Introduction and Overview
Why does addiction exert such a tenacious grip on those who fall under its spell? In this book I propose that the answer to this question lies largely within the cognitive domain: the persistence of addiction is viewed as a failure or aberration of cognitive control motivated by the enduring and unconditional value assigned to substances or behaviours that activate neural reward systems. I shall outline how addictive behaviour endures because it recruits core cognitive processes such as attention, memory and decision making in pursuit of the goal of gratification, the associated alleviation of negative emotions, or both. This recruitment process is often covert, if not subversive, and operates implicitly or automatically in the context of impaired inhibitory control. The habituated drug user is effectively disarmed when exposed to a wide range of cues that generate powerful involuntary responses. The best, and often the only, option is to mount a rear-guard action from the command and control centre of the brain. This sets the scene for a reappraisal of cognitive therapy applied to addiction. Beginning with an overview of the plan and scope of the book, this introductory chapter outlines a cognitive perspective on addiction. It goes on to address shortcomings in historical and current therapeutic approaches to addictive behaviour and includes a brief review of the equivocal and occasionally puzzling findings generated in clinical trials. It concludes with an overview of CHANGE, the re-formulated account of psychological intervention based on cognitive, motivational and behavioural principles in a cognitive neuroscience framework that forms the basis of this text.
Terminology
I have avoided the use of the term addict unless quoting from other sources. I do not think the manifestation of a particular behaviour should be used to denote an individual, in the same way that I would avoid use of terms such as a depressive or an obsessive in other circumstances. Of course, many of those who develop addictive disorders choose to refer to themselves as ‘addicts’. That is entirely appropriate for them, but I believe choosing to designate oneself as an addict is different from being so labelled by another. However, beginning with the title, I readily adopt the term addiction. Here, I apply a functional definition emphasizing the apparent involitional nature of addictive behaviour, its persistence in the face of repeated harm to self and others, and a tendency for drug seeking and taking to recur following cessation. In truth, addictive behaviour and its concomitant cognitive, behavioural and neurobiological facets occur on a continuum of varying, but often escalating, frequency and quantity or dosage. This is why attributing a static label such as addict is likely to miss the point, even if occasionally seeming to hit the nail on the head. There will be some interchange between the terms addiction, substance use and substance misuse according to the context. Generally, however, my use of the term addiction implies that the individual or group referred to meet standard diagnostic criteria for addictive disorders or dependence syndromes. Similarly, and again given pride of place on the front cover, I have opted for the term cognitive therapy rather than cognitive behavioural therapy. This decision is pragmatic rather than doctrinal but does authenticate the emphasis on cognition throughout the book. Both terms feature in the text, and anything deemed purely cognitive can easily be assimilated into the broader church of CBT.
Scope
Addiction has long been a source of fascination for theorists from a wide variety of scientific backgrounds. West (2001) listed a total of 98 theoretical models of addiction, which he classified broadly as either biological, psychological or social in orientation and content. Here, I do not attempt to review this diverse body of work. Nonetheless, West’s taxonomy, referencing a ‘biopsychosocial’ framework, serves as a reminder that addiction is a complex, multifactorial, phenomenon. The main focus here is on understanding the neurocognitive and behavioural mechanisms of addiction and translating this knowledge into more effective therapeutic intervention. Most of the theoretical and empirical findings cited are based on either clinical trials or experimental paradigms involving drug administration, drug ingestion and drug withdrawal in humans and other species. For the most part, the substances at the root of the problems addressed in this text will therefore include opiates, cocaine, amphetamines, alcohol, nicotine and cannabis. At the time of writing, preparations for the fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) are well underway. The term dependence, also central to the ICD-10 (WHO, 1992), is apparently being dropped. This is apparently due mainly to the possibility of conceptual confusion stemming from its dual meaning referring to either uncontrolled drug use, or normal neuroadaptation when, for example, narcotic analgesics are prescribed to alleviate chronic pain (O’Brien, 2011). The forthcoming taxonomy, due to be published in 2013, will therefore refer to ‘Addiction and Related Disorders’. Subcategories will refer to ‘alcohol use disorder’, ‘heroin use disorder’ and so on.
Gambling and other compulsive appetitive behaviours
In the forthcoming diagnostic manual on addictive disorders, the chapter on addiction will also include compulsive gambling, currently classified as an impulse control disorder along with trichotillomania and kleptomania in DSM-IV (American Psychiatric Association, 1994). Consistent with this, Castellani and Rugle (1995) demonstrated that problem gambling is associated with tolerance, withdrawal, urges and cravings, high rates of relapse and high levels of co-morbidity for mental health problems. More fundamentally, from a cognitive neuroscience point of view, it is what goes on in the brain that matters, whether this is triggered by heroin, cocaine, alcohol or indeed gambling. By way of illustration, an intriguing series of case studies provides a more clinical dimension to the motivational power of dopamine, a key neurotransmitter in reward processing, in relation to gambling. Dodd et al. (2005) reported how they encountered 11 patients over a two-year period at a movement disorders clinic with idiopathic Parkinson’s disease who developed pathological gambling. All of these patients were given dopamine agonist therapy such as pramipexole dihydrochloride. Seven of these patients developed pathological or compulsive gambling within 1–3 months of achieving the maintenance dose or with dose escalation. One 68-year-old man, with no history of gambling, acquired $200,000 of gambling debt. On cessation of dopamine agonist therapy his urge to gamble subsided and eventually ceased, an outcome also observed in the seven other patients that were available for follow-up. More generally, other behaviours with a propensity to become compulsive include online activities such as Internet addiction and gaming. My view is that a behaviour such as gambling that activates reward neurocircuitry with wins, and probably downregulates the same system with losses, is liable to become compulsive in susceptible individuals. Consequently, aspects of compulsive gambling and other behaviours where motivation to desist is compromised fall within the scope of this book.
The plan of the book
The book begins with a brief critical appraisal of existing approaches, in particular cognitive and behavioural approaches such as cognitive behavioural therapy (CBT) and cognitive therapy itself (Chapter 2). This review is highly selective insofar as it focuses on shortcomings and unanswered questions, such as the finding that markedly diverse therapeutic approaches, including CBT, deliver broadly equivalent clinical outcomes. In successive chapters (3 and 4), I address first the core learning processes that contribute to the development of addiction and their neurocognitive bases, as well as delineating the predispositional role of exposure to adversity. Next, a conceptual framework that accommodates implicit cognitive and behavioural processes along with more familiar targets such as consciously available beliefs is outlined. The conclusion is that the most plausible way to regulate the former is by augmenting the latter: strategies that enhance executive control, metacognition or awareness are more likely to deliver better outcomes. By emphasizing a component process such as executive or ‘top-down’ control, the therapist and client are provided with a conceptual compass with which to navigate through the voyage of recovery. Chapter 5 addresses the question of individual susceptibility to addiction: if, indeed, drugs and gambling wins are such powerful rewards, why, ultimately, do not all but a small minority develop compulsive or addictive syndromes? This marks the transition from the more theoretical and research based chapters to content that is more directly relevant to the clinical or applied arena, although remaining grounded in a cognitive neuroscience paradigm.
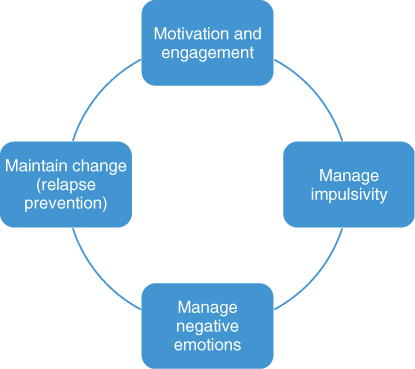
Most of the remainder of the book (Chapters 6, 7, 8 and 9) explicates key therapeutic phases from a cognitive control standpoint. The sequence that unfolds follows the ‘Four M’ structure (see Figure 1.1), which is the enactment of the CHANGE approach:
Chapter 10 aims to summarize, integrate and look forward in the context of a vibrant research arena with major implications for the concept and conduct of cognitive therapy.
Discovering Cognition
Existing accounts of cognitive therapy for addiction have not accommodated findings that cognitive processes, in particular those deemed automatic or implicit, are influential in maintaining addiction, or indeed as a potential means of leveraging change. In cognitive parlance, these models do not legislate for ‘parallel processing’ across controlled or automatic modes, with the latter being largely overlooked. Simply put, existing accounts fail to address what is the hallmark of addiction: compulsive drug seeking behaviour that appears to occur with little insight and often in the face of an explicit desire for restraint. Moreover, existing cognitive therapy approaches do not accommodate findings that cognitive efficiency is often impaired in those presenting with addictive disorders, whether stemming from pre-existing or acquired deficiencies. The client has developed a strong tendency for preferential cognitive processing and facilitated behavioural approach in the face of impaired cognitive control. Failure to acknowledge this leaves the therapist and client in the dark about an important source of variance that is influential at all stages of the therapeutic journey.
The findings of Childress and her colleagues (2008), who used advanced functional magnetic resonance imaging (fMRI) techniques to explore the neural signature of very briefly presented appetitive stimuli, are noteworthy. They found early activation of limbic structures such as the amygdala when the 22 participating abstinent cocaine addicts were shown subliminal, backward masked drug associated cues. A similar pattern was observed when covert sexual stimuli were presented. This design effectively eliminated the possibility of conscious recognition with backward masked exposure for a mere 33 ms, yet participants showed a clear pattern of activation in limbic structures implicated in reward processing. When tested with visible versions of these cues ‘off-magnet’ two days later, initial higher levels of brain activity in response to invisible cues was predictive of positive affective evaluation among the participants. As well as demonstrating the exquisite sensitivity of neural reward mechanisms to drug-related stimuli, these findings show that for habituated drug users the appetite for their drug of choice compares to powerful sexual drives: evidence perhaps that, for some, drugs are as good as, if not better than, sex. Further, Leventhal et al. (2008) found selective subliminal processing of smoking-related cues by nicotine-deprived smokers, again indicating non-conscious evaluative appraisal. It appears that, when exposed to significant cues, the brain makes up its mind very rapidly about what it wants. Extant theories (see, e.g., Marlatt, 1985; Beck, 1993) have difficulty in accounting for these cognitive events and processes, largely because information is processed at one level. Dual processing accounts, which form the basis of this text, have no such difficulty.
Implicit Cognition and Addiction
The definitive feature of implicit cognition is that ‘traces of past experience affect some performance, even though the influential earlier experience is not remembered in the usual sense—that is, it is unavailable to self-report or introspection’ (Greenwald and Banji, 1995, p. 4). These theorists illustrate the operation of implicit cognition with a generic example from experimental psychology. Participants are thus more likely to complete a word fragment or word stem using a word from a list to which they were previously casually exposed. Note that participants may not show explicit recall of the words but the effect of prior exposure nonetheless influences performance. The individual thus appears primed or predisposed to automatically generate a response that appears to evade introspection. This is, of course, precisely what is happening in the brains of the cocaine-addicted people referred to above: the drug-associated cues have acquired considerable emotional and motivational potency that assured them of preferential processing even the absence of conscious awareness.
In the addiction clinic, prior exposure to a vast array of appetitive stimuli, both focal and contextual, is the norm. Learning theory correctly charts the acquisition of conditioned behaviour, but is less able to accommodate cognitive processes, especially if these are implicit rather than manifest. Wiers et al. (2006) sought to clarify the scope of implicit cognition approaches in the addictive behaviour field by proposing three broad categories: attentional bias research, memory bias research and the study of implicit associations. Wiers et al. (2006) concluded that, at least in the populations of problem drinkers addressed in their article, there was an implicit bias towards the detection of alcohol-related stimuli. Following engagement of attention, subsequent information processing was shaped by implicit memory associations. Understandably, given their covert nature, these processes remain largely unseen and unheard by addicted people and their therapists. Moreover, their influence and expression is often masked in the sanitized environment of the treatment centre or clinic, thus creating a somewhat illusory sense of progress. For example, an individual who has just completed a detoxification procedure might explicitly predict their future progress, but implicit factors might improve predictive utility and thus influence the level and intensity of treatment subsequently received. Indeed, preliminary findings from Cox et al. (2002) indicated that alcohol-dependent patients who showed escalating levels of attentional bias to alcohol cues through the treatment episode were more likely to relapse. This raises the question of the feasibility and utility of modifying or reversing cognitive biases that will be addressed in Chapter 7. This finding was replicated by Garland et al. (2012), who found that attentional bias and cue-induced high-frequency heart-rate variability (HFHRV), assessed post treatment, significantly predicted the occurrence and latency to relapse at six-month follow-up in a sample of 53 people in residential care. This was independent of treatment condition (a 10-session mindfulness-based intervention and a comparable therapeutic support group) and after controlling for severity of alcohol dependence.
Implicit cognition might well be subtle but is also pervasive and can be detrimental for both therapeutic engagement and clinical outcomes. Accordingly, cognitive therapy needs to accommodate a broader concept of cognition in addiction, delineating a role for implicit processes in parallel with the more familiar focus on conscious deliberation and re-appraisal. This re-conceptualization is the basis for developing the innovative approaches to formulating and intervening with addictive and impulsive appetitive behaviours that will be addressed in this text. The theoretical framework and clinical strategies are thus derived from CBT but framed within a cognitive neuroscience paradigm. I shall describe how this emergent paradigm can augment existing therapeutics and also generate innovative techniques that directly target the core cognitive and behavioural mechanisms of addiction.
Cognitive control is compromised in addiction
In the context of overcoming addiction, cognitive control is concerned with maintaining recovery goals and monitoring progress in goal pursuit. In particular, managing addictive impulses that have become redundant, unwanted or risky is vital. Cognitive control, especially inhibition, thus forms a key component of the broader executive functioning necessary for self-regulation. Other components of this function, associated with the prefrontal cortex, include shifting strategies in response to changing task requirements and updating by monitoring of goal pursuit. These cognitive operations—shifting, inhibiting and updating—have emerged as relatively independent factors in experimental investigation of executive functioning Miyake et al., (2000). Impaired control over drug use by habituated users is of course a definitive feature of substance dependence and thus a rather obvious target for therapeutic intervention. Cognitive neuroscience findings provide confirmatory evidence for this. Chambers et al. (2009) reviewed evidence pointing to cocaine users, for example, showing impairments on several laboratory measures of impulse control such as having to withhold a well practised response or manifested in making riskier decisions. These deficiencies have been noted both under conditions of acute intoxication and also among abstinent restrained drug and alcohol users. Kaufman et al. (2003), for instance, using fMRI during a go/no go task, found significant cingulate, pre-supplementary motor and insular hyperactivity in a sample of 13 active cocaine users when compared with 14 cocaine naive controls. Forman and colleagues (2004), also using fMRI found abnormally decreased activity of this cingulo-frontoparietal–cerebellar neural network with a cohort of opiateaddicted individuals. These findings suggest that some drugs with addiction liability compromise command and control centres in the brain. This happens during intoxication but also carries over to abstinent periods. The most important faculty required for recovery, cognitive control or willpower, is thus rendered less effective when it is most needed.
Neuropsychological Findings
Conversely, clinical neuropsychological findings indicate that damage to cortical structures can dramatically disrupt appetitive behaviour. Yucel et al. (2007) used a combination of fMRI and proton magnetic resonance spectroscopy to investigate cognitive control in a cohort of 24 opiate-dependent individuals on either methadone or buprenorphine with drug-naive controls. They found that, while anterior cingulate cortex (ACC) activation was equivalent across the two groups, the opiate users failed to demonstrate the normal association between ACC physiological activity and behaviour measures (i.e. response errors) shown by the control group. There were abnormalities detected in neurochemical markers such as N-acetyl aspartate and glutamate. In addition, opiate users required greater involvement of the frontoparietal and cerebellar behavioural regulation network to achieve normal levels of cognitive control. Yucel et al. (2007, p. S99) speculated that ‘The pattern of results across these studies implies that chronic drug use leads to the recruitment of a compensatory network of brain regions in order to successfully detect and resolve conflicts in response tendencies. However, even though normative behavioural performance may be achieved in structured laboratory experiments, the same neural systems may be more vulnerable to fail in the real world, where emotional and motivational influences (e.g. stress, craving, withdrawal, etc.) also tax these cognitive and neural resources’. Interestingly, both the clinic cohort and matched controls showed robust neurocognitive functioning as indicated by obtaining IQ scores of 112, above the normal range. The influence of opiate substitution therapy (average methadone, about 43 mg; average buprenorphine, 10 mg), or indeed premorbid cognitive performance deficits, cannot of course be ruled out as a source of differences between the clinic attendees and the control group. However, in the studies reviewed here, while participants from both experimental and control groups made errors such as pressing a button when they did not intend to, it was those with the addictive history who were somewhat underwhelmed at the neurobiological level, as evidenced by hypoactivity in the cingulate.
With regard to other substances, heavy marijuana use was associated with lower performance on tests of memory, executive functioning and manual dexterity in a sample of 22 regular users who had remained abstinent for 28 days prior to testing (Bolla et al., 2002). Eldreth et al. (2004) compared performance on a modified version of the Stroop task and brain activity between 11 heavy marijuana users who had been abstinent for 25 days and 11 matched comparators. The marijuana users showed no comparative deficits in performance on the Stroop task. However, the marijuana users showed hypoactivity in the ACC and the left lateral prefrontal cortex and hyperactivity in the hippocampus bilaterally, a pattern not observed in the comparator group. This suggests that the marijuana-using group was relying on a compensatory mechanism in the face of suboptimal error monitoring.
Turning to neurocognitive deficits associated with cocaine use, Bolla et al. (2004) used a variant of the Stroop test and positron emission tomography to explore cognitive conflict in 23-day-abstinent cocaine users. While engaged on the Stroop task, cocaine abusers showed less activation than non-drug-using comparison subjects in the left ACC and the right lateral prefrontal cortex but greater activation in the right ACC. This pattern was associated with response competition generated by the Stroop task. Resting scans showed no differences in neural circuitry such as the ACC, which subserves executive functioning. The abstinent cocaine users with the most intense of history of drug use showed the highest level of abnormality when cognitively challenged. Importantly, the two groups performed at equivalent levels on the cognitive tasks, being differentiated only at the neuronal level.
How should these findings be interpreted in the context of responding to addictive behaviour in the clinical arena? First, it is neither possible nor necessarily helpful to speculate on the issue of causality. In this regard, Garavan and Stout (2005) hypothesized that observed functional deficits such as those briefly reviewed above could be the product of pre-existing cognitive ‘trait’ variables such as poor impulse control that could be potentiated by acquired patterns of substance misuse, thus leading to more transient ‘state’ variables such as compromised cognitive control associated with recent intoxication. The fact that these deficits appear to endure for at least a month after cessation of drug use suggests that those involved in delivering therapeutic intervention should, at the very least, be aware of the fact that the client may be compromised in terms of cognitive control or at least have to exert more mental effort in dealing with situations where rapid decision or response inhibition is required.
As evidenced by the robust performance on neuropsychological tests, there did not appear to be global differences in cognitive functioning across the various groups of substance using and control participants. Instead, there appeared to be a specific deficit revealed by precise cognitive tests and neurobiological assays among the cohorts of drug users recruited. From the standpoint of embarking on a journey of rehabilitation that will inevitably involve complex new learning, it appears to me that a deficit in detecting errors or perhaps the necessity to exert more cognitive effort to compensate for this will inevitably prove challenging, if not exhausting. Moreover, these subtle alterations in cognitive processing remain largely unrecognized outside the cognitive neuroscience laboratory. At the very least, awareness of this should enable the addiction therapist to generate more accurate empathy as their clients encounter the inevitable challenges on the route to recovery.
Garavan and Stout (2005) concluded on the basis of their review that drug misusers evidenced a low level of awareness of errors on a range of laboratory tasks. This was associated with hypoactivity in the ACC, a structure vital to performance monitoring . The ACC is the early warning system for errors and is activated during action slips (Garavan et al., 2003), and contributes to the ‘D’oh!’ feeling epitomized by Homer Simpson when he makes yet another error. In a sense, these findings validate phenomenological aspects of drug use. When clients state that they are struggling to cope with the challenges of restraint as they work towards recovery, the informed therapist can thus provide a more empathic response. As will be seen, recognizing deficits in cognitive control is the first step in developing the emerging ‘neurocognitive’ therapy addressed as outlined in Chapter 6 and elsewhere in this volume. This focus on cognition is thus intended to create a therapeutic space that bridges the gap between the neurobiological mechanisms of addiction and the need to devise plausible therapeutic strategies. The rationale is that CBT can be more accurately formulated and precisely targeted by understanding the enduring neurocognitive signature of addiction.
Addictive Behaviour is Primary, Not Compensatory
Second, existing or historical accounts emphasize or assume that addiction is compensatory: compulsive drug use and gambling are seen as a means of dulling or avoiding emotional pain, rather than seeking pleasure or reward. This follows a long tradition in psychology, largely unfettered by empirical support. In the psychodynamic tradition, Kohut (1971, p. 46), for example, viewed drug use as ‘a replacement for a defect in the psychological structure’. The major failing of intuitive accounts of addiction such as this was circular reasoning. They echo historical accounts proposing that ‘moral deficiency’ was the cause of addiction on the decidedly shaky premise that individuals were lacking moral fibre simply because they were addicted. In turn, the addiction was paraded as evidence of the underlying moral frailty.
More recently, cognitive therapy accounts have similarly proposed addiction as a reaction to an event or an emotional state rather than a primary motive. Addiction stemmed from attempts to cope with or suppress maladaptive core beliefs such as ‘I am helpless’ or ‘I am unlovable’ (Beck et al., 1993, p. 52). Cognitive therapists reading this text will doubtless have elicited these beliefs in the course of their work in addiction clinics and elsewhere. Clearly, negative emotions such as depression and anxiety can lead to drug taking, and dysphoria can be also be consequential to intoxication. However, vulnerability to emotional disorders and addictive disorders could also emerge and present in parallel because of their prevalence: lifetime prevalence rates for anxiety disorders in the USA, for example, have been estimated at 29% and mood disorders at 21% of the population (Kessler et al., 2005) and an estimated 120 million of the adult population regularly consume alcohol (Anthony et al., 1994).
It seems plausible that some individuals with coexisting emotional and addictive problems could have acquired these through different mechanisms or learning processes. In this regard, Hiroi and Agatsuma (2005) reviewed evidence indicating genetically distinct pathways leading to expressions of either drug dependence or comorbidity. Presumably, these could coexist. For instance, an individual could acquire an anxious disposition through a combination of genetic predisposition and exposure to adversity in childhood. The same individual could develop a dependence on cocaine or alcohol because of a different combination of genetic predisposition and an environmental factor such as easily available cocaine and hence greater exposure. Significantly, when cigarette smokers speak of their addiction, the listener rarely responds with speculation that this reflects some compensatory behaviour linked to disrupted attachment to parents, or being the victim of cruelty as a child. The addicted smoker is implicitly viewed in a manner more akin to that proposed in this text: regardless of his or her pre-existing vulnerabilities, it seems clear that the problem is inability to give up smoking. Similarly, a lifelong heroin user, recently detoxified, said to me in the course of a brief screening assessment: ‘Basically I’m fine; I’m just an addict’. He did in fact appear to enjoy a sense of well-being. Many of course do not, and this can lead the formulation astray as the therapist and client strive to connect up the addictive behaviour with the negative emotional legacy. Generating a valid conceptualization of addiction is crucial if cognitive and cognitive behavioural approaches are to deliver enhanced outcomes. In the absence of conceptual clarity, confusion can thus emerge. Consider this statement from a client who resumed using cocaine and drinking alcohol after eight months abstinence:
What is it about me, just when I get things right for a change, I start using again and end up relapsing. I seem to push the ‘self-destruct button’. It must be that, deep down, I just want to be a failure (Ryan, 2006, p. 291).
Cognitive therapists (at least this one!) would most likely need to engage their own inhibitory systems to avoid tackling this maladaptive core belief. The CHANGE model does not ignore the possibility that such core beliefs are therapeutically significant, but questions whether they should be the primary focus. Here, a more parsimonious account of addictive behaviour is offered. The attention of the therapist and client when reviewing this episode focused on the more proximal antecedents of behaviour rather than searching for underlying vulnerabilities.
Drugs: no excuse needed!
Here, addiction is viewed as initially appetitive or hedonic, at least in the acquisition phase, when neural reward systems are first transformed by repeated drug ingestion. The hedonism or pleasure may well diminish with habituation but the approach behaviour remains as compelling as ever. It therefore contrasts sharply with common mental health problems such as anxiety and depression manifested (and maintained) by avoidance behaviour, or effortful suppression of unwanted thoughts or images. Existing cognitive therapy accounts of addiction (e.g., Beck et al., 1993) view stress or interpersonal conflict as contexts for eliciting beliefs such as ‘A drink will relax me’, which in turn elicit automatic thoughts such as ‘Drink!’ or ‘Smoke!’. These thoughts evoke craving and urges to use drugs. Without doubt, this is a potential pathway to a lapse or relapse, and a competent therapist would not hesitate in addressing this potentially maladaptive sequence of thought and action. Here, I propose that, while virtually any event or situation can become a precursor to drug use, there is a more direct cognitive–motivational process activated when drug cues are detected. Moreover, negative affect is by no means the only pathway, and positive affect or factors such as testing personal control also appear to precipitate relapse. Granted, these lapses did not prove as sustained as those associated with negative affect (Hodgins et al., 1995). Nonetheless, a different picture emerged when a prospective design was employed to investigate the affective antecedents of relapse among a group of 133 smokers. Shiffman and Waters (2004) found that more enduring, day-to-day changes in stress and negative affect appeared to have little influence on lapse risk, but that more sudden increases in negativity, perhaps triggered by an argument and lasting for shorter periods of hours or minutes, were more likely to promote smoking lapses. They concluded that smokers aiming to give up are best advised to learn to cope with the challenges posed by the transient ‘slings and arrows’ of everyday life. Changes in affect, of whatever valence, are dynamically linked to addictive behaviour but are neither necessary nor sufficient to account for its genesis and enduring legacy. On occasion affective changes serve as triggers for compulsive drug taking or gambling, but often no excuse is needed. Addictive pursuits are intrinsically rewarding.
Changing Habits is the Priority
Therefore, in the current text I am according more immediacy and primacy to drug cues as powerful and direct motivators of behaviour in their own right. There is thus no need for an ‘activating event’ such as stress or interpersonal conflict for drug-seeking behaviour to be mobilized. Situations or scenarios associated with drug use will understandably evoke previously acquired, situation-specific, responses such as reaching for a drink or one’s favourite drug, or immersing oneself in gambling. This is because, in reality, the potential activating event and the drug cue will often share the scene and the timeframe. As implied above, failure to grasp the appetitive essence of addiction has led to problems in how cognitive therapists conceptualize and formulate treatment plans. Cognitive and behavioural therapies have proved very effective in helping anxious and depressed people overcome avoidance. Arguably, instigating behavioural change is the quickest way to change cognitive processes. However, the behavioural signature of addictive disorders is approach. Orchestrating approach or exposure to addictive cues does not reliably or consistently lead to the therapeutic desensitization observed with, say, anxious patients (Conklin and Tiffany, 2002; see p. 159). Further, if cue exposure and response prevention does not work with an anxious person, the result is an unpleasant but usually transient increase in stress on the part of the patient and perhaps a slightly embarrassed therapist. In contrast, for an addicted individual exposed to drug-associated cues in a naturalistic setting, the consequences can be altogether more negative and enduring, as a lapse or relapse can ensue. The relapsing drug user risks losing parenting privileges, freedom, career, relationships, health or even life itself.
Diagnostic Criteria
Diagnostic criteria also appear circular, or at least remaining at a descriptive rather than explanatory level. Thus, the ICD-10 (WHO, 1992) criteria for substance dependence include the following: ‘A cluster of behavioural, cognitive, and physiological phenomena that develop after repeated substance use and that typically include a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences’. Again, the development of dependence, roughly equivalent to addiction in this context, emerges from repetitious substance use. The antecedents or the underlying mechanisms are ignored. This flawed reasoning is also echoed in disease entity or ‘loss of control’ accounts of addiction espoused by Alcoholics Anonymous (AA). Here, the sign or manifestation of the condition—inability to regulate appetitive behaviour—is reframed as the causative factor. Thus, individuals who cannot control their use of drugs or their propensity to gamble are deemed to be afflicted by a syndrome defined by inability to control the behaviour in question.
Towards Integration
Despite the logical shortcomings in the above, individuals can and do respond to well intentioned moral argument, the voice of the cognitive therapist or caring physician or the support of a self-help group. Indeed, there are commonalities between the more traditional views referred to above and the cognitive perspective espoused here: Somewhat ironically, the cognitive neuroscience findings highlighted in the foregoing suggest that self-regulation is indeed impaired in the context of addiction, resonant with the ‘loss of control’ concept that forms the basis of Twelve-Step approaches. There is one crucial difference: cognitive neuroscience illuminates hitherto unrecognized or unknown mechanisms or processes. Neuroimaging and experimental psychology findings, as above, have shown that appetitive stimuli are differentiated from neutral cues outside conscious awareness. It appears therefore that the drivers of addictive behaviour are unreportable by the patient and can thus remain hidden from the clinician. Given the covert nature of the mechanisms of addiction, merely observing addictive behaviour, or seeking introspective reports, has not led to a convincing account of the mechanisms of addictive behaviour. For example, experimental cognitive psychology findings indicate that it is difficult to impede the rapid and preconscious engagement of attention but there is more therapeutic potential in focusing on the enhancement of disengagement of attention, because the latter is more amenable to cognitive control (see Chapter 6). Cognitive neuroscience thus promises to reveal more about the processes that govern addiction than is available through either introspection on the part of the addicted or the observations of the clinician. The aim of this text is to translate these revelations into viable therapeutic formulations and procedures.
Equivocal Findings from Research Trials
Third, cognitive therapy for addiction has not yielded the same robust therapeutic gains typically observed with, for example, anxious and depressed patients: cognitive therapy works, but does not consistently deliver added value when compared with other approaches such as Twelve-Step interventions. CBT has proved wanting, or at best inconsistent, when deployed against addiction, at least when compared with its impressive track record in tackling emotional disorders such as depression and anxiety. Even when our efforts are augmented by CBT, the apparently straightforward task of abiding by our promise not to do something often proves overwhelmingly difficult. Meta-analytic and controlled clinical trial findings attest to the stubborn nature of addiction. Intriguingly, markedly diverse therapeutic approaches including CBT motivational enhancement and Twelve-Step models have been found to deliver equivalent outcomes. As discussed in Chapter 2, this poses a particular challenge to CBT, which prides itself on the integrity and specificity of its core component processes.
Time for CHANGE
To recap, theorists and therapists first need to acknowledge that the cognitive processes that govern addiction are often autonomous. Addictive behaviour can therefore be initiated and proceed in the absence of awareness. The rivalry between these implicit cognitive and behavioural responses and explicit efforts to regulate impulsivity epitomizes the cognitive–motivational conflict that fosters addictive behaviour. Therapeutic intervention in response to addiction is thus more aptly viewed as a form of conflict resolution that directly or indirectly facilitates cognitive control. Interventions that foster cognitive control are more likely to deliver robust and enduring gains. Second, existing cognitive therapy accounts relegate addiction to a compensatory or consequential role symptomatic of underlying personal or emotional vulnerability. Here, I aim to reaffirm the primacy of addiction, regardless of the emotional or personal context from which it stems. Third, clinical outcomes observed after cognitive and behavioural interventions are often equivocal and sometimes negligible. Moreover, there is no empirically based consensus on the key mechanisms of change, as diverse therapies generate equivalent results. The CHANGE framework aims to address the above issues by acknowledging a role for implicit or automatic cognitive processes and emphasizing the primacy of addictive behaviour as a target for therapeutic intervention. However, emotional and neurocognitive factors are intrinsically linked to the initiation, maintenance and cessation of addictive behaviour. Accordingly, affect regulation and cognitive control skills are assigned a key role in enabling individuals to overcome addiction.
Evolution, Not Revolution
The aim of this book is not, however, to advocate abandoning tried and tested methods of therapeutic intervention with addictive behaviour and supplanting these with novel strategies, not least because for the most part the latter await the verdict of clinical trials. Rather, by delineating a core component process—cognitive or executive control—the aim is to accentuate common features in the mechanisms of change. As will be seen, viewing established therapeutic approaches such as cognitive therapy, motivational interviewing and Twelve-Step programmes through a cognitive processing prism reveals perhaps surprising commonality in the midst of diversity. Novel techniques that have only recently emerged from the experimenters’ laboratories, such as cognitive bias modification or strategies for inhibiting automatic approach tendencies, will also be assigned a role in the evolving neurocognitive framework that forms the basis of this book. In this regard, the book resonates with contemporary efforts to anchor cognitive therapy in a more neurobiological framework. Disner et al. (2011), for example, described a neurobiological architecture based on Beck’s (1967) cognitive model of depression. They proposed that the negative cognitive biases that characterize depression are facilitated by greater activity in subcortical emotion processing regions such as the thalamus and amygdala in tandem with attenuated top–down cognitive control mediated by areas such as the prefrontal cortex. The relevant point here is that extant models of cognitive therapy are fundamentally about how information is processed, especially that which is emotionally or motivationally significant.
In addition to exploiting emergent trends in applied cognitive science, I also intend to delineate a role for the ancient tradition of mindfulness. The conceptual thread running through such apparently diverse approaches is cognitive control: Remedial strategies capable of fostering disengagement, detachment or indeed greater awareness or insight offer the potential to derail the self-perpetuating spirals of desire and impulsivity that characterize addiction. However, merely identifying a component process such as cognitive control, or suggesting an addicted person simply adopts mindful awareness, is not necessarily therapeutic! The strength of the cognitive therapy approach is based on the twin pillars of conceptualization and formulation, both firmly embedded in a therapeutic alliance. The book is thus in keeping with the pragmatic empiricism that defines cognitive and behavioural therapies insofar as it eagerly embraces any technique or strategy that demonstrably enhances self-regulation, reduces distress and ultimately improves well-being.
Something Old, Something New
The reader will encounter much that is familiar and based on the inspirational work of other clinicians and researchers as well as much as yet unseen. From a clinical standpoint, a definitive feature of this book is the sequential manner in which therapeutic intervention is conceptualized, formulated and orchestrated. Motivational enhancement strategies thus precede interventions aimed at enhancing impulse control that in turn anticipate efforts at improving emotion regulation. Importantly, motivational enhancement strategies are seen as an integral part of the therapeutic intervention rather than just a preparatory phase. Motivation thus remains crucial, at all stages of the therapeutic process. This is because addiction represents a distortion of motivation that is at least partially maintained by implicit cognitive processes. This relentless processing remains dedicated to following the pre-treatment agenda of drug seeking and drug taking long after the individuals seeking treatment have explicitly declared their intention to change. The most important message is that greater understanding of the cognitive–motivational aspects of addiction will serve as a platform for a robust therapeutic alliance and the delivery of therapy that has a valid focus on appropriate intensity.
More detailed exploration of the therapeutic engagement, motivation and formulation marks the transition to the second part of the text, beginning with Chapter 5. Thus begins an elaboration of this model CHANGE (Change Habits and Negative Generation of Emotion). As outlined above, CHANGE is differentiated from existing approaches in four key areas.
- Addiction is viewed as a failure of cognitive control.
- CHANGE addresses both controlled and automatic cognitive processes as part of a formulated intervention.
- It recognizes the imperative of directly targeting addiction, notably with its emphasis on cognitive control and the promotion of therapeutic strategies to promote this.
- It explicates how to recognize and manage the psychological mechanisms in addiction, such as lack of insight, that can undermine the therapeutic alliance and sap the resolve of both patient and therapist.
CHANGE also aims to provide a route map for therapeutic intervention that should guide both therapist and client through a predictable sequence of stages referred to as the Four Ms. By acknowledging evidence of subtle but pervasive cognitive deficits in areas such as inhibition and error monitoring (see Chapter 3), the therapist is provided with clear justification for devoting time in session and assigning tasks between sessions that focus on problem-solving strategies and skills.
Overall, I aim to respect key tenets of cognitive and behavioural approaches. Fundamentally, CHANGE is thus collaborative, active, time limited and structured. It utilizes, for example, the complementarity between ‘within session’ change processes and ‘between session’ change processes. It thus finds common ground with recent accounts of cognitive therapy such as that by Bennett-Levy et al. (2004, p. 6), who defined the overall strategy of cognitive therapy as twofold:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree