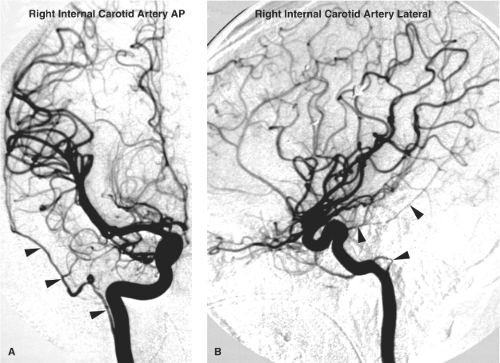
The common carotid artery usually bifurcates at the C3–C4 level into an external carotid artery trunk and an internal carotid artery. The bifurcation may be lower, occasionally being seen as low as T2–T3, although such extremes are rare (Fig. 10-1) (1). Most carotid angiograms are performed on older patients in whom the possibility of atherosclerotic change demands an evaluation of the bifurcation before catheterization of the internal carotid artery (Fig. 10-2). There are other situations in which it is prudent or imperative to perform an angiogram of the common carotid bifurcation before further catheterization or wire manipulation. Some of these are obvious and include questions related to the cervical internal carotid artery itself, for example, dissection, pseudoaneurysm, tumor involvement, and the like (Figs. 10-3–10-6). Others are less obvious but encompass any situation in which the final interpretation of the angiogram might be seriously compromised by the presence of a minimal amount of cervical carotid spasm induced by the wire, for example, evaluation of subtle tumor encasement or traumatic injury (Figs. 10-7–10-9).
Anatomy of the Internal Carotid Artery
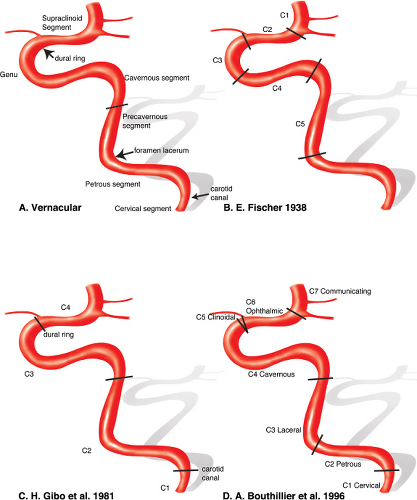
The anatomy of the internal carotid artery is described in segments between the common carotid bifurcation in the neck and the supraclinoidal internal carotid bifurcation. In ascending order, these consist broadly of the cervical, petrous, precavernous, cavernous, paraclinoidal, and supraclinoidal segments (Fig. 10-10).
Cervical Segment
This segment spans the common carotid bifurcation to the skull base. At the base of the skull, the internal carotid artery lies anteromedial to the internal jugular vein with which it shares a neurovascular sheath. This sheath also encloses the IX, X, XI, and XII cranial nerves and postganglionic sympathetic fibers. The pharyngeal wall lies directly anteromedial to the carotid artery. Instrumentation or biopsy of the Rosenmuller fossa carries a risk of internal carotid injury. Such injuries are also more likely in the setting of unsuspected pharyngeal loops of the internal carotid artery, particularly where these loops have a more medial or directly submucosal course (sometimes confusingly referred to as an aberrant carotid artery, not to be confused with the more important variant by the same name taking a route through the middle ear). Parapharyngeal infections may involve the wall of the carotid artery at this level with a risk of pseudoaneurysm formation. At the exocranial ostium of the carotid canal, the carotid sheath splits into two layers. The inner layer becomes the periosteum of the carotid canal; the outer becomes the exocranial periosteum. The cervical segment usually does not have any branches (Fig. 10-11).
Petrous Segment and Laceral Segment
The petrous segment of the internal carotid artery consists of a vertical and a horizontal portion (Fig. 10-12). It enters the skull base at the exocranial opening of the carotid canal, ascends approximately 1 cm, and then turns anteromedially until it enters the intracranial space at the foramen lacerum. The laceral segment is a continuation of the petrous segment ending at the petrolingual ligament (2,3). The artery is accompanied along its course by the sympathetic fibers of the stellate ganglion and by a venous plexus (4,5). Some of the sympathetic fibers part company from the internal carotid artery at the foramen lacerum and form the deep petrosal nerve. The deep petrosal nerve joins the parasympathetic fibers of the greater superficial petrosal nerve to become the Vidian nerve. This nerve travels anteriorly to the pterygopalatine fossa via the Vidian (pterygoid) canal. Angiographically, branches of the petrous internal carotid artery are uncommon, but at least three possible branches are worth remembering: The caroticotympanic branch, the mandibulovidian branch, and the variant stapedial artery.
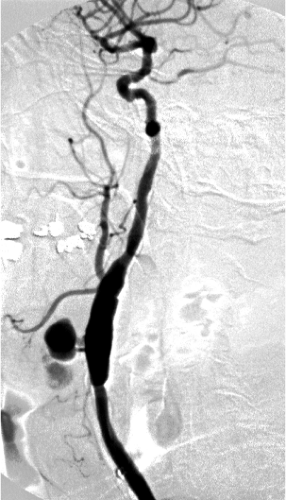 Figure 10-7. Anastomotic breakdown in a left carotid graft. A jet of contrast directed anteriorly fills a multilobulated pseudoaneurysm, which presented as a pulsatile mass. |
Caroticotympanic Branch of the Petrous Internal Carotid Artery
This branch of the petrous internal carotid artery is usually too small to see or is obscured by dense petrous bone. It is a vestige of the course of the hyoid artery. Apart from its role as a vestigial remnant in understanding vascular anomalies of the middle ear, the importance of the caroticotympanic artery lies in its potential supply to vascular tumors of the middle ear.
Mandibulovidian Branch of the Petrous Internal Carotid Artery
This artery is usually too small to see but may enlarge quickly in the setting of occlusive disease (see Fig. 10-13). It is unusual to see this artery in adults. When seen, it is usually in children with a vascular mass of the nasopharynx, for example, a juvenile angiofibroma. It has an origin from the horizontal portion of the petrous carotid artery. The Vidian branch is described as more horizontal and medial than the inferolateral direction of the mandibular branch. The Vidian artery has a straight course along the skull base, anastomosing with branches of the internal maxillary artery anteriorly (5).
Variant Stapedial Artery
Discussed below are the variants of the carotid artery (Figs. 10-14 and 10-15).
Cavernous Segment
From the foramen lacerum, the internal carotid artery ascends vertically and medially to the sella, where it turns anteriorly within the structures of the cavernous sinus. Anteriorly, the carotid artery makes a 180-degree turn, pierces
the proximal dural ring at the level of the anterior clinoid process, and becomes the clinoidal segment. The level of tortuosity of the carotid artery in this region is variable. Children have a straighter course than adults. In older patients, redundant superimposed loops present problems from the point of view of catheterization, visualization of the anatomy of aneurysms, and arterial injury during transphenoidal surgery.
the proximal dural ring at the level of the anterior clinoid process, and becomes the clinoidal segment. The level of tortuosity of the carotid artery in this region is variable. Children have a straighter course than adults. In older patients, redundant superimposed loops present problems from the point of view of catheterization, visualization of the anatomy of aneurysms, and arterial injury during transphenoidal surgery.
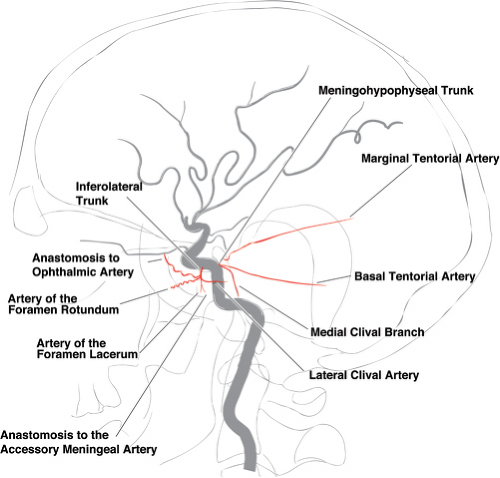
Branches of the juxtasellar internal carotid artery are frequently seen with modern digital technology and may become enlarged in the presence of collateral flow or pathologic conditions (Fig. 10-16). These branches are among the most important for consideration during external carotid artery embolization. They constitute a dangerous system of anastomoses between the external carotid and internal carotid artery systems. Therefore, whether or not they are seen on an initial angiogram, embolization is always done with the cautious assumption that they are present.
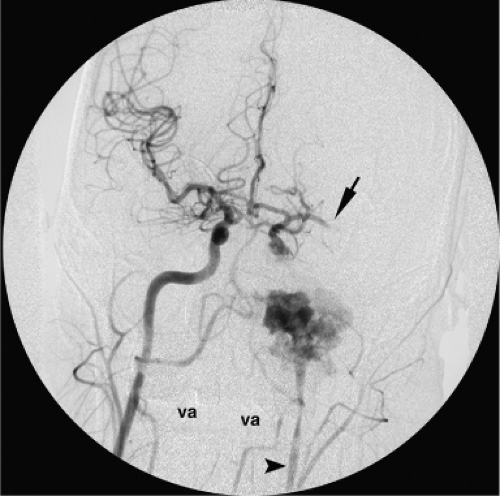
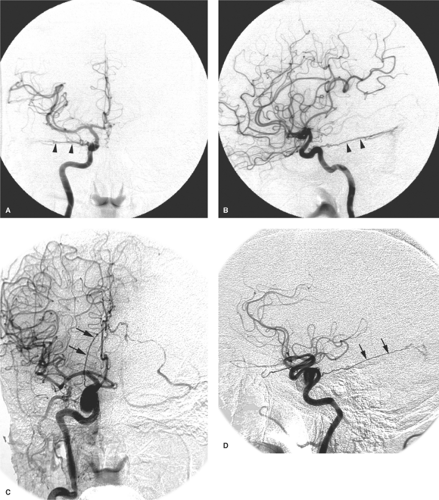
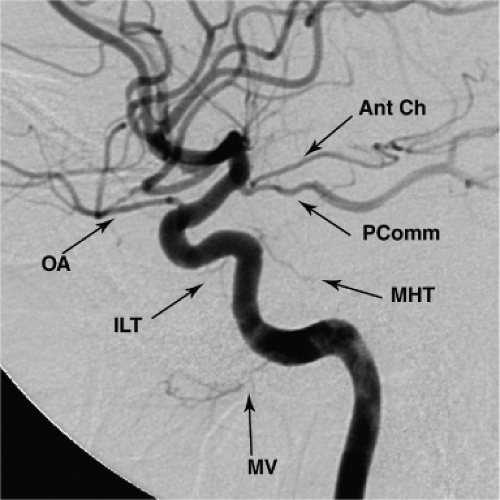
The branches of the cavernous internal carotid artery supply the pituitary gland and the adjacent dura. They have important anastomoses with the distal external carotid artery and with the ophthalmic artery. They play an important role in the arterial component of dural arteriovenous malformations (AVMs). They are sometimes described as being seen as two major trunks: The meningohypophyseal trunk posteriorly and the inferolateral trunk anteriorly and laterally (Figs. 10-16–10-20). The most consistently present branches from this site are as follows.
The Marginal and Basal Tentorial Arteries
The tentorial arteries (Fig. 10-18) from this segment of the internal carotid artery are described as marginal, that is, running medially and superiorly along the margin of the tentorial incisura, or basal, that is, running laterally and inferiorly along the insertion of the tentorium along the petrous ridge.
The marginal artery of the tentorium, regardless of its many possible sites of origin, is sometimes referred to eponymously as the artery of Bernasconi and Cassinari (6). In contrast, the basal tentorial artery does not ascend in the same manner but rather diverges laterally along the course of the tentorial insertion on the petrous ridge. Along the petrous ridge and sigmoid sinus, it has anastomoses with the middle meningeal artery and dural arteries of the posterior fossa.
The Posterior Inferior Hypophyseal Artery
The posteroinferior hypophyseal artery is directed medially from the cavernous segment. It supplies the neurohypophysis and peripheral adenohypophysis of the pituitary gland. It anastomoses with the superior hypophyseal arteries (from the supraclinoidal segment), and with its contralateral
fellow. These branches cause a characteristic early neurohypophyseal blush on carotid angiography. The posteroinferior hypophyseal artery also gives a medial clival branch, which runs near the midline along the clivus to meet the ascending clival branch from the hypoglossal artery (a branch of the neuromeningeal trunk deriving from the ascending pharyngeal artery). This connection explains the occasional visualization of the pituitary blush on ascending pharyngeal artery injections.
fellow. These branches cause a characteristic early neurohypophyseal blush on carotid angiography. The posteroinferior hypophyseal artery also gives a medial clival branch, which runs near the midline along the clivus to meet the ascending clival branch from the hypoglossal artery (a branch of the neuromeningeal trunk deriving from the ascending pharyngeal artery). This connection explains the occasional visualization of the pituitary blush on ascending pharyngeal artery injections.
Lateral Clival Artery
The lateral clival artery gives lateral and inferomedial branches along the course of the superior and inferior petrosal sinuses, respectively (7) (Fig. 10-17).
The Recurrent Artery of the Foramen Lacerum
The recurrent artery of the foramen lacerum is important in clinical practice by virtue of its anastomosis in the foramen lacerum with the carotid branch of the superior pharyngeal branch of the ascending pharyngeal artery.
Persistent Trigeminal Artery
The persistent trigeminal artery is discussed below with carotid basilar anastomoses.
Capsular Arteries of McConnell
The capsular arteries of McConnell in the normal state are rarely if ever seen during angiography. However, they may represent one possible site of cavernous internal carotid artery aneurysm formation. Medially directed aneurysms in this location can occupy the sella and are thought to represent a more serious variant of cavernous aneurysms. Their rupture into the sella can penetrate the diaphragm sellae and cause subarachnoid hemorrhage (Fig. 10-21). Sella-occupying aneurysms may also cause hypopituitarism as the presenting clinical problem.
Inferolateral Trunk
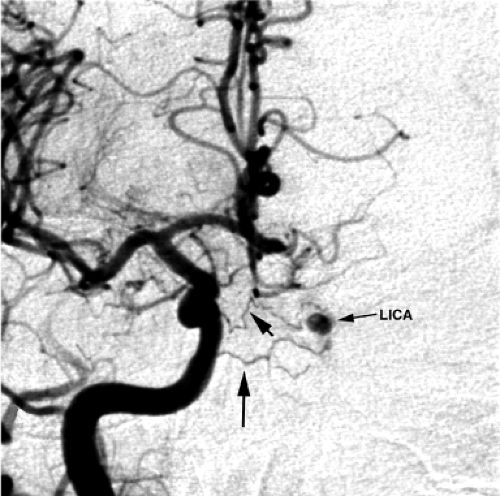
The inferolateral trunk (8), sometimes referred to as the artery of the inferior cavernous sinus (7), is the remnant of the embryonic dorsal ophthalmic artery. It is present in more than 80% of microsurgical dissections (9) (Figs. 10-16–10-23). Its reach includes branches to the tentorium, the superior orbital fissure (potentially connecting with the ophthalmic territory), the foramen rotundum (connecting to the internal maxillary artery), the foramen lacerum (where it can anastomose with the ascending pharyngeal artery), and the foramen ovale. Very rarely, the dorsal ophthalmic artery may persist beyond embryonic life and be the dominant arterial supply to the orbit (Fig. 10-24). When a dual ophthalmic artery supply to the orbit is present (Fig. 10-25), variations in the pattern of anastomosis between the two arteries may be seen, including the possibility of a complete or partial arterial ring around the optic nerve (10).
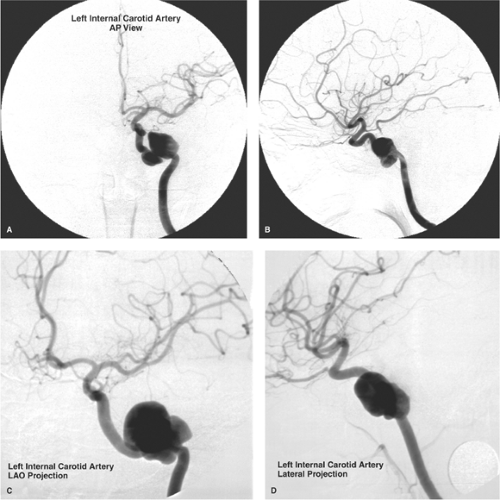
Cavernous Carotid Aneurysms
Aneurysms of the cavernous segment of the internal carotid artery account for approximately 5% of intracranial aneurysms and are more likely to be detected in female patients (Fig. 10-26). Idiopathic aneurysms in this location have a
strong association with hypertension and advancing age, whereas posttraumatic aneurysms or pseudoaneurysms may be seen in any age group. Approximately 50% of cavernous aneurysms occur anteriorly adjacent to the carotid genu, and 16% can be giant aneurysms, that is, greater than 2.5 cm in diameter (11,12). Most cavernous aneurysms seen during angiography are incidental, asymptomatic lesions that usually warrant no further evaluation or treatment (13). Symptoms may develop due to compression of adjacent structures causing cranial nerve deficits, headache, embolic events, or aneurysmal rupture.
strong association with hypertension and advancing age, whereas posttraumatic aneurysms or pseudoaneurysms may be seen in any age group. Approximately 50% of cavernous aneurysms occur anteriorly adjacent to the carotid genu, and 16% can be giant aneurysms, that is, greater than 2.5 cm in diameter (11,12). Most cavernous aneurysms seen during angiography are incidental, asymptomatic lesions that usually warrant no further evaluation or treatment (13). Symptoms may develop due to compression of adjacent structures causing cranial nerve deficits, headache, embolic events, or aneurysmal rupture.
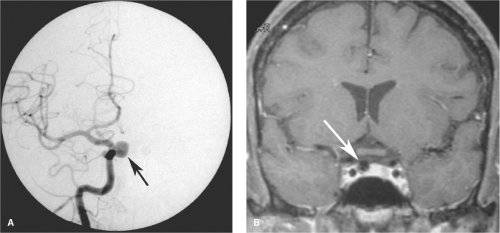 Figure 10-21. (A–B) Intrasellar aneurysm from the cavernous internal carotid artery. A PA angiographic view (A) of a right internal carotid artery injection in a middle-aged female with multiple aneurysms. A medially directed aneurysm from the cavernous internal carotid artery is present (arrow). Aneurysms in this location are thought to correspond with the hypophyseal or capsular branches. The intrasellar location was confirmed on a coronal T1-weighted, gadolinium-enhanced MRI study (B). Although this particular aneurysm was asymptomatic, endovascular treatment was recommended. Intrasellar aneurysms that rupture can leak into the subarachnoid space, causing significantly greater morbidity than rupture of cavernous aneurysms in other positions.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|