The Neuropsychiatry of Head Injury
Simon Fleminger
Head injury ‘imparts at a blow both physical and psychological trauma’,(1) and the consequences are often devastating and enduring.(2) Not infrequently head injury leads to a psychiatric consultation, which will need to take into account the interplay between the brain and its injuries as well as the psychodynamic processes that follow from the injury.
In the immediate aftermath of the head injury, the management rests with the acute surgical and medical team.(3) The psychiatrist is usually not involved at this stage. Nevertheless, to understand the later neuropsychiatric effects of head injury it is first necessary to know what happens to the brain when it is injured.
Neuropathology
Open head injuries
In open head injuries there is penetration of the skull often with considerable destruction of brain tissue local to the trauma, but relatively less at a distance—particularly for lower velocity injuries such as stabbing. Open head injuries may therefore be associated with little, if any, loss of consciousness, which is generally a marker of diffuse brain injury.
Closed head injuries
(a) Contusions
In closed head injuries acceleration/deceleration forces and shearing forces damage the brain. The soft brain moves within its hard bony box and is damaged. Contusion of the brain occurs, ranging from slight localized small vessel bleeding into surrounding tissue to almost complete local destruction of the brain.
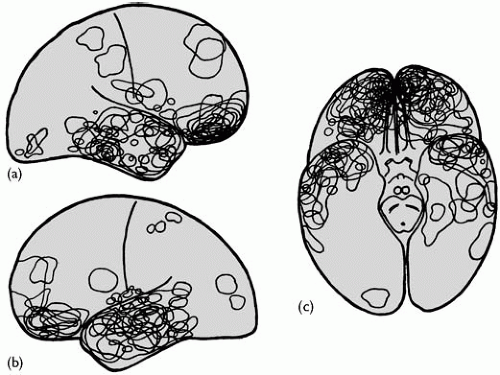
The medial orbital frontal cortex and the tips and undersurface of the temporal lobes are particularly vulnerable to contusions (Fig. 4.1.10.1). The brain becomes traumatized on adjacent bone of the floor of the skull. Contrecoup localization of contusions is sometimes evident.
(b) Intracerebral haemorrhage
Localized haemorrhage into the brain occurs at the site of a contusion. Scattered intracerebral haemorrhages found at the interface between grey and white matter are thought to be associated with diffuse axonal injury (see below). A large isolated haematoma suggests that a blood vessel has ruptured.
In very severe injury haemorrhages are also found round the aqueduct in the brainstem, perhaps caused by distortion of the brainstem as a result of cerebral herniation into the posterior fossa due to raised intracranial pressure. They are associated with prolonged coma or death.
(c) Extradural and subdural haemorrhage
Haemorrhage into the extradural or subdural space will act as a space-occupying lesion and contribute to raised intracranial pressure. The extradural haemorrhage, being under high pressure, can rapidly cause coma and death. The patient may ‘talk and die’, regaining consciousness after the head injury, only to lapse a few hours later into severe coma. Without acute neurosurgical intervention to drain the blood these patients will die.
Subdural haematomas tend to run a subacute course and as such are of more interest to the psychiatrist. They may present with a failure to improve, or fluctuating drowsiness, weeks or months after the head injury. They may regress spontaneously or may require surgical drainage, but they do have a propensity to recur.
(d) Diffuse axonal injury
Diffuse axonal injury occurs in the white matter tracts of the cerebral hemispheres, including the corpus callosum, and the brainstem, particularly the cerebellar peduncles. Axons break up over the course of the first 24 to 48 h following brain trauma with the formation of ‘retraction balls’-globular structures at the end of transected axons.(4)
(e) Oedema and ischaemia
Oedema of damaged brain occurs over the first few hours following brain injury. The resulting raised intracranial pressure compromises the cerebral circulation and results in ischaemia, which may further contribute to brain injury. Cerebral oedema tends to resolve over the course of a few days or weeks.
(f) Neuronal death
Two fairly distinct processes result in neuronal death from traumatic brain injury.(4) Necrotic cell death occurs when there is massive cell disruption either from the direct effects of the trauma on the cell membrane or from anoxia. It is a relatively passive process though may involve toxic effects of high levels of intracellular calcium, excitatory transmitters, and free radicals. On the other hand apoptotic cell death, ‘cell suicide’, is a more active process triggered by various routes including ligand binding to cell death receptors. These activate, for example, endonucleases which attack cellular DNA. Markers of apoptotic cell death are elevated in the days and weeks after injury.
(g) Late effects
Ventriculomegaly may develop over the weeks and months following injury. Often it is the result of atrophy of the white matter of the cerebral hemispheres, usually attributed to diffuse axonal injury, and is associated with atrophy of the corpus callosum. More localized atrophy is observed when contusions resolve to leave a loss of brain tissue.
Of greater importance is hydrocephalus resulting from the residual effects of subarachnoid blood interfering with the normal cerebrospinal fluid flow and preventing it from escaping into the venous system. This may require insertion of a ventriculo-peritoneal shunt to prevent deterioration in cognitive function.
Fractures to the floor of the skull, particularly if they are associated with cerebrospinal fluid leaks, may allow infection into the subarachnoid space, causing meningitis sometimes years after injury. Cerebral abscesses may take months before they become clinically evident.
Loss of consciousness following head injury
The mechanism of loss of consciousness after mild blows to the head is poorly understood. Based on animal work some researchers suggest it is produced by activation of cholinergic nuclei in the pons.(5)
Loss of consciousness lasting for more than a few minutes is likely to damage either cortical areas necessary for consciousness or the subcortical arousal systems. Raised intracranial pressure, partly as a result of compromising cerebral circulation, causes coma. Large or multiple haematomas are likely to be associated with a period of coma, particularly if they are associated with cerebral oedema.
Some patients, however, show prolonged coma with little to be found on brain scan apart from some evidence of generalized cerebral oedema. In these patients, diffuse axonal injury may be the cause of their coma, possibly by damaging the white matter tracts that carry arousal signals from the brainstem to the cortex.
Remember that the head injury may have been caused by an accident triggered by a loss of consciousness, for example, due to hypoglycaemia, alcohol intoxication, or an epileptic fit. Systemic effects (e.g. hypoxaemia or fat emboli) may exacerbate unconsciousness due to head trauma, as may drug intoxication.
Head injury severity
It is surprisingly difficult to predict the degree of brain injury from the size of the blow to the head. Some patients after a severe blow to the head sustain little injury to the brain. Others will suffer severe brain injury associated with prolonged unconsciousness, merely as a result of hitting their head on the ground by falling over from the standing position. Perhaps in the very occasional case significant brain injury occurs when there is no, or only momentary, loss of consciousness (see post-concussion syndrome below). The presence of a skull fracture says little about the severity of the brain injury incurred.
There are several clinical indicators of head injury severity (Box 4.1.10.1). Of these the duration of retrograde amnesia is probably the least valuable: it correlates very poorly with head injury severity.
Box 4.1.10.1 Clinical indicators of head injury severity
The duration of retrograde amnesia—the period leading up to the injury for which memories have been lost. Tends to shrink as the patient recovers.
The depth of unconsciousness as assessed by the worst score on the Glasgow Coma Scale—a score of 3 indicates absent responses with severe coma, 15 is normal consciousness.
The duration of coma—this may be difficult to ascertain because of routine sedation and ventilation following severe head injuries.
Neurological evidence of cerebral injury—abnormality on neuroimaging or EEG.
The duration of post-traumatic amnesia—interval between injury and the return of normal day-to-day memories.
The duration of post-traumatic amnesia is probably the best marker of outcome,(6) and is particularly useful because it can be assessed retrospectively. Most patients with a post-traumatic amnesia of less than 1 week will be left with little if any disability, while a duration of more than 1 month indicates that there is likely to be enduring and significant disability.
Predictors of a worse outcome after head injury are a previous head injury, older age, APOE e4 positive status, and alcohol dependence.
There is no universally accepted classification of head injury severity. However, the most widely used grading system is based on the lowest rating of the Glasgow Coma Scale (GCS)(7) following injury.
Mild: GCS score 13 to 15. Likely to be associated with a loss of consciousness of less than 30 min and a post-traumatic amnesia of less than 24 h. There must be clinical evidence of concussion.
Moderate: GCS score 9 to 12. Likely to be associated with a loss of consciousness of more than a few minutes but less than 6 h and a post-traumatic amnesia of more than 1 day but less than 2 weeks.
Severe: GCS score 3 to 8. Likely to be associated with a loss of consciousness of more than 6 h or a post-traumatic amnesia of more than 2 weeks.
Epidemiology
On average 200-300/100000 population attend hospital with a head injury every year.(8) About one-sixth of those attending hospital will be admitted. This reflects the fact that about 80 per cent of head injuries are mild, 10 per cent moderate, and 10 per cent severe.
At greatest risk are 15- to 25-year-olds. The sex ratio is about two to three males to one female. Risk factors include alcohol misuse as well as lower socio-economic class. Road traffic accidents are the largest single cause of head injury in most civilian cohorts, followed by assaults and falls. A significant proportion will sustain their head injury as a result of deliberate self-harm.
The prevalence rate for those experiencing considerable disability as a result of head injury is in the order of 100 per 100 000.
Investigations
Neuroimaging
In the emergency room or on the trauma unit CT brain scanning is generally the preferred investigation, with its faster acquisition time and good visualization of subdural and extradural haematomas.
For later neuropsychiatric assessment magnetic resonance imaging (MRI) is preferred.(9) Cerebral contusions are often found near the bone-brain interface (see above) where the image quality of CT is reduced because of imaging artefacts from the adjacent bone. MRI has no such limitation and generally has better sensitivity and anatomical definition. MRI is able to detect, on T2-weighted images, changes in signal associated with a diffuse axonal injury when the white matter would have appeared normal on CT brain imaging. Gradient echo MRI sequences should be performed to detect haemosiderin deposits from old small traumatic haemorrhages.
Despite its greater sensitivity a normal MRI does not rule out significant brain injury. On the other hand, particularly in the elderly, MRI may detect abnormalities unrelated to the head injury. It may not be possible to perform an MRI scan if there is magnetic material present in the body (e.g. a pacemaker).
The MRI scan can be normal and yet functional imaging of cerebral metabolism using single-photon emission computed tomography or positron-emission tomography will detect abnormalities. In general, changes on functional imaging correlate better with neuropsychological test performance than do lesions found on structural imaging.(10) However, abnormalities on functional imaging are not necessarily due to brain injury. Hypometabolism may be seen in mental illness without brain injury, for example in depression. Marked hypometabolism on positron-emission tomography imaging has been observed in a man with cognitive impairment occurring immediately after a psychological trauma.(11) He had sustained no head injury.
Electroencephalography
Electroencephalography (EEG) may be useful in the investigation of a deteriorating conscious level or unexpectedly prolonged unconsciousness, and in the investigation of unusual behavioural disturbances that may be attributable to epilepsy. However, EEG is not a good predictor of post-traumatic epilepsy and is generally not useful as a guide to prognosis.
Neuropsychological assessment
A neuropsychological assessment is an invaluable accompaniment to the psychiatric history and examination, and good liaison with the neuropsychologist is essential. Areas of impaired performance can be documented and quantified. This is often useful as a baseline for future assessments and to guide rehabilitation.
The National Adult Reading Test, for people whose first language is English, gives a good estimate of pre-injury IQ.(12) This can then be compared with the present performance on cognitive testing, to estimate the impairment produced by the head injury.
Subtle neuropsychological impairments, which are often not obvious clinically, suggest that the patient may have more problems when they return to work than would otherwise have been expected. On the other hand, if there is clinical evidence of underperformance, and yet standard neuropsychological test results are normal, then it is particularly important that executive function is tested.(13)
Function and health
Psychological symptoms far outstrip neurophysical symptoms (e.g. hemiparesis or dysarthria) as determinants of chronic disability and suffering, both of the patient and their carer, following brain injury.
The ideas encapsulated in the International Classification of Functioning, Disability and Health (ICF) (http://www3.who.int/icf/icftemplate.cfm) are important for understanding recovery from brain injury. ICF is so named because it wishes to emphasize health and functioning by moving away from a dichotomous distinction between those who are healthy and those who are disabled. ICF is a development of the earlier classification ICIDH based on:
Impairments—abnormalities of structure, or physiological or psychological function.
Disability—concerned with performance of activities.
Handicap—reflects limitations fulfilling the person’s normal social role and participation in society. It is very responsive to external, e.g. environmental and societal, factors.
In ICF an individual’s position on the spectrum between health and disability is considered according to (i) functioning and disability and (ii) contextual factors. ICF details the environmental impacts on functioning, e.g. the consequences of living in an area prone to flooding in somebody who is wheelchair dependent. What a person can do in a standard environment (their capacity) is distinguished from what they actually do in their usual environment (their performance).
Recovery and long-term outcome from head injury
Most recovery takes place in the first year. As a general rule, the milder the head injury the sooner the patient achieves the asymptote of their recovery curve. After a mild head injury most patients will have fully recovered within 6 months. After very severe injury significant further improvements in impairment may be seen after the first year post-injury. Neuropsychological impairments tend to continue improving after neurophysical impairments are static. Nevertheless most of the recovery of cognitive function occurs within the first year.(14) Psychiatric symptoms, with their multifactorial aetiology, generally show no simple pattern of recovery.
Improvement in functioning and participation may continue long after the recovery of the underlying impairment has stopped. These further improvements often reflect improved coping strategies and environmental measures to facilitate independence. This will be the focus of the community rehabilitation team as they attempt to help minimize handicap, for example by improving access to local shops. Memory aids may enable the person to return to work. Continuing improvements in participation in social life and work can take place 5 to 10 years after head injury.(15)
But sometimes early gains are made, for example as a result of being in a return-to-work rehabilitation programme, which are subsequently lost over the longer term. In one study,(16) 25 per cent
had deteriorated at 5 years follow-up, with a similar proportion improving compared with how they were at 6 months. Those who deteriorated were more depressed and anxious, had lower self-esteem and had more problems with alcohol than those who improved.
had deteriorated at 5 years follow-up, with a similar proportion improving compared with how they were at 6 months. Those who deteriorated were more depressed and anxious, had lower self-esteem and had more problems with alcohol than those who improved.
In the longer term, decades after injury, it has been suggested that the reduced reserve of the injured brain makes it particularly vulnerable to the effects of ageing. Some studies have found an accelerated cognitive decline compared with age matched controls, for example in head-injured soldiers 25 years later.(17) Head injury may be a risk factor for the development of Alzheimer’s disease, particularly in men.(18) However the evidence, both for an accelerated cognitive decline and for an increased risk of Alzheimer’s disease, is inconsistent.
Aetiology of psychological sequelae
To understand the mental symptoms that follow head injury it is necessary to know about the person who has been injured, what brain injuries they sustained, and the consequences. However, the interaction between these is complex and poorly understood.
Pre-traumatic factors
People who take risks or get into fights are more likely to sustain a head injury; therefore these personality traits, present before injury, are over-represented in head-injury survivors. Young men are at high risk, as are those who have already had a head injury or have cognitive dysfunction.(19)
The poor social adjustment of many patients before the head injury partly explains why so many run into behavioural problems afterwards. But premorbid characteristics do not strongly predict who will develop emotional and behavioural problems. Nevertheless, traumatic brain injury probably has the potential to turn pre-injury personality traits into post-injury personality disorders.
The trauma
The extent of brain injury probably explains less than 10 per cent of the variance in the amount of psychiatric morbidity that follows brain injury.(20) In general, early psychiatric symptoms, within weeks and months of the injury, correlate better with the extent and location of brain injury than do late psychiatric symptoms. Left hemisphere damage seems to be associated with greater psychiatric morbidity. Specific relationships between the location of brain injury and the psychiatric symptoms are discussed below.
But the head injury is also a psychological trauma. Amnesia for the event, as a result of the head injury, protects against post-traumatic stress disorder. However, it is a mistake to believe that amnesia for the event prevents a psychological stress reaction to the event itself.
The meaning of the event may be distressing to the patient.(21) In the case of assaults, the head injury may signal the potential for further assaults. An accident may have been life-threatening and a shocking reminder to the patient that they are mortal. They may feel aggrieved by an employer’s negligent action that caused the accident.
The patient may be amnesic for the event, lacking explicit memories of what happened, but retain implicit memory of what happened. The consequences of these implicit memories may be akin to that observed in one of Claperède’s amnesic patients.(22) The doctor shook the patient’s hand, pricking it while doing so with a concealed drawing pin. The next day the patient could not remember having met the doctor, but flinched from shaking his hand when it was offered.
They may have islets of intact memories that may be extremely frightening.(23)
Post-traumatic factors
Post-traumatic factors deserve special attention because they are most likely to be amenable to intervention. The psychiatrist needs to consider the patient’s reaction to any disability, as well as the consequences of the disability on the role of the patient in the family and society. There may be reinforcing cycles of maladaptive behaviour, and compensation claims may complicate the picture.
Cognitive impairment
Cognitive impairment correlates with measures of head injury severity better than any of the other mental sequelae. For example, there is a strong correlation between the duration of post-traumatic amnesia and the severity of cognitive impairment.
Attention and concentration
Non-specific cognitive impairments include slowness and reduced concentration. The severely injured patient is likely to be stimulus bound, i.e. responding to each and every stimulus they are exposed to in a rather concrete way. At the same time they may show perseveration, with previous responses inappropriately interfering with the answers to subsequent questions, or when the topic of a conversation has been changed.
Dysexecutive syndrome
More specific impairments, generally referred to as the dysexecutive syndrome, result from a disturbance of the executive system responsible for organizing, planning, scheduling, prioritizing, and monitoring cognitive activities.(24) In some patients with isolated medial orbito-frontal lesions or dorso-lateral prefrontal lesions, the dysexecutive syndrome may stand alone. Disturbance of the executive system also results in difficulties in attending to two things at once, and distractibility.
Patients with the dysexecutive syndrome may be much more impaired in everyday life than is predicted by their performance on standard neuropsychological tests. They can manage with the clear instructions of the well-structured and constrained test situation. But in the real world these are absent; priorities have to be set, a strategy planned, decisions taken, and the unexpected dealt with, all without guidance. In the real world, impairment of the executive system may be catastrophic. Tests of the dysexecutive syndrome have been developed in order to be better predictors of these reallife problems. (13)
Memory impairment
Memory impairment is perhaps the most common cognitive impairment that follows head injury, and can be very disabling.(25) People will have problems remembering where they put things, what to do next, how to get home from the shops, or what they did
yesterday. Anterograde amnesia refers to these enduring problems laying down new memories, and must be distinguished from retrograde and post-traumatic amnesia (see Box 4.1.10.1).
yesterday. Anterograde amnesia refers to these enduring problems laying down new memories, and must be distinguished from retrograde and post-traumatic amnesia (see Box 4.1.10.1).
No consistent pattern of brain injury is associated with anterograde amnesia and it seems likely that it is the combined damage to several areas which causes the amnesia. Frontal injury may be particularly implicated perhaps by interfering with the executive processes required for normal memory, for example in memory retrieval. As with most amnesic states the amnesia following brain injury is for explicit memories, namely those which are consciously remembered. Implicit memory, for example remembering and learning a motor skill, is relatively well preserved.
Anterograde amnesia is often characterized by distortions and inaccurate recall with poor monitoring and insight. Confabulations are often seen.
Communication
Dysphasia is quite common after head injury, and may be rather different from that seen after stroke. The more diffuse and widespread injury of traumatic brain injury results in additional cognitive impairments which colour the picture. Monitoring of language errors is often particularly poor and the patient may demonstrate a jargon aphasia such that they are apparently unaware that their speech is completely incomprehensible. Dysphasia often continues to improve even many years post-injury.(26)
Dysprosody, in which the normal rhythms and intonations of speech are lost, is also seen, more so after right hemisphere damage. This interferes with social communication because the voice sounds flat and fails to convey emotion. Social communication is disrupted for other reasons, for example the patient fails in the turn-taking necessary for normal conversation. Word-finding difficulties are common.
Visuospatial impairments
Visuospatial impairments may contribute to spatial disorientation. Visual agnosia is easy to miss in someone with quite widespread cognitive impairments. Hemi-neglect can be troublesome.
Personality change
Personality change after head injury results in more suffering than any other single sequel.(27,28) In general, personality change goes hand in hand with cognitive impairment. However, a severe personality change is occasionally found in somebody with almost no impairment of cognitive function. Normal test scores for memory and intellect do not rule out brain injury as a cause of personality change after head injury.
Aetiology
It is not easy to predict who will develop a change in personality after head injury. Sometimes a personality trait present before the injury becomes much more troublesome, but often there is no obvious predisposition. The site of the brain injury may play a role.(29) Lesions of the medial and lateral surfaces of the frontal lobe can produce impairments of drive. Whereas orbito-frontal lesions, on the undersurface of the frontal lobe, may cause a more troublesome personality change with impairments in social behaviour.
Post-traumatic factors also need to be considered. Some patients seem to learn maladaptive patterns of behaviour; for example the response of the carers may unwittingly reinforce unwanted behaviours. Chronic mental illness, aggravated by chronic psychosocial stressors, may be manifest as personality change. Dependence on drugs, particularly alcohol, frequently confounds the picture.
Characteristics of the personality change
Changes in personality(27) include apathy and impairment of motivation and ambition. Patients are often described as childish; this covers a range of traits including impulsivity, poor tolerance of frustration, being demanding and self-centred, and generally lacking the ability to take on the adult role in terms of independent decision-making. Patients may be fatuous and facetious. Antisocial behaviours (see below) and disinhibition are severe handicaps that make integration back into the community difficult. Sexual disinhibition of any type is particularly worrisome. A spectrum of severity is seen, ranging from being inappropriately flirtatious through to indiscriminate sexual assaults. Head injury is probably a risk factor for borderline personality disorder.(30)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree