10 The State of the Art in Cerebrovascular Bypasses
Side-to-Side in situ PICA-PICA Bypass
Introduction
Intracranial bypasses are believed to be high-risk operations with poorly studied outcome measures, and they are often considered as the last and final option in the treatment of neurosurgically demanding vascular and oncological lesions. In situ bypasses, such as middle cerebral artery (MCA) to MCA and anterior cerebral artery (ACA) to ACA bypasses, differ from conventional graft-utilizing bypasses in many aspects. For example, in situ bypasses are always occlusive bypasses, contrary to nonocclusive bypasses like ELANA bypasses,1–3 have only one anastomotic site between two intracranial vessels, and do not utilize extracranial or harvested vessel grafts. Poor collateral network limits the use of in situ bypasses to some extent in anterior circulation and in large proximal vessels, whereas distal segments of the posterior inferior cerebellar artery (PICA) are able to tolerate temporary occlusion for indefinite periods permitting the safe creation of bypasses proximal to their vascular territory. Therefore, a side-to-side in situ PICA-PICA bypass operation can be considered a relatively safe and elegant adjunct to the treatment repertoire of, for example, complex vertebral artery (VA)-PICA vascular lesions, when other treatment options could compromise the blood flow through the anterior medullary segment of the PICA vessel.
Only a few dozen side-to-side in situ PICA-PICA bypass cases have been reported to date.4–12 The first report of the side-to-side in situ PICA-PICA bypass was published by Takikawa and others in 1991 describing a 42-year-old man with a ruptured right VA-PICA aneurysm treated with a combination of microsurgical aneurysm trapping and the side-to-side in situ PICA-PICA bypass.12 Due to the lack of technical reports, we will describe this modern bypass technique in the following sections in detail.
Procedure
Preoperative Evaluation
A clear understanding and visualization of the PICA anatomy is of utmost importance. The PICA is a rather complex, tortuous, and variable artery,13 which originates from the intracranial portion of the VA in 80% to 95% of cases (on average 8.6 mm above the foramen magnum and approximately 1 cm proximal to the vertebrobasilar junction).13,14 The gold standard for visualizing the PICAs is a vertebrobasilar angiography for both vertebral arteries; 1.5-T MRA images and CT angiographies can often provide supplementary information for in situ PICA-PICA bypass planning. It is of essence to understand PICA-related anatomical structures, as it will help to clarify the approach for the revascularization procedure.
Decision Process
Although collateral networks in posterior fossa are robust for hemispheric perfusion, sacrifice of the proximal PICA segment can result in catastrophic ischemic injury. This proximal PICA segment maintains the origin of relatively small but extremely critical perforators feeding the medulla oblongata and cerebellum.13 To evaluate the need of the PICA revascularization, the PICA should be divided into five segments and two loops as suggested previously13,15 (Figure 10–1):
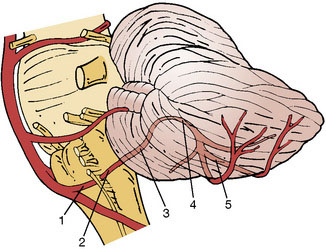
Figure 10–1 The PICA segments illustrated.
(Figure redrawn from Ramina R, et al., Distal posterior inferior cerebellar artery aneurysm: case report. Arq Neuro-psiquiatr 2005;63(2a): 335–338, Fig. 1.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








