Chapter 11 The theoretical basis for evidence-based neurological physiotherapy
Introduction
This chapter aims to explain the theoretical framework underlying current practice in neurological physiotherapy for adults with damage to the nervous system. The text below will explain why theory and evidence-based practice are important, clarify the role of the neurological physiotherapist and discuss the key neurophysiological, motor learning and behavioural principles that guide practice. These guiding principles are derived from the theoretical framework proposed by Lennon and Bassile (2009).
Why are theory and evidence-based practice important?
Therapists need to subscribe to a theoretical framework for intervention, as theory provides the explanation not only for the behaviour of people following neurological damage, but also for the actions and decisions of therapists in clinical practice (Shephard, 1991). There are several neurological treatment approaches that influence the content, structure and aims of therapy. In the past therapists may have implemented care based on their preferred treatment approaches. However, to date there is no evidence to suggest that one therapy approach is superior to another (Kollen et al., 2009; Pollock et al., 2007). Therapy delivered in practice is always composed of multiple components tailored to suit each individual patient; therefore, research trials should aim to evaluate the active ingredients or components within physiotherapy, as similarities between approaches may actually outweigh their differences. In order to implement evidence-based practice, therapists are expected to incorporate a wide range of strategies that are supported by the current evidence base into their treatment programmes (Pollock et al., 2007).
There are many examples of specific training strategies such as strength training or task-specific practice, which are effective at improving movement and function (Van Peppen et al., 2007 see www.cochrane.org for relevant systematic reviews). There are also many clinical guidelines that provide a comprehensive review of all the available evidence to date for multidisciplinary management of people post-stroke (NCGS, 2008), with Parkinson’s disease (Keus et al., 2006) and with multiple sclerosis (MS Society, 2008). These guidelines, developed by multidisciplinary panels and subjected to peer review, and are based on the best available evidence.
Components selected within therapy sessions should be evidence-based rather than based on therapist preference for a specific treatment approach. However, it is also important to realize that there are still many key areas of clinical practice with no evidence or conflicting evidence; therefore, therapists continue to rely on their clinical reasoning skills to select treatment techniques appropriate to the needs, wishes and goals of patients and their carers. This is why evidence-based practice is defined as the integration of best evidence with clinical expertise and patient values (Bernhardt & Legg, 2009).
Evidence-based guidelines rather than therapist preference for any named therapy approach should serve as a framework from which therapists should derive the most effective treatment (Kollen et al., 2009). However, there are many methodological shortcomings in the current evidence base and further high-quality trials need to be conducted (Kollen et al., 2009).
Role of the physiotherapist
Physiotherapists help patients, their carers and the multidisciplinary team to identify potential for change following damage to the nervous system. Physiotherapists provide stimulus via movement to engage patient response; physiotherapists make movement and activity possible by using a variety of strategies such as therapeutic handling, or elimination of gravity and activity in mid range to elicit motor activity even when patients are unable to demonstrate movement to command (Kilbride & Cassidy, 2009).
The aims of neurological physiotherapy can be summed up using the acronym RAMP for Recovery, Adaptation, Maintenance and Prevention (see Figure 11.1).

Figure 11.1 RAMP – aims of neurological physiotherapy.
(Reproduced from Lennon S, Bassile C. Guiding Principles for neurological physiotherapy. In Lennon S, Stokes M (eds). Pocketbook of Neurological Physiotherapy. Elsevier Ltd, London, 2009, pp. 97-111, with permission from Elsevier Ltd.)
Physiotherapy ideally aims to restore movement and function in people with neurological pathology, but this may not always be possible. Adaptation (compensation) refers to the use of alternative movement strategies to complete a task (Shumway-Cook & Woollacott, 2007, pp. 152–153). Therapists focus on promoting compensatory strategies that are necessary for function and discouraging those that may be detrimental to the patient, e.g. promoting musculoskeletal damage, such as knee hyperextension (Edwards, 2002, p. 2). Interventions aimed at recovery of function need to be emphasized over compensation if the patient has the potential to change. Maintenance of function is just as important as recovery, and should be viewed as a positive achievement; several reviews have now confirmed that functional ability can be maintained despite deteriorating impairments in progressive neurological disease (Keus et al., 2006). Physiotherapy also aims to prevent the development of complications such as contracture, swelling and disuse atrophy. There are different stages in patient management, where these aims may have differential priorities. Understanding the nature of the pathology, and the prognosis for recovery in collaboration with patients and care givers to establish desired goals will help determine which of these aims should be emphasized in physiotherapy.
Guiding principles
Lennon and Bassile (2009) have identified eight principles to guide physiotherapy practice (see Figure 11.2): (1) the World Health Organization (WHO) International Classification of Functioning, Disability and Health (ICF); (2) team work; (3) patient-centred care; (4) neural plasticity; (5) a systems model of motor control; (6) functional movement re-education; (7) skill acquisition; and (8) self-management (self-efficacy). Each of these principles will be discussed in this chapter.
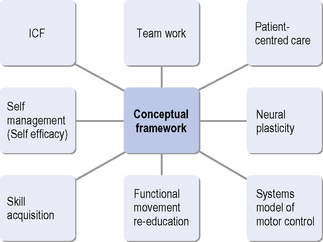
Figure 11.2 Guiding principles for neurological physiotherapy.
(Reproduced from Lennon S, Bassile C. Guiding Principles for neurological physiotherapy. In: Lennon S, Stokes M, eds. Pocketbook of Neurological Physiotherapy. Elsevier Ltd, London, 2009, pp. 97-111, with permission from Elsevier Ltd.)
Principle 1: The ICF
The WHO has developed the ICF (2001; www.who.int/classifications/icf), which provides a systematic way of understanding the problems faced by patients, illustrating the multiple levels at which therapy may act. The activities dimension covers the range of activities performed by an individual. The participation dimension classifies the areas of life in which there are societal opportunities or barriers for each individual.
Within the ICF framework, neurological physiotherapy may directly target both impairment (a loss or abnormality of body structure) and activity (performance in functional activities) with the overall aim of improving quality of life and enabling participation in desired life roles. Most large randomized controlled trials agree that patients need to have a minimum level of residual movement to demonstrate functional improvement (Van Peppen et al., 2004). This means that therapists will need to use both impairment and function focused strategies depending on the patient.
Principle 2: Team work
Neurological physiotherapists use their clinical reasoning skills combined with current evidence to assess, develop and evaluate an appropriate plan of care in collaboration with the patients and their carers, and the multidisciplinary team (Ryerson, 2009).
Team work is required to coordinate rehabilitation, as a variety of health-care professionals are involved to exchange information with the patients and their families. Team meetings are held to agree a common plan of care in order to reduce the risk of conflicting information, and to work towards common goals (Sivaraman Nair & Wade, 2003). Interdisciplinary rehabilitation refers to the activities of the health-care team, where there is a high level of communication, mutual goal planning and evaluation (Long et al., 2003). The Stroke Unit Trialists Collaboration (SUTC, 2006) has identified that patients who receive organized stroke unit care provided in hospital by nurses, doctors and therapists who specialize in looking after stroke patients and work as a coordinated team are more likely to survive their stroke, return home and become independent in looking after themselves. Thus it would appear that team working is an essential factor in improving patient outcomes.
Goal setting
Developing an appropriate plan of care revolves around collaborative goal setting within the team. Setting goals by the interdisciplinary team is recognized as a core component of neurorehabilitation (Wade, 2009). Setting goals aims to:
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







