Fig. 1.1
6F femoral sheath
Wires and Catheters
Diagnostic Cerebral Angiography
Diagnostic catheters are usually advanced over a hydrophilic wire. The wire acts as a guide to prevent the catheter tip from damaging vessel walls and/or causing a dissection.
Hydrophilic wires vary from soft and flexible to slightly stiffer. Selection of the wire for a procedure depends on how much wire support is needed to navigate the catheter. With stiffer catheters, there is a greater risk of vessel dissection [1]. Arterial dissections are an uncommon complication with prevalence reported in the literature at around 0.4 % [4].
Typically, a 5-French standard catheter is used for cerebral angiography (4 French in children). Catheters should have good torque control, be soft and nontraumatic, be radiopaque, and have a smooth surface to prevent thrombus formation. A standard angled catheter is the workhorse of most diagnostic cases. However, in cases of tortuous anatomy, more complex-shaped catheters can be used such as Simmons II shaped, Headhunter, or Mikaelsson [5].
Guide Catheter and Microcatheters
For intracranial aneurysm embolization procedures, a large-lumen 6-French guide catheter (Fig. 1.2) or long 6-French sheath is typically used. Once the guide catheter is in position, a microcatheter is advanced under road-mapping guidance over a micro-guidewire into the aneurysm. Subsequently, coils are advanced and detached inside the aneurysm [6]. In tortuous anatomy, a long sheath may be used, in coordination with a guide catheter or an intermediate distal access catheter, and a microcatheter. This system is termed a triaxial system.


Fig. 1.2
6F Envoy guide catheter. Credit: DePuy Companies, used with permission
Microcatheters can be hydrophilic or nonhydrophilic, but only hydrophilic microcatheters are recommended since they are proven to be less thrombogenic [7]. Microcatheters come in different sizes, and in general, the smallest catheter for the desirable coils should be used [1] (Fig. 1.3). The inner diameter of the microcatheter may range in size for coil delivery from 0.015 to 0.025 in., so close attention must be paid to coil size compatibility during aneurysm embolization.
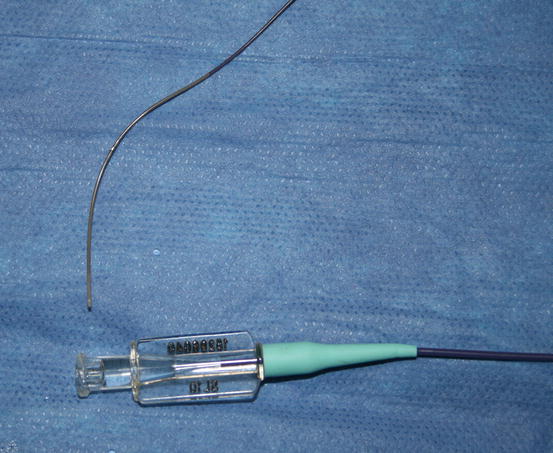
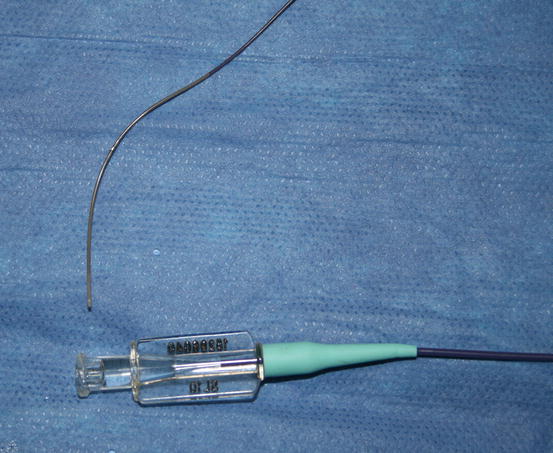
Fig. 1.3
Excelsior® SL-10® microcatheter. Credit: Stryker, used with permission
Coils
Platinum coils for the treatment of brain aneurysms were introduced in the 1990s as an alternative to surgical clipping [8]. Platinum coils consist of a platinum thread looped around a thicker platinum wire. Once deployed inside the aneurysm, they regain their original shape and are subsequently detached from the wire by a low current (Fig. 1.4) or other mechanism.


Fig. 1.4
Low-current detachment system. Credit: Boston Scientific, used with permission
Coils can be “filling,” “framing,” or “finishing.” They have different diameters, stiffness profile, and geometry that influence their stability within the aneurysm [9].
Framing coils are three-dimensionally designed coils to frame the circumference of the aneurysm, while filling coils pack the aneurysm once it has been framed. Finishing coils, on the other hand, are soft coils designed for final packing of the aneurysm and neck [1].
Achieving an adequate packing density of the coils within the aneurysm is one of the most important factors in avoiding aneurysm recanalization [10]. Recanalization and coil compaction are determined by many factors; however, notably, smaller and softer coils generally have a higher risk for coil compaction.
An effort to minimize recanalization led to the introduction of bioactive coils. Bioactive coils consist of platinum coils with adjunctive polymers that have the properties affecting the thrombosis, inflammation, and healing processes within the aneurysm [11]. Theoretically, bioactive coils are expected to produce a more prominent healing response within the aneurysm and therefore result in less recanalization. Longer follow-up, however, is needed for validation [11].
Recently, a randomized trial showed no angiographic difference between Cerecyte coils and bare platinum coils [12].
Liquid Embolic Materials
Liquid embolic material is mainly used for embolization of cerebral or spinal arteriovenous malformations (AVMs) and pial or dural arteriovenous fistulas (AVFs). It is used less frequently for cerebral aneurysms. Most of these materials are supplied in a liquid state and delivered using microcatheters. Currently, there are few liquid embolic agents commercially available.
Ethylene-vinyl alcohol copolymer (Onyx) is supplied by the manufacturer in a liquid form dissolved in an organic solvent, dimethyl sulfoxide (DMSO), with tantalum powder added for radiopacity. Onyx is nonadhesive and has an even flow pattern. When Onyx contacts blood, the DMSO rapidly diffuses causing precipitation and solidification of the polymer [13]. The solidification occurs more slowly than cyanoacrylates, and it usually does not adhere to the walls of the microcatheter, thereby allowing a slower injection and better AVM nidus and/or fistula penetration [13]. Reflux of the Onyx around the distal microcatheter, however, is often encountered the longer the injection of the copolymer, which can make the microcatheter difficult to retrieve.
Cyanoacrylate (n-BCA TRUFILL) is an acrylic agent that polymerizes when it contacts blood or saline solutions. Due to its strong adhesive characteristics, it is possible to cause adhesion between the tip of the microcatheter and the vessel or glue cast [14]. The polymerization rate can be adjusted by varying the concentration of the monomer in Ethiodol or by adding glacial acetic acid to the mixture.
Particulate Embolics
Polyvinyl alcohol particles are small solid particles of various sizes which are radiolucent and need to be mixed with contrast material to make them radiopaque. Particles are commonly used for permanent small-vessel occlusion. They produce occlusion by thrombus formation, and when the particles are too large, they can clog the microcatheter. Particles can be carried out by flow; this means that flow can take them to the lesion or may cause them to land more distally than intended. For this reason, particles are not effective for high-flow fistulas. Embospheres (BioSphere Medical, Rockland, MA) of various sizes may also be used for deliberate small-vessel occlusions in AVMs, tumors, and epistaxis.
Stents
Stent–assisted coiling is used in the setting of a wide-neck aneurysm. Stent-assisted coiling requires the use of dual antiplatelet therapy, and therefore, they are generally used for unruptured cases. Their use in the setting of subarachnoid hemorrhage (SAH) has been described as a viable option in the literature but still remains controversial [15]. Stents or vascular remodeling devices designed for aneurysm treatment are self-expandable nitinol meshes of thin-strut density deployed across the neck aneurysm and followed by coil packing of the aneurysm [16]. They provide more stability to the coil mass by holding it in place, and theoretically, they reduce the possibility of recanalization [16]. Early complications include thromboembolism, and, in a late setting, stent stenosis and occlusion of the parent vessel can rarely occur [17] (Fig. 1.5). These come in open-cell and closed-cell designs. The open-cell design has somewhat more vessel conformity in small vessels, on a turn, and allows for a Y-stent configuration. The closed-cell design has somewhat more protection from the stent herniating into aneurysm or coils herniating through the stent.