The Relationship Between Neuroanatomy and Neurology: Introduction
Neurology, more than any other specialty, rests on clinicoanatomic correlation. Patients do not arrive at the neurologist’s office saying “the motor cortex in my right hemisphere is damaged,” but they do tell, or show, the neurologist that there is weakness of the face and arm on the left. Since the nervous system is constructed in a modular manner, with different parts of the brain and spinal cord subserving different functions, it is often possible to infer, from a careful physical examination and history together with knowledge of neuroanatomy, which part of the nervous system is affected, even prior to ordering or viewing imaging studies. The neurologic clinician thus attempts, with each patient, to answer two questions: (1) Where is (are) the lesion(s)? and (2) What is (are) the lesion(s)?
Lesions of the nervous system can be anatomic, with dysfunction resulting from structural damage (examples are provided by stroke, trauma, and brain tumors). Lesions can also be physiologic, reflecting physiologic dysfunction in the absence of demonstrable anatomic abnormalities. An example is provided by transient ischemic attacks, in which reversible loss of function of part of the brain occurs without structural damage to neurons or glial cells, as a result of metabolic changes caused by vascular insufficiency.
This chapter gives a brief overview of clinical thinking in neurology and emphasizes the relationship between neuroanatomy and neurology. It has been included to help the reader begin to think as the clinician does and thus to place neuroanatomy, as outlined in the subsequent chapters, in a patient-oriented framework. Together with the Clinical Illustrations and Cases placed throughout this book, this chapter provides a clinical perspective on neuroanatomy.
Symptoms and Signs of Neurologic Diseases
In taking a history and examining the patient, the neurologic clinician elicits both symptoms and signs. Symptoms are subjective experiences resulting from the disorder (ie, “I have a headache”; “The vision in my right eye became blurry a month ago”). Signs are objective abnormalities detected on examination or via laboratory tests (eg, a hyperactive reflex or abnormal eye movements).
The history may provide crucial information about diagnosis. For example, a patient was admitted to the hospital in a coma. His wife told the admitting physician that “my husband has high blood pressure but doesn’t like to take his medicine. This morning he complained of the worst headache in his life. Then he passed out.” On the basis of this history and a brief (but careful) examination, the physician rapidly reached a tentative diagnosis of subarachnoid hemorrhage (bleeding from an aneurysm, ie, a defect in a cerebral artery into the subarachnoid space). He confirmed this diagnostic impression with appropriate (but focused) imaging and laboratory tests and instituted appropriate therapy.
The astute clinical observer may be able to detect signs of neurologic disease by carefully observing the patients’ spontaneous behavior as they walk into the room and tell their story. Even before touching the patient, the clinician may observe the “festinating” (shuffling, small-stepped) gait of Parkinson’s disease, hemiparesis (weakness of one side of the body) resulting from a hemispheric lesion such as a stroke, or a third nerve palsy suggesting an intracranial mass. The way patients tell their story also may be informative; for example, it may reveal aphasia (difficulty with language), confusion, or impaired memory. Details of history taking and the neurologic examination are included in Appendix A.
In synthesizing the information obtained from the history and examination, the clinician usually keeps asking the questions, “Where is the lesion? What is the lesion?” This thinking process will usually result in the correct diagnosis. Several points should be kept in mind while one is going through the diagnostic process.
In the early 1900s, some investigators believed that the nervous system operated via a principle of mass action. According to this now outdated principle of mass action, neurons distributed widely throughout the brain contribute to any given function, and few if any functions depend on localized groups of neurons within a single, demarcated part of the brain. If the brain were, in fact, organized according to the principle of mass action, a lesion affecting any region of the brain would be expected to impair many functions, and few if any functions would be totally lost as a result of a well-circumscribed, localized lesion affecting a single part of the brain.
We now know that, with respect to many functions, the principle of mass action is incorrect. Different parts of the nervous system subserve different functions. In turn, in many parts of the brain or spinal cord, even relatively small well-circumscribed lesions produce loss or severe impairment of a specific function. This effect reflects the principle of localized function within the nervous system.
There are numerous examples of localized function. (1) Aphasia (difficulty producing or understanding language) often results from damage to well-localized speech areas within the left cerebral hemisphere. (2) Control of fine movements of each hand is dependent on signals sent from a hand area within the motor cortex in the contralateral cerebral hemisphere. The motor cortex is organized in the form of a map, or “homunculus,” reflecting control of different parts of the body by different parts of the motor cortex (see Chapter 10, especially Fig 10–14). A lesion affecting the hand area or the highly circumscribed pathways that descend from it to the spinal cord can result in loss of skilled movements or even paralysis of the hand. (3) At a more basic level, many simple and complex reflexes, which are tested as part of the neurologic examination, depend on circuits that run through particular parts of the nervous system. For example, the patellar reflex (knee jerk) depends on afferent and efferent nerve fibers in the femoral nerve and L3 and L4 spinal roots and the L3 and L4 spinal segments, where afferent Ia axons synapse with motor neurons that subserve the reflex. Damage to any of the parts of this circuit (nerve, spinal roots, or L3 or L4 spinal segments) can interfere with the reflex.
As a corollary of the principle of localized function, it is often possible to predict, from neurologic signs and symptoms, which parts of the nervous system are involved. By obtaining an accurate history and performing a careful examination, the clinician can obtain important clues about the localization of dysfunction in the nervous system.
Negative manifestations result from loss of function (eg, hemiparesis, weakness of an eye muscle, impaired sensation, or loss of memory). Negative manifestations of neurologic disease may reflect damage to neurons (eg, in stroke, where there is often loss of neurons located within a particular vascular territory, and in Parkinson’s disease, where there is degeneration of neurons in the substantia nigra) or to glial cells or myelin (eg, in multiple sclerosis, in which there is inflammatory damage to myelin). Positive abnormalities result from inappropriate excitation. These include, for example, seizures (caused by abnormal cortical discharge) and spasticity (from the loss of inhibition of motor neurons).
Damage to gray or white matter (or both) interferes with normal neurologic function. Lesions in gray matter interfere with the function of neuronal cell bodies and synapses, thereby leading to negative or positive abnormalities, as previously described. Lesions in white matter, on the other hand, interfere with axonal conduction and produce disconnection syndromes, which usually cause negative manifestations. Examples of these syndromes include optic neuritis (demyelination of the optic nerve), which interferes with vision; and infarction affecting pyramidal tract axons, which descend from the motor cortex in regions such as the internal capsule, which can cause “pure motor stroke” (Fig 4–1).
Figure 4–1
Magnetic resonance image (MRI) of a 51-year-old patient with hypertension. The patient complained of weakness of the right side of the face and the right arm and leg, which had developed over a 5-h period. There was no sensory loss or problems with language or cognition. The MRI revealed a small infarction in the internal capsule (arrow), which destroyed axons descending from the motor cortex, thus causing a “pure motor stroke” in this patient.
Some neurologic disorders affect primarily gray matter (eg, amyotrophic lateral sclerosis, a degenerative disease leading to the death of motor neurons in the cerebral cortex and gray matter of the spinal cord). Others primarily affect white matter (eg, multiple sclerosis). Still other disorders affect both gray and white matter (eg, large strokes, which lead to necrosis of the cerebral cortex and underlying white matter).
A syndrome is a constellation of signs and symptoms frequently associated with each other and suggests that the signs and symptoms have a common origin. An example is Wallenberg’s syndrome, which is characterized by vertigo, nausea, hoarseness, and dysphagia (difficulty swallowing). Other signs and symptoms include ipsilateral ataxia, ptosis, and meiosis; impairment of all sensory modalities over the ipsilateral face; and loss of pain and temperature sensitivity over the contralateral torso and limbs. This syndrome results from dysfunction of clustered nuclei and tracts in the lateral medulla and is usually due to infarction resulting from occlusion of the posterior inferior cerebellar artery, which irrigates these neighboring structures.
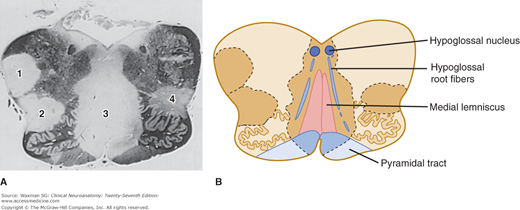
The brain and spinal cord contain many tracts and nuclei that are intimately associated with each other or are anatomic neighbors of each other. Particularly in the brain stem and spinal cord, where there is not much room, there is crowding of nuclei and fiber tracts. Many pathologic processes result in lesions that are larger than any single nucleus or tract. Combinations of signs and symptoms may help to localize the lesion. Figure 4–2 shows a section through the medulla of a patient with multiple sclerosis. The patient had a sensory loss in the legs (impaired touch-pressure sense and position sense) and weakness of the tongue. As an alternative to positing the presence of two separate lesions to account for these two abnormalities, the clinician should pose the question, “Might a single lesion account for both abnormalities?” Knowledge of brain stem neuroanatomy allowed the clinician to localize the lesion in the medial part of the medulla.
Figure 4–2
A: Section through the medulla, stained for myelin, from a patient with multiple sclerosis. Notice the multiple demyelinated plaques (labeled 1–4) that are disseminated throughout the central nervous system (CNS). B: Even a single lesion can interfere with function in multiple neighboring parts of the CNS. Notice that plaque 3 involves the hypoglossal root (producing weakness of the tongue) and the medial lemnisci (causing an impairment of vibratory and touch-pressure sense). Figure 7–7B shows, for comparison, a diagram of the normal medulla at this level.
Dysfunction of the Nervous System Can Be Due to Destruction or Compression of Neural Tissue or Compromise of the Ventricles or Vasculature
Several types of structural pathologic conditions can lead to dysfunction of the nervous system (Table 4–1). Destruction of neurons (or associated glial cells) occurs in disorders such as stroke (in which neurons are injured as a result of ischemia) and Parkinson’s disease (in which degeneration of neurons occurs in one region of the brain stem, the substantia nigra). Destruction of axons secondary to trauma causes much of the dysfunction in spinal cord injury, and destruction of myelin as a result of inflammatory processes leads to the abnormal function in multiple sclerosis.
Mechanism | Disease Example | Target | Comments |
|---|---|---|---|
Destruction | Stroke | Neurons (often cortical) | Acute destruction, within hours of loss of blood flow |
Destruction | Parkinson’s disease | Neurons (subcortical) | Chronic degeneration of neurons in substantia nigra |
Destruction | Spinal cord injury | Ascending and descending axons | Injury to fiber tracts from trauma |