The mental status examination for a psychiatric evaluation is analogous to the physical examination for a general medical assessment.
The AMPS screening tool (Figure 1.1) includes four primary clinical dimensions of the psychiatric review of systems: Anxiety, Mood, Psychosis, and Substance use. This approach can be easily used in the primary care setting as a starting point to develop a reasonable differential diagnosis for common psychiatric disorders.
The psychiatric interview places an emphasis on psychosocial function and should give a personalized description of the patient from a biopsychosocial perspective.
One helpful time-saving strategy is the use of the Supplemental Psychiatric History Form to help gather a preliminary psychiatric history. A patient should complete this form either before the first clinic visit or during later visits, if a psychiatric illness is suspected.
from the interview is critical to establish a diagnosis, a collaborative, therapeutic relationship is a key component to a successful treatment plan. Therefore, the clinician should try to balance the urgency to obtain information with the need to establish a positive, trusting therapeutic alliance with the patient. Similar in style and complementary to the general medical history, the psychiatric interview is outlined below (Table 1.1).
conceptualize their medical problems. The history of present illness (HPI) should include the duration, severity, and extent of each symptom along with exacerbating and ameliorating factors. Patients vary greatly in their recall of subjective historical material, and often vague or contradictory material surfaces. Once consent is obtained from the patient, it is important to follow up on any inconsistencies with the patient and gather collateral information by speaking with family members and other treatment providers.
Table 1.1 Outline of the Primary Care Psychiatric Interview | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
substance use disorders. We recommend incorporating the AMPS screening tool as part of the HPI. The conversation flows more naturally when the practitioner queries the patient comprehensively about both past and current symptoms. When a particular dimension is present and causing distress, further exploration is indicated (Table 1.2).
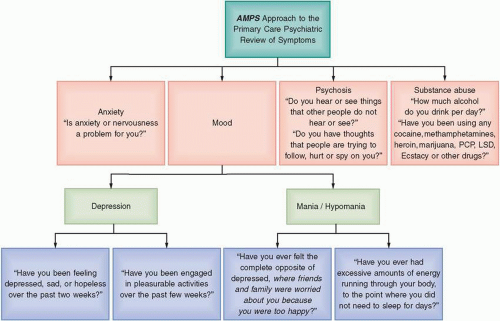 Figure 1.1 Psychiatric review of systems: AMPS screening tool. |
about suicidal thoughts, plans, and intent, with documentation of answers in the medical record.
Table 1.2 The AMPS Screening Tool for Common Psychiatric Conditions | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







