Fig. 12.1
One-level SPO. A 34-year-old man suffering AS thoracolumbar kyphosis, one-level SPO was performed at L3/L4. Preoperative and postoperative clinical appearances and lateral radiographs were as shown. The SPO contributed 35° correction. The sharp curve seemed unstabilized
Later, researchers improved the technique to polysegmental posterior wedge osteotomies (SPOs) [7]. It changed from one level to multiple levels and the hinge became to posterior fiber ring. Not too much elongation in each level would happen because one level only obtained about 10° correction, when multilevel osteotomy was done, the correction curve is smooth rather than shape. At the same time, the complications reduce significantly.
Thoracolumbar kyphosis is the most common AS deformity, while this technique is right appropriate for the area. So, for mild AS thoracolumbar kyphotic deformity whose anterior column has not fused and ossified, SPO is the first choice. Though recent study noted that SPOs might lead to correction lost, it is still a safe and effective method [8, 9] (Fig. 12.2d).
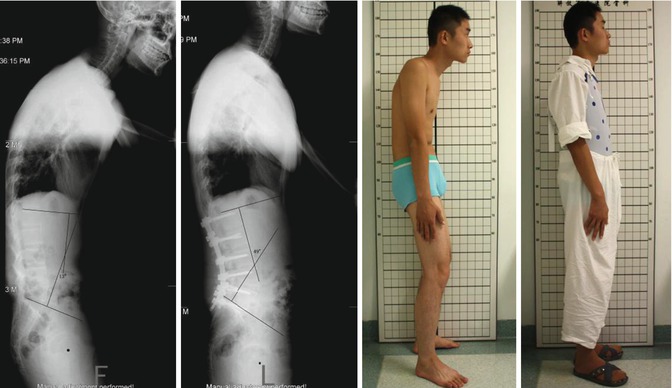
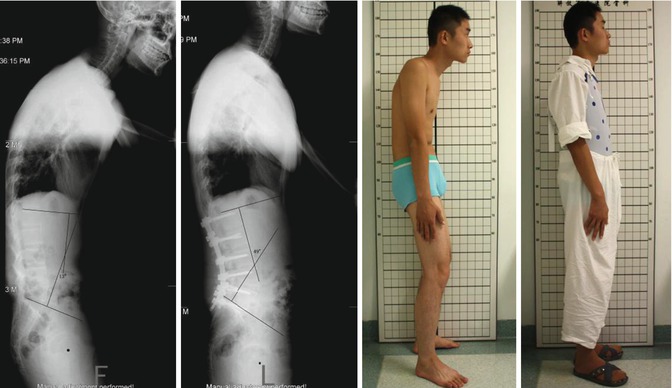
Fig. 12.2
Multilevel SPO (SPOs). A 26-year-old man suffering AS thoracolumbar kyphosis, five-level SPOs was performed at L1/L2/L3/L4/L5/S1. Preoperative and postoperative clinical appearances and lateral radiographs were as shown. Each level obtained about 7° correction, and the total obtained 36°correction. The round and smooth curve was stabilized
12.2.2 Pedicle Subtraction Osteotomy (PSO)
According to three-dimensional reconstruction, parts of the kyphotic spine are fused to a beam; for these cases, we could not obtain a correction by SPO. In this condition, PSO is available (Fig. 12.3).
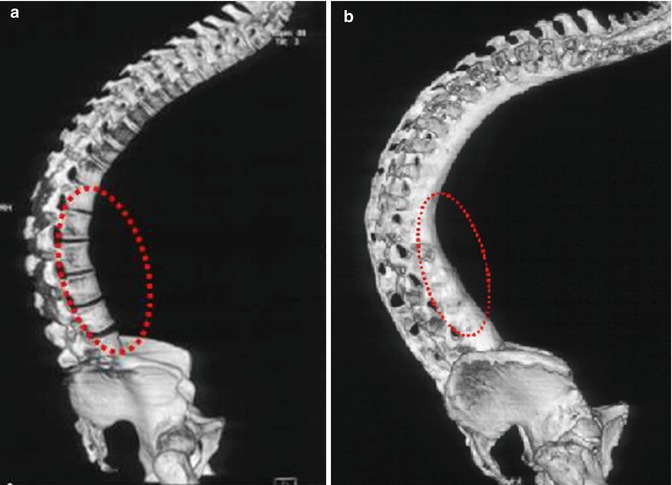
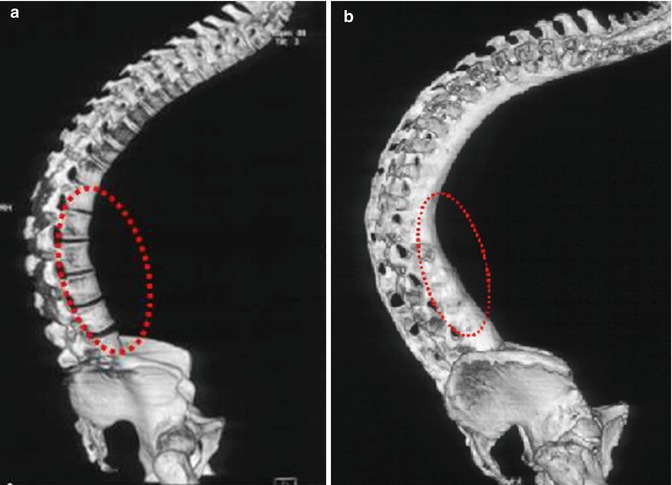
Fig. 12.3
SPOs and PSO. (a) No bony bridge anteriorly, SPOs is feasible. (b) Complete bony bridge anteriorly, PSO is more suitable
Thomasen first described this closing wedge osteotomy in AS in 1985 [10]. The technique makes anterior vertebral cortical bone as hinge, so the anterior column does not need to stretch, leading to little big blood vessel complication. This osteotomy also reserves large area of bone interface, and it is beneficial for stability and bone healing. The most important, it is applied for complete fusion spine in AS because of the three-column osteotomy [11, 12].
Normally, one-level PSO can obtain 30–40° correction and two-level PSO 60–80° correction in lumbar or in thoracolumbar vertebra [13]. An osteotomy at the apex vertebra may achieve a better correction effect. For this reason, the osteotomy site was located at L2 or L3, because L3 is the apex of the lumbar spine. In addition, L2 and L3 are usually located below the conus medullaris, which means osteotomy can be performed safely. We do not perform spinal osteotomy at L5, two important reasons are that L5 is not the apex vertebrae of lumbar lordosis and it brings difficulty to exposure and instrumentation. If two-level PSO are needed, L1/L3 and T12/L2 are common choices. The upper vertebral osteotomy (T12 or L1) can correct thoracolumbar kyphosis to straight, whereas the lower vertebral osteotomy (L2 or L3) can correct the straight to lumbar lordosis.
12.3 Classification and Surgical Decision Making
Based on lots of cases, we divided AS kyphosis into four types according to the location of apex of kyphosis: lumbar (type 1), thoracolumbar (type 2), thoracic (type 3), and cervical (type 4) (Table 12.1, Fig. 12.4). Moreover, surgical decision making was performed (Table 12.2) [14].
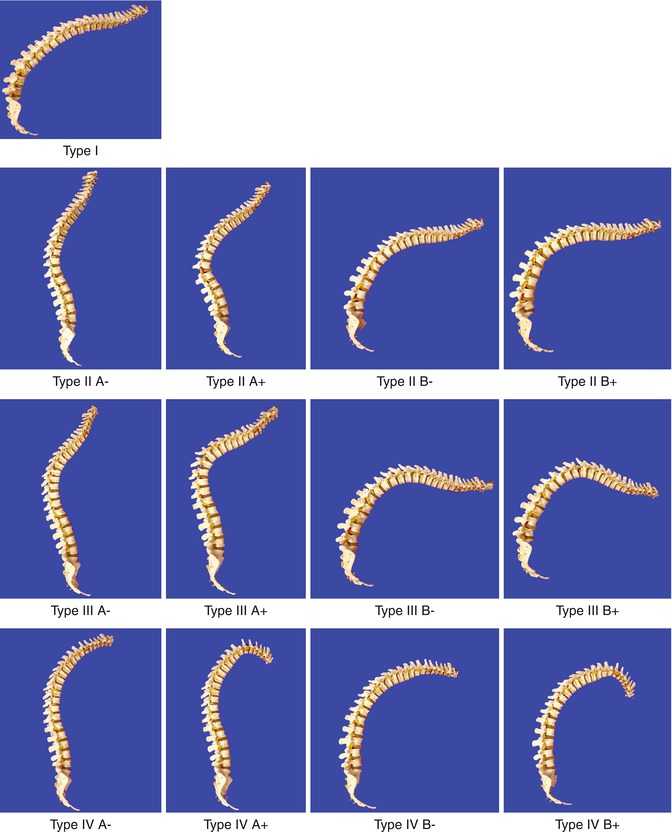
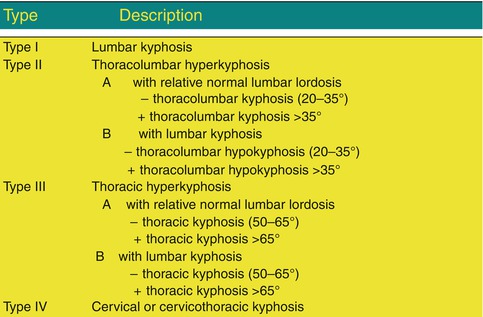
Table 12.1
Classification of AS kyphosis
Type I lumbar kyphosis |
Type II thoracolumbar kyphosis |
A with relative normal lumbar lordosis |
− with little hyperkyphosis (20–35°) |
+ with large hyperkyphosis >40° |
B with lumbar kyphosis |
− with little hypokyphosis (20–35°) |
+ with large hypokyphosis >40° |
Type III thoracic kyphosis |
A with relative normal lumbar lordosis |
− with little thoracic hyperkyphosis (50–65°) |
+ with large thoracic hyperkyphosis >65° |
B with lumbar kyphosis |
− with little thoracic hyperkyphosis (50–65°) |
+ with large thoracic hyperkyphosis >65° |
Type IV cervical kyphosis |
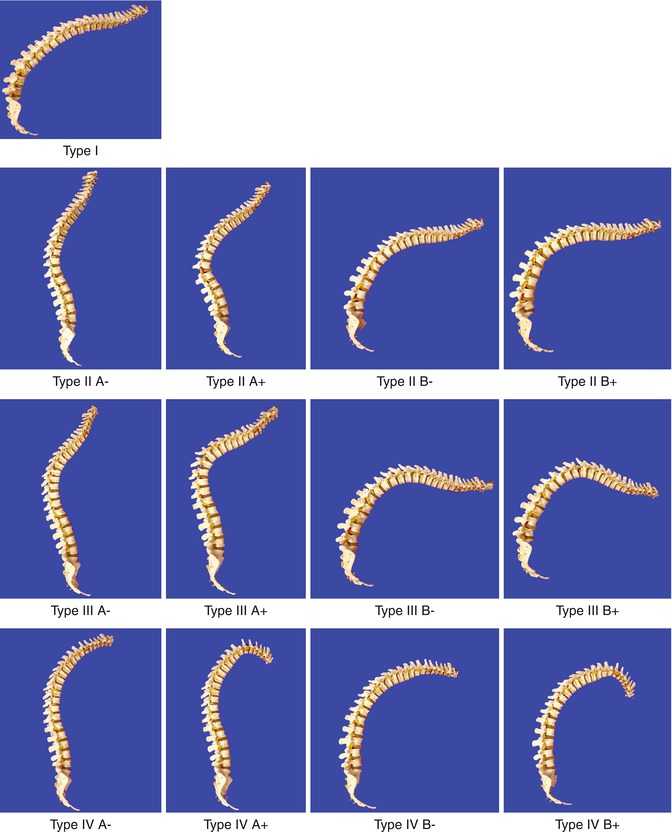
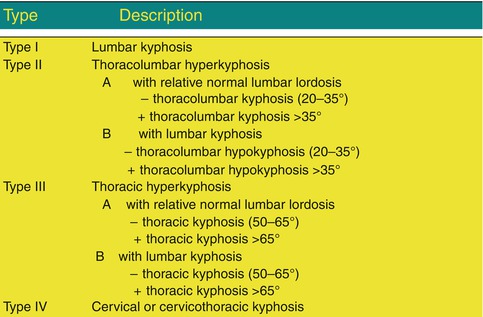
Fig. 12.4
AS classification
Table 12.2
Surgical decision making according to classification
Type | Surgical plan |
|---|---|
Type II A− | Non-operative or thoracolumbar SPOs |
Type II A+ | L2 or L3 osteotomy |
Type II B− | L3 or L2 osteotomy +/or thoracolumbar SPOs |
Type II B+ | Two levels spinal osteotomy(L1 + L3 or T12 + L2) |
Type III A− | Non-operative or thoracic SPOs |
Type III A+ | L2 spinal osteotomy |
Type III B− | L2 +/or T12 osteotomy |
Type III B+ | L2 + T12 osteotomy |
Type IV | C7 spinal osteotomy |
In general, with the same curvature, the shorter distance from hip axis to the apex of kyphosis, the larger impact to the sagittal balance due to leverage effect. How to design the distribution of correction degree is very important. Without the restriction of ribs, without the risk of spinal cord compression, and with more ability to reconstruct sagittal balance due to leverage effect [15, 16]. We prefer to perform the osteotomy more aggressively in the lumbar and thoracolumbar region.
We do not recommend performing PSO at spinal cord regions only if we have to do. First, the reconstruction of lumbar lordosis is necessary, because the loss of lumbar lordosis is usually coexistent with hyperkyphosis of thoracolumbar and thoracic spine. Second, spinal osteotomy at nonspinal cord regions is relative safety, and the degrees of osteotomy at the lumbar region should be as large as possible to retrieve the global alignment.
12.4 Thoracolumbar Kyphotic Deformity Design
12.4.1 Sagittal Balance
For most adults with a well-balanced spine, the center of gravity (CG) of the trunk is over the hip axis (HA) and directly under the promontory of the sacrum when the pelvis is in a neutral position [17, 18]. In spinal deformity, compensatory mechanisms still tend to locate the CG onto the HA by pelvic rotation in order to maintain a balanced upright posture with a minimum of muscular energy expenditure. This leads to the promontory of the sacrum to move either to behind or in front of the HA. Thus, on one hand, we can use the line connecting the sacrum promontory and the HA as the pelvic neutral positional line. On the other hand, we can consider the vertical angle of the line connecting the sacrum promontory and the HA as the pelvic rotation angle (PRA).
For fixed thoracolumbar kyphosis caused by AS, the CG is anterior to normal, which means that the CG will fall in front of the HA. However, this position does not occur, as it appears that the body rotates the pelvis backward to relocate the CG on the HA by extension of the hips and flexion of the knees for balance and less energy expenditure (Fig. 12.5a) [16, 19]. When an insufficient PSO angle was achieved, the CG was relocated, although the pelvis did not need to rotate backward to the same degree as before; it was still in a backward rotation (Fig. 12.5b). If an excessive PSO angle was achieved, then the pelvis would rotate forward to compensate for locating CG on the HA (Fig. 12.5c). Therefore, we could only obtain a pelvic neutral position when the CG was relocated on the line connecting the sacrum promontory and the HA or named pelvic neutral positional line (Fig. 12.5d). So, all left we should do was to find CG.
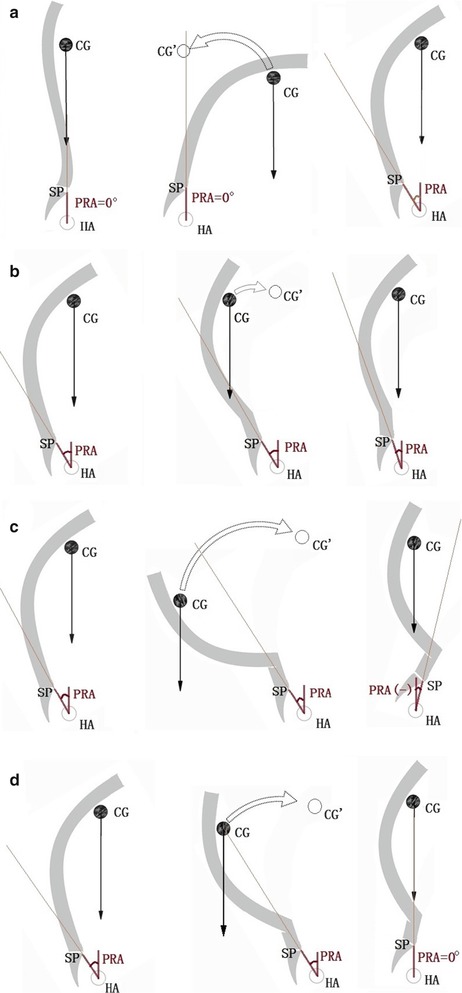
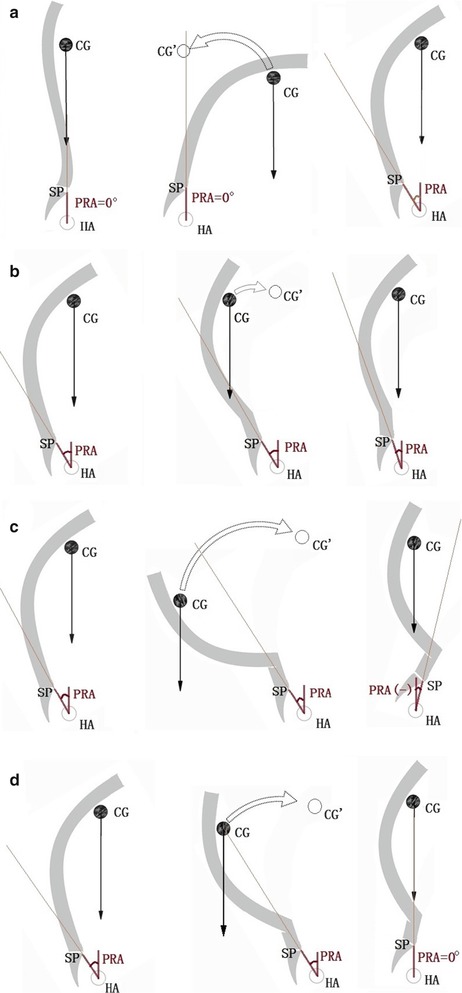
Fig. 12.5
(a) (1) For a healthy adult, CG and SP are on HA; (2) For AS kyphosis, CG is anterior compared to normal in the pelvic neutral position, and is not a stable state; (3) Pelvis rotated backward, then CG fell on HA again, whereas SP was behind HA. (b) Insufficient PSO angle. (1) Preoperatively, CG is on HA, whereas SP is behind HA, so pelvis is rotated backward; (2) after PSO, CG was behind HA, and this was not a stable state; (3) postoperatively, CG was on HA, whereas SP was still behind HA in spite of moving forward. (c) Excess PSO angle. (1) Preoperatively, CG was on HA, whereas SP was behind HA, so pelvis was in backward rotation; (2) after PSO, CG was behind HA, and was not a stable state; (3) postoperatively, CG was on HA, whereas SP was in front of HA because of rotating forward too much. (d) Adequate PSO angle. (1) Preoperatively, CG is on HA, whereas SP was behind HA, so pelvis was in backward rotation; (2) after PSO, CG was behind HA, and was not a stable state; (3) postoperatively, CG was on HA, and likewise SP was on HA as a result of rotating forward properly. Abbreviations: CG center of gravity of the trunk, SP sacrum promontory, HA hip axis, PRA pelvic rotation angle
How do we find the CG? Usually, it is not feasible to determine the position of the CG because of the irregular shape of the trunk and the irregular distribution of bone, fat, muscles, and internal organs. However, we come up with a different way to deal with this complex problem. To our knowledge, the CG of an irregular object can be obtained by hanging or supporting it in different points and directions, and the CG will be on the point of intersection. According to this Principle of Mechanics, we can use the pre and postoperative HA vertical lines (or CG line) to locate the CG of the trunk (Fig. 12.6a, b).
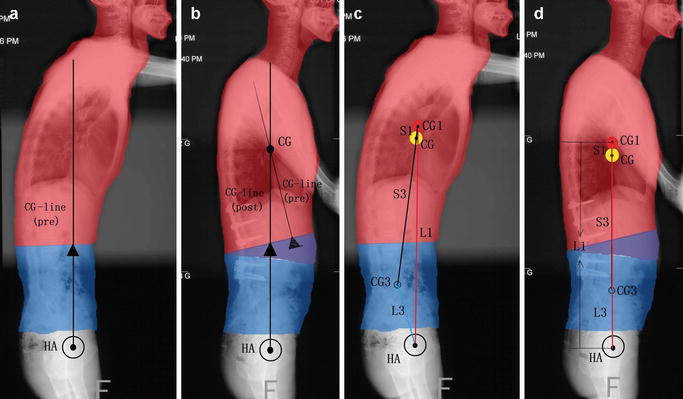
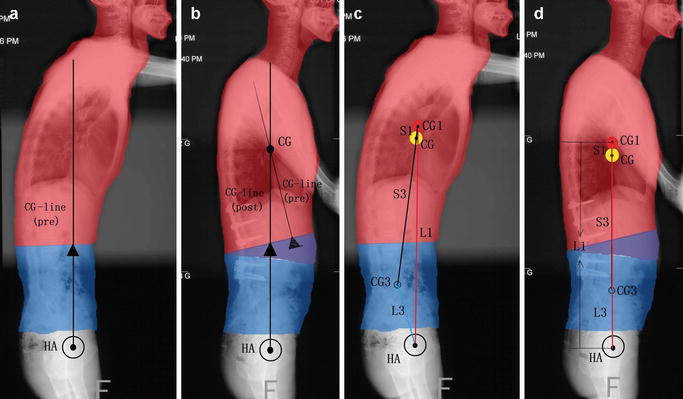
Fig. 12.6




(a) Presurgery and (b) postsurgery. CG center of gravity, is on the crossing point of the preoperative CG-line and the postoperative CG-line. The shorter the distance is between the marker with the two lines, the better marker it is as the center of gravity. (c) Presurgery and (d) postsurgery CG center of gravity of the entire trunk, CG1 center of gravity of the proximal part of the trunk, CG3 center of gravity of the distal part of the trunk. Mass of proximal part > Mass of distal part; Arm L1 > Arm L3; Mass CG1* Arm L1 > > Mass CG3 * Arm L3; S3/S1 = (Mass CG1* Arm L1)/(Mass CG3 * Arm L3), so S3 > > S1. Thus, CG is next to CG1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








