4 The neurological examination
Peripheral nervous system
Examination of the peripheral nervous system assumes a stylised approach when adopting the traditional method. This means following a set pattern of: observation and inspection; tone; power; reflexes; sensation; coordination; and gait. This ignores what was stated earlier, namely that the consultation starts long before the patient enters the consultation room.
Before undergoing the formal peripheral assessment it is worth testing for grasp reflexes. This is done by distracting the patient, possibly by engaging in ‘small talk’, and while doing so sliding the hand out, pushing up against the patient’s palm and fingers. Grasp reflex may be as subtle as feeling the fingers of the patient flexing downwards towards the examiner’s sliding fingers. A positive grasp reflex is indicative of contralateral frontal lobe (upper motor neurone) damage. Other frontal lobe signs may include palmar–mental response. This is evoked by applying a noxious stimulus (such as scratching) to the palm of the patient’s hand and observing the movement of the chin (mentalis muscle) on the same side as the scratched hand. This again suggests contralateral frontal lobe damage.
The glabellar tap is elicited by tapping the index finger on the patient’s forehead. It is best achieved by holding the hand above the forehead and tapping the forehead without coming front-on as this movement, equivocal to menace (as described when testing visual fields in Ch 2), may itself evoke a blink response. When testing the glabellar tap the normal response allows up to three blinks. More than three blinks represent a positive response. When testing glabellar tap it is worth reappraising the patient for ptosis, as attention is focused on the eyelids.
Tone
If Parkinson’s disease is considered, then the initial testing of tone by moving the hand up and down at the wrist should be normal early in the disease process. The patient is asked to move their head from side to side, pushing the ear into the shoulder with each turn, at which time the tone increases with ‘cogwheeling’ and ‘lead pipe’ rigidity. This is pathognomic of early Parkinson’s disease.
Power
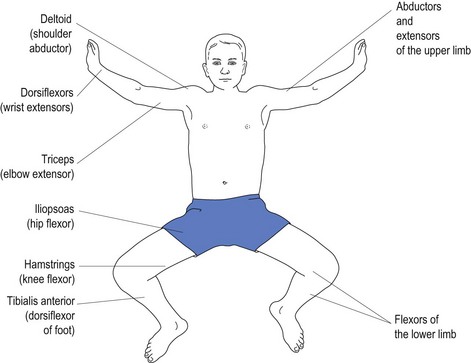
Various conditions affect different muscles. Upper motor neurone weakness, as with stroke, affects the antigravity muscles. Most inexperienced doctors have difficulty remembering which muscles constitute the antigravity muscles (see Fig 4.1).
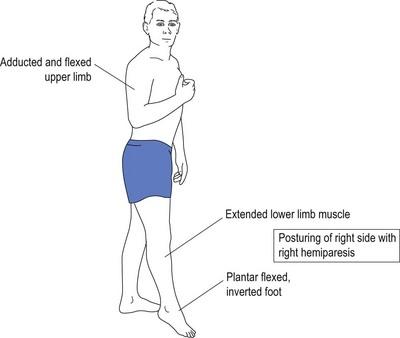
It is because of weakness of the antigravity muscles that the patient with upper motor neurone damage presents with flexion of the upper limbs and extension of the lower limbs. With weakness of the antigravity muscles, the opposing muscles exert their effect causing posturing without counter effect by opposing muscles (see Fig 4.2).
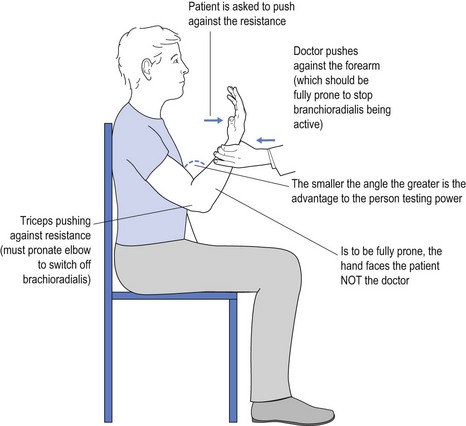
It is obvious that a 60 kg female may have trouble overcoming the strength of a 100 kg male who is engaged in very physical work. One way to overcome this is to use mechanical advantage to test power. An example of this might be to test triceps power by flexing the elbow much more than the traditional 90° (see Fig 4.3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree