The Posterior Cerebral Artery
Key Points
The vessels along the basilar trunk and at the basilar apex are delicate and can be easily perforated or injured with a wire or microcatheter.
The proximal segment of the posterior cerebral artery runs in the perimesencephalic cistern, but so do many other smaller parallel arteries. A wire may look on roadmap as though it is in the posterior cerebral artery but may actually be in a much smaller vessel. Be attentive to what the tip of the wire might be telling you and if there is inexplicable difficulty in advancing the wire, reconsider where you might be.
The embryologic origin of the posterior cerebral artery is from the internal carotid artery, but by the time of full development, the dominant supply to the posterior cerebral artery is usually from the basilar artery (1). A fetal posterior communicating artery configuration implies origin of posterior cerebral artery flow from the internal carotid artery.
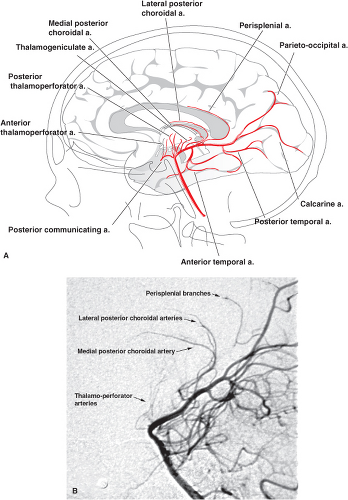
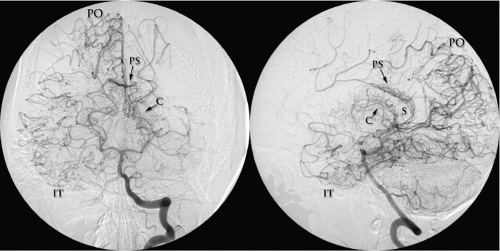
The posterior cerebral artery serves the posterior cerebral hemisphere, thalamus, midbrain, and structures in the walls of the third ventricle and choroidal fissure (Figs. 13-1–13-3). Vascular injury to the posterior cerebral artery or its branches causes a range of debilitating deficits, of which the most severe are those related to the realm of vision. These include functions of a higher order for cortical and subcortical integration of visual perception, interhemispheric integration of visual fields, and relay of visual information to the visual association cortex. Ocular functions served by the posterior cerebral artery include many aspects of eye movement, pupillary reflexes, and eye coordination. Other sites of injury to the posterior cerebral artery may result in devastating neurologic syndromes related to thalamic infarction. Other deficits relate to disruption of afferent pathways in the medial lemniscus and of efferent pathways in the corticospinal tracts. Alterations in levels of arousal and consciousness occur with involvement of the midbrain reticular activating system; memory and endocrine disturbances occur with involvement of the hippocampal and hypothalamic vascular supply.
Segmental Nomenclature
Various shorthand schemes for segmental description of the posterior cerebral artery have been proposed, two of which are most commonly used. A descriptive scheme (2) identifies:
The peduncular segment coursing around the peduncle and bisected by the posterior communicating artery (Fig. 13-4).
The ambient segment lying between the midbrain and the hippocampal gyrus.
The quadrigeminal segment running in the cistern of that name.
More commonly, a symbolic scheme is used (3,4,5,6), wherein the P1 segment extends from the basilar tip to the posterior communicating artery insertion, the P2 segment extends from there to the back of the midbrain, and the P3 segment runs through the lateral aspect of the quadrigeminal cistern around the pulvinar and divides into named branches at the anterior end of the calcarine fissure. The patterns of the proximal branches of the posterior cerebral artery vary and cannot always be exclusively assigned to one segment or another.
Herniation Through the Tentorial Incisura
As the posterior cerebral artery and some of its circumflex branches curve around the midbrain, they course parallel and inferior to the basal vein of Rosenthal and to the geniculate bodies. The posterior cerebral artery is separated from the superior cerebellar artery below by the oculomotor nerve medially and the trochlear nerve laterally. Its usual position is superomedial to the tentorium. In the setting of severe asymmetric mass effect or temporal lobe herniation, the midbrain may become compressed against the tentorium. This causes a classically described indentation in the midbrain contralateral to the mass effect, the Kernohan notch (7), with an occlusion of the interposed posterior cerebral artery or its branches. Therefore, the clinical phenomenon of a “false localizing sign” occurs with hemiparesis ipsilateral to the side of the tumor or mass lesion. In addition to occlusion of the contralateral posterior cerebral artery by compression between the midbrain and tentorium, occlusion of the posterior cerebral artery ipsilateral to the side of mass effect may occur as well. This can happen when this vessel or its branches are stretched around the tentorial edge (8,9).
Posterior Cerebral Artery Branches
For purposes of description, three broad categories of branches from the posterior cerebral artery are identified (10):
Direct or circumflex perforating branches to the brainstem and thalamus
Ventricular branches winding around the brainstem to the choroidal fissure
Cortical branches
Occasionally, in the setting of a meningioma or a dural arteriovenous malformation of the tentorium or posterior fossa, evidence of dural arteries from the posterior cerebral artery may be seen. Small dural branches from the distal cortical and choroidal branches of the artery, normally too small to image angiographically, can supply the falx cerebri (the artery of Davidoff and Schechter) (11,12).
Brainstem and Thalamic Branches of the Posterior Cerebral Artery
These centrally directed branches fall into two patterns:
Direct branches arise from the posterior cerebral artery and enter the brainstem immediately. This pattern includes the posterior thalamoperforator arteries from the P1 segment directed superiorly, the thalamogeniculate arteries from the P2 segment directed superiorly and laterally, and the peduncular perforating branches from the P1 and P2 segments directed centrally into the peduncle and brainstem.
Circumflex branches encircle the brainstem in a course parallel to that of the posterior cerebral artery for variable distances before entering the thalamus or mesencephalon.
Thalamic Perforator Arteries of the Posterior Cerebral Artery
The anterior thalamoperforator arteries, 7 to 10 in number, arise from the superolateral aspect of the posterior communicating arteries. The anterior group of thalamoperforator arteries supplies the thalamic nuclei, the posterior aspect of the optic chiasm, the proximal part of the optic radiations, the posterior hypothalamus, and part of the cerebral peduncle. Having traversed the thalamus, they may give a variable supply to the ependyma of the lateral ventricle and anastomose there with the choroidal vessels (13).
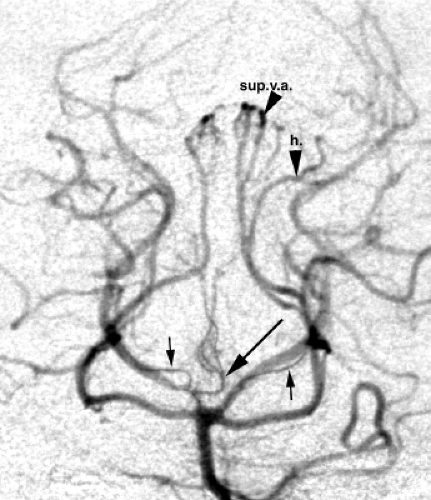
Up to eight posterior thalamoperforator and thalamogeniculate arteries arise from the posterior or posterosuperior aspect of the P1 segment of the posterior cerebral artery. They enter the brain via the posterior perforated substance, the recess of the interpeduncular fossa, and the medial walls of the cerebral peduncles. Together, they supply the thalamus, subthalamic nucleus, and the nuclei and tracts of the upper midbrain, including the substantia nigra, red nucleus, oculomotor and trochlear nuclei, posterior portion of the internal capsule, and the cisternal segment of the oculomotor nerve (2,14,15). Occasionally, posterior thalamoperforating arteries may arise predominantly or exclusively from one side. When a dominant thalamoperforating vessel is seen giving bilateral supply, it is sometimes referred to as the artery of Percheron (Fig. 13-2) (16,17).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree