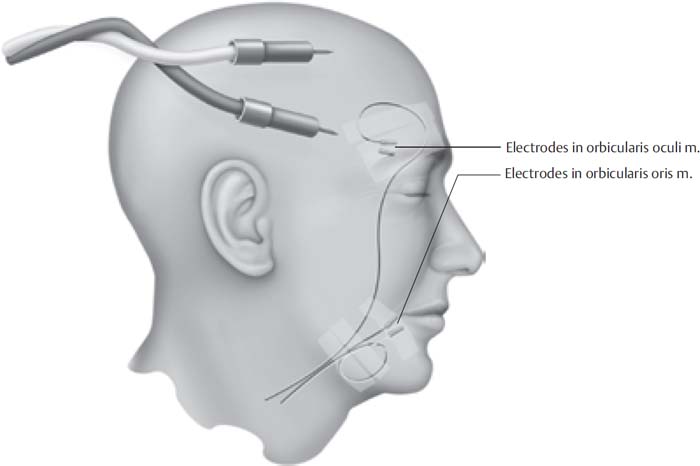
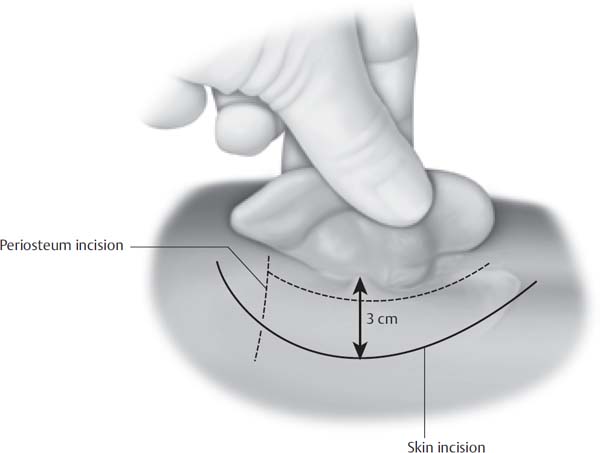
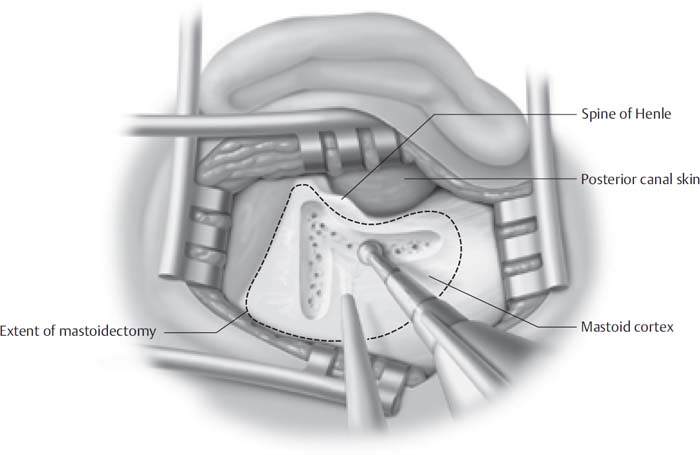
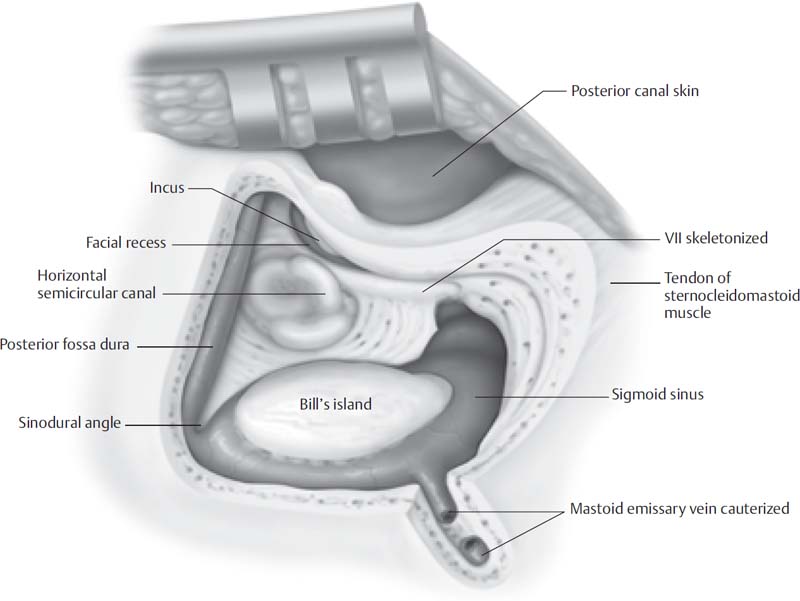
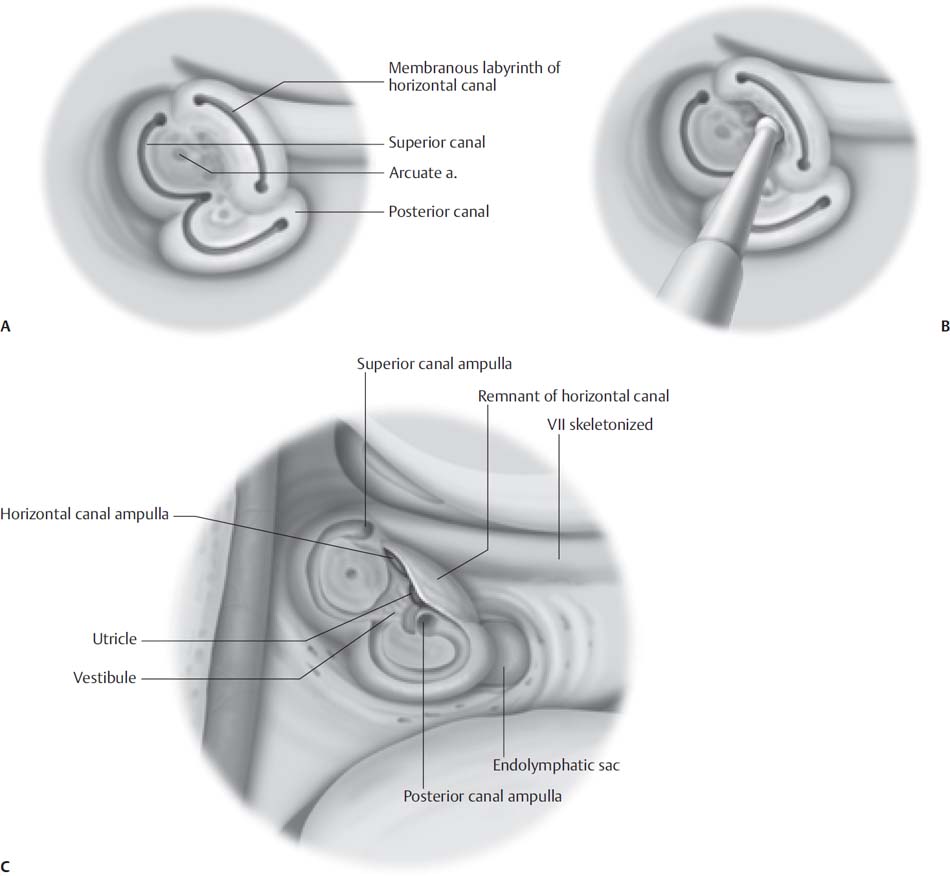
6 The translabyrinthine approach is the most direct approach to the cerebellopontine angle. It was first used by William F. House in the 1960s to remove acoustic tumors, and it resulted in a significant drop in the mortality associated with acoustic tumor removal. The House Clinic has been using this approach since that time. More than 5,000 acoustic tumor (vestibular schwannoma) surgeries using the translabyrinthine approach have been performed at House Clinic. The approach provides excellent exposure to the cerebellopontine angle, allowing early identification of the facial nerve in the labyrinthine segment. The entire facial nerve can be exposed from the brainstem to the stylomastoid foramen. One advantage of this approach is that the entire tumor can be visualized extradurally, reducing the requirement for any type of retraction on the brain. The main disadvantage of the translabyrinthine approach is the sacrifice of hearing. This approach is most commonly used for vestibular schwannoma removal, although it may also be used for total cranial nerve VIII section for disabling vertigo when no useful hearing remains, and for facial nerve tumor removal or facial nerve repair following temporal bone fractures. The translabyrinthine approach is ideal for vestibular schwannoma removal, regardless of the size of the tumor, when the hearing is poor. It is also useful in tumors larger than 2.0 cm when chances of hearing preservation are extremely poor. The approach has many advantages including minimal cerebellar retraction. The lateral end of the internal auditory canal (IAC) can be dissected to ensure complete tumor removal from this area, and this approach allows consistent visualization of the facial nerve in the labyrinthine section. Another advantage of the translabyrinthine approach is that the patient is in the supine position with the head turned away from the surgeon, reducing the risk associated with the sitting position of the classic suboccipital approach where the risk of air embolism was significant. The translabyrinthine approach poses no danger of air embolus and does not require retraction of the cerebellum. Most of the surgical approach is extradural, which lessens any trauma to the brain. The tumor can be directly approached and dissection begun without any retraction on the brain. This extradural dissection also decreases the risk of spreading bone dust into the cerebellopontine angle, which may contribute to the headaches associated with the sub-occipital procedure. This approach may be used for tumors other than vestibular schwannomas including meningiomas, cholesteatomas that involve the petrous bone or posterior fossa, cholesterol granulomas in which the hearing has been lost, and glomus tumors. If the facial nerve is lost during tumor removal, a direct nerve anastomosis may be performed. This technique may also be used when a facial nerve schwannoma requires removal. The facial nerve may be removed from the fallopian canal in the vertical and horizontal segments. Mobilization of the facial nerve allows the temporal portion of the facial nerve to be swung down into the cerebellopontine angle for a direct nerve anastomosis. Neuragen tubules can facilitate nerve anastomosis in the cerebellopontine angle, as suturing is difficult due to the lack of epineurium surrounding the facial nerve stump at the brainstem. This offers the best opportunity for facial reanimation with an immediate direct end-to-end nerve anastomosis or, on the rare occasion, an interpositional nerve graft. The disadvantage of the translabyrinthine approach is sacrifice of any residual hearing. Therefore, the procedure is reserved for patients with poor hearing, or patients whose tumor is larger than 2.0 cm in size, in which case hearing preservation is extremely rare. • Large acoustic neuromas • Acoustic neuromas with poor hearing • Massive cholesteatomas • Cerebellopontine angle tumors with poor hearing • Auditory brainstem implant placement • Growing acoustic neuromas, status post–radiation treatment The choice of approach toward a tumor in the cerebellopontine angle is based on tumor type, size, location, and baseline hearing status (Table 6.1). Vestibular schwannomas that are large with no serviceable hearing are ideal for this approach. Small tumors that extend no more than 1.0 cm into the cerebellopontine angle with good residual hearing may be removed via a middle fossa approach described in Chapter 3. Vestibular schwannomas that are medial in location with very little projection into the IAC and good residual hearing are usually approached via a retrosigmoid/suboccipital approach. The decision to attempt hearing preservation depends on the status of the preoperative hearing and location of the tumor. Serviceable hearing is defined by the 50/50 rule: this definition requires that the pure-tone average be better than 50 dB and the speech discrimination score be greater than 50%. The status of the contralateral ear must also be taken into consideration when deciding the approach as, rarely, these tumors may present in an only-hearing ear or a better-hearing ear. Vestibular schwannomas larger than 2 cm are usually removed with the translabyrinthine approach, as the chance of preserving the hearing is poor in tumors this large. The choice of approach for meningiomas may be different from that used with vestibular schwannomas, even when located in the same position. Meningiomas have a tendency to displace rather than invade the cochlear and facial nerves, and therefore they have a better chance of hearing preservation, even with large tumors. Therefore, a hearing preservation approach may be selected even if the hearing is poor. Hearing improvement can occur with meningioma resection. No tumor is too large to be removed via the translabyrinthine approach. Larger tumors require an expanded exposure with more bone removal over the middle fossa and posterior fossa dura. The House Clinic has removed all large acoustic tumors via the translabyrinthine approach for the past 50 years. General endotracheal anesthesia with inhalation agents is used. Muscle relaxants are used only for induction, as they may interfere with nerve monitoring, specifically intraoperative facial nerve monitoring. An oral gastric tube and Foley catheter are placed. Antibiotics with good cerebral spinal fluid penetration are given prior to skin incision. Cefuroxime is our antibiotic of choice in non–penicillin-allergic patients, whereas vancomycin is used in those patients with penicillin allergy. Intravenous antibiotics are given for 24 hours and perioperative steroids are used. The patient is instructed to use Hibiclens solution (Mölnlycke Health Care, Norcross, GA) daily for the 3 days preoperatively to reduce skin bacteria. The average blood loss with translabyrinthine procedures is less than 250 cc. The need for blood transfusion is extremely rare, but all patients have a type and screen performed preoperatively. One to two units of blood are reserved for patients with large tumors, as the risk for transfusion increases with very large tumors greater than 2.5 cm. Patients are offered the opportunity to directly donate 1 to 2 units of their own blood preoperatively to be available for use during surgery. This has to be done at least 3 to 4 weeks in advance of the surgery. Iron supplements are recommended for these 3 to 4 weeks to increase the hematocrit after donation. The patient is placed in the supine position with the head turned away from the surgeon. The table is rotated 180 degrees so that the foot of the table is next to the anesthesiologist. This allows the anesthesiologist to control the table for movement. The surgeon is seated at the table with the scrub nurse across from the surgeon. The microscope is placed at the head of the table. The head is placed on a donut or a gel pad to prevent pressure necrosis on the contralateral scalp. No fixation of the head is required. Hair is shaved from the postauricular and temporal areas. The skin is cleaned with a povidone-iodine (Betadine) solution and a sheet of Ioban is placed over the entire area. Facial nerve monitoring is considered the standard of care for all vestibular schwannoma procedures and all translabyrinthine procedures. The Medtronic (Jacksonville, FL) facial nerve electromyogram (EMG) monitor is recommended, as it has been specifically designed for this use. Needle electrodes are placed in the orbicularis oris and orbicularis oculi muscle (Fig. 6.1). A facial nerve EMG is recorded, and this EMG is then used to monitor the facial nerve throughout the case. The lower abdomen is also prepped and draped with Ioban to allow for harvesting of fat graft. The fat graft will be placed in the temporal bone defect after the tumor is removed. The navel is prepped in the abdominal field for orientation. The fat graft is obtained from the left lower quadrant to prevent later mistaking the incision for an appendectomy scar. One percent lidocaine with 1/100,000 epinephrine is injected into the postauricular area. The epinephrine assists with hemostasis. A postauricular incision is made approximately 3.0 cm behind the auricular sulcus (Fig. 6.2). As a general rule a larger tumor requires a more posterior incision. This allows for additional decompression of the dura posterior to the sigmoid sinus. A two-layer incision is created, with the first part of the incision in the skin and the second incision involving the temporalis muscle and periosteum. Ideally, these two incisions should be offset, which helps prevent cerebrospinal fluid (CSF) leakage. The first incision involves the scalp flap just superficial to the temporalis fascia and mastoid periosteum, allowing elevation and anterior movement of the pinna. The second incision is through the periosteum and temporalis muscle, and is T-shaped with the horizontal incision approximately 1.0 cm above the linear temporalis and the vertical incision just posterior to the external ear canal. The Lempert elevator is used to elevate the periosteum off the bone of the mastoid. Care must be taken not to tear the skin of the external auditory canal, otherwise a CSF leak may develop posteriorly. The periosteal flap is brought posteriorly, and a large self-retaining retractor is used to retract the tissue, thus exposing the mastoid cortex for extensive bony dissection. Electrocautery may be required to remove the periosteum off the mastoid tip at the insertion of the sternocleidomastoid muscle. Care is taken in elevating the periosteal flaps as the same tissue is needed for closure to aid in prevention of cerebral spinal fluid leaks. Fig. 6.1 Facial nerve monitoring of face. Fig. 6.2 Skin incision. A complete cortical mastoidectomy is performed (Fig. 6.3). There are two schools of thought on the translabyrinthine approach regarding a mastoidectomy. Some surgeons prefer to leave bone over important structures such as the dura and sigmoid sinus, only to remove this bone after further medial dissection has been performed. This technique can be very useful during training procedures with residents or fellows, because important structures are protected during the drilling. The disadvantage of this approach is that it limits the angle of exposure because the dura cannot be compressed due to the thin shelf of bone left over the dura and sigmoid sinus. My preference is to remove all bone as dissection continues medially, creating a large angle of exposure. A cortical mastoidectomy is performed with a standard T-incision. The first bony cut is along the linear temporalis, with a second cut directly behind the external ear canal. All cortical bone is removed from the mastoid. The middle fossa dural plate and sigmoid sinus are identified. All air cells are removed from behind the external ear canal to identify the external ear canal. Bone is removed down to the mastoid tip for exposure; however, cortical bone is left on the mastoid tip to allow screws to be placed for titanium mesh cranioplasty plating. In contrast to chronic ear disease, it is usually not necessary to remove bone up toward the zygomatic arch. In chronic ear disease the epitympanic space must be opened widely. In contrast, the surgeon rarely needs to remove this bone in a translabyrinthine approach. Fig. 6.3 Cortical mastoidectomy. Fig. 6.4 Complete mastoidectomy. It is important that the surgeon performing the translabyrinthine approach be familiar with dissection in the posterior fossa. A criticism of the translabyrinthine approach is that it does not allow adequate exposure and it is difficult for the neurosurgeon to work in such a tight space. This is true only if the translabyrinthine approach is not done correctly. The angle of exposure is important, especially as the surgeon works medially, because the wider the exposure laterally, the more working area that is available for the dissection in the cerebellopontine angle. A very narrow translabyrinthine approach will significantly limit and make dissection much more difficult in the cerebellopontine angle. Bone is removed off of the middle fossa plate from the sinal dural angle forward to the posterior limit of the external bony ear canal. All air cells are removed from the bony external ear canal so that a thin shelf of bone is all that remains. The sigmoid sinus is identified, and a thin layer of bone (“Bill’s island”) is left on top of the sigmoid sinus. Bill’s island was extremely important when older drills were used as they had a tendency to cut and tear open the sigmoid sinus (Fig. 6.4). New high-speed air-driven drills rarely cause this problem, but nonetheless, this acts as a protective factor. Care must be taken in compressing the bone over the sigmoid sinus or compressing the sigmoid sinuses as blood clots can arise. This becomes especially important in patients with bilateral acoustic tumors. Although rarely causing problems, increased cranial pressure can arise postoperatively from an occluded sigmoid sinus. The mastoid emissary vein has a very consistent anatomic relationship located posteriorly to the midportion of the sigmoid sinus. Bone is removed posteriorly to the sigmoid sinus over the posterior fossa dura for large tumors and in anatomic cases where the sigmoid sinus is found in a more anterior location. Bone may be removed up to 2.0 cm behind the sigmoid sinus. The mastoid emissary vein is removed from the bone and coagulated. Ideally, a diamond drill can be used to drill on each side of the mastoid emissary vein until a small tag is left that is coagulated with a bipolar cautery. It is best to leave a small piece of the mastoid emissary vein next to the sigmoid sinus, which makes cauterization easier. Upon completion of the cortical mastoidectomy, the middle fossa plate, the sigmoid sinus, and the posterior ear canal have been identified. Bone is removed down to the antrum so that the incus and horizontal semicircular canal may be identified. The horizontal semicircular canal is a landmark, which helps with identification of the facial nerve and labyrinth. The vertical segment of the facial nerve may be identified and skeletonized. Bone should be left over the facial nerve. The retrofacial air cells may be opened, but care must be taken to prevent the drill bit from undercutting into the facial nerve. Air cells are removed down to the digastric ridge, and air cells should also be removed from the mastoid tip. Fat packing is easier when all the air cells have been removed, but this also helps prevent CSF leak. The bone over the sinodural angle should be removed with care, as the superior petrosal sinus lies underneath this area. Occasionally small fragments of bone will embed into the sinus, and removal can cause bleeding. Bipolar cautery will usually control this. If significant bleeding occurs, packing the sinus with Surgicel should control the bleeding. Bone wax is placed over the Surgicel, which prevents the Surgicel from getting caught up in the drill during further dissection. The hard bone of the labyrinth may be drilled with a cutting or diamond drill bit, depending on the comfort of the surgeon (Fig. 6.5A). More experienced surgeons may use a cutting drill bit, whereas those with less experience are encouraged to use a diamond drill bit. The risk of complications such as facial nerve injury or damage to the dura increases as drilling continues medially. The horizontal semicircular canal should be identified as a result of the mastoidectomy. Safe drilling may be performed superior to the horizontal semicircular canal and posterior to the posterior semicircular canal (Fig. 6.5B). This general guideline prevents injury to the facial nerve. Drilling is continued to outline the circular nature of the semicircular canals. The circular nature of the semicircular canal should be retained until all semicircular canals are outlined to help prevent disorientation by the surgeon. Snake eyes is defined as a cut across the semicircular canals when both ends of the canal are facing lateral and the circular orientation has been lost, and this is to be avoided. The horizontal semicircular canal bisects the posterior semicircular canal creating a T-formation. The superior semicircular canal is entirely superior to the horizontal canal, and the common crus is identified as the junction of the posterior and superior semicircular canals. If the incus has been removed, the suction irrigator is positioned over the facial nerve to protect the facial nerve during drilling. Cases have been reported in which the drill rolled over the top of the horizontal semicircular canal, injuring the facial nerve. The first goal of the labyrinthectomy is to have all three semicircular canals completely outlined so that the anatomic relationships remain intact. The superior semicircular canal is opened to the ampulla and vestibule. The junction of the ampulla and vestibule is a landmark that identifies the superior aspect of the IAC. The ampulla of the posterior canal is a landmark for the inferior border of the IAC. The posterior semicircular canal is also opened into the vestibule. The inferior bony removal is to the level of the jugular bulb. Bone is removed medial to the jugular bulb and in many cases anterior to the jugular bulb. In cases of a high jugular bulb, bipolar cautery may be used on the dura overlying the jugular bulb to allow the jugular bulb to shrink. Fig. 6.5 Labyrinthectomy. (A) The orientation of the labyrinth; (B) drilling performed superior to the horizontal semicircular canal; (C) labyrinthectomy completed with the vestibular open.
The Translabyrinthine Approach to the Skull Base
 Indications and Patient Selection
Indications and Patient Selection
 Surgical Technique
Surgical Technique
Positioning
Skin Incision
Mastoidectomy
Labyrinthectomy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Translabyrinthine Approach to the Skull Base
