The Use of Outcome Scales in the Management of Spondylolysis
Finn Bjarke Christensen
Thomas Andersen
Why should outcome measurement of spinal patients’ health and treatment be less accurate than corresponding measurements in other fields such as evaluation of educational achievements? There truly is no reasonable justification for this discrepancy; individual outcome assessment of patients receiving spinal treatment is essential in today’s health care environment. In the construction of a spinal health index, a fundamental issue is how to select among the virtually unlimited number of questions that could potentially be included. The vast numbers of assessment techniques reported in the literature complicates the choice of appropriate tools for the assessment of clinical results. Thus, it is difficult to recommend the “best questionnaire buy” without knowledge of the study in which the user intends to use the method. The user must decide exactly what is required of the measurement. For example, will it be used to evaluate a program of care, or to study individual patients? What type of patient will be assessed (what diagnosis, age group, level of disability)? What time frame must the assessment cover: acute or long-term conditions?
Patient-oriented outcome measurements should include categories pertaining to health-related quality of life (symptoms and pain, activities of daily living, social, psychological, role status/employment), satisfaction, and costs.
Clearly, no single variable adequately describes health; rather, its measurement relies on compilation of a number of variables as indicators of outcome or health, each of which represents an element of the overall concept. Although there is a broad range of available tools, only a limited number of measurement instruments are frequently used.
The impact of low back pain can generally be described and measured on three different levels:
Physical impairment (decreased range of motion, reduced muscle strength, neurologic deficiency, etc.)
Physical disability (reduced walking ability; impaired lifting capacity; decreased ability to sit, stand, and perform other physical functions)
Social handicap (the resulting limitations in social, vocational, and recreational life as well as life satisfaction).
In the selection of outcome questionnaires, the following aspects should be considered:
Is the questionnaire validated? (Does it measure what it claims to measure?)
Is it reliable? (Is it consistent and reproducible?)
Is it responsive? (Is it capable of detecting subtle change?)
Is the questionnaire available in the target language?
Is the questionnaire sensible? (Is it relevant, and easy to complete and score?)
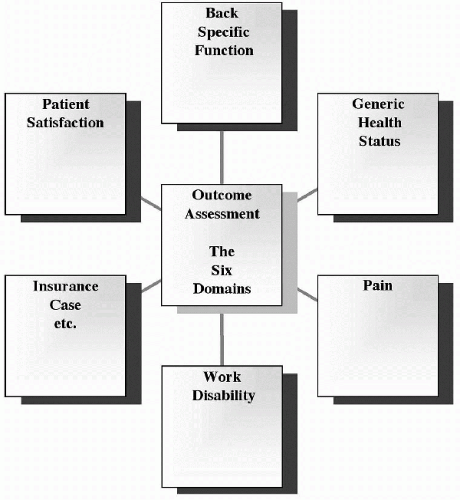
For outcome assessment, we recommend the six domains shown in Figure 32.1. However, if there is a risk of burdening the patient, which may result in loss of compliance, fewer domains might be relevant.
Some of the most commonly used questionnaires in relation to management of spondylolysis are reviewed in this chapter, and the pertinent area of dysfunction covered by each of them is indicated.
FUNCTIONAL OUTCOME
Oswestry Disability Index
The Oswestry Disability Index (ODI) (1,2) is a multiple-choice questionnaire filled out by the patient. It consists of 10 sections related to different activities of daily living. Each section describes six different levels of disability, which are scored by the sections answered and multiplied by 100. The first section rates pain intensity, while the remaining nine cover the disabling effects of pain on typical daily activities: personal care, lifting, walking, sitting, standing, sleeping, sex life, social life, and traveling. This allows potentially irrelevant sections, such as sex life, to be omitted. The Oswestry Disability Index is available in many languages.
Dallas Pain Questionnaire
The Dallas Pain Questionnaire (DPQ) (3) is disease-specific questionnaire in the form of a 16-item visual analogue scale. It was developed by Lawlis et al. to assess the amount
of chronic spinal pain that affects four aspects of the patients’ lives: daily activities, work-leisure activities, anxiety-depression, and social concerns. At our institution, it has been used as the main outcome instrument in several randomized and prospective studies as well as several other studies on the treatment of low back pain (4,5,6,7,8,9). Ozguler et al. (10) recently published a new way of scoring this questionnaire. In a population still in the work force despite low back pain, the authors were able to classify the individuals into one of four groups based on their degree of disability and the presence of emotional distress. We have demonstrated that this classification is of use in relation to spinal fusion patients.
of chronic spinal pain that affects four aspects of the patients’ lives: daily activities, work-leisure activities, anxiety-depression, and social concerns. At our institution, it has been used as the main outcome instrument in several randomized and prospective studies as well as several other studies on the treatment of low back pain (4,5,6,7,8,9). Ozguler et al. (10) recently published a new way of scoring this questionnaire. In a population still in the work force despite low back pain, the authors were able to classify the individuals into one of four groups based on their degree of disability and the presence of emotional distress. We have demonstrated that this classification is of use in relation to spinal fusion patients.
Roland-Morris Disability Questionnaire
Roland-Morris Disability Questionnaire (RDQ) (2,11,12) is a back-specific scale that is completed by selecting 24 items from the Sickness Impact Profile (e.g., “I avoid heavy jobs around the house,” “I sleep less well”) and adding the phrase “because of my back.” Patients completing the RDQ are asked to place a check mark beside a statement if it applies to them that day. The RDQ score is calculated by adding up the number of items checked. Items are not weighted. The scores therefore range from 0 (no disability) to 24 (maximum disability). The scale has become popular among back pain researchers and has been translated into several languages.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree