The Vertebral Column and Other Structures Surrounding the Spinal Cord: Introduction
The spinal cord is an essential highway that carries information between the brain and much of the body. But it is vulnerable to injury arising in the structures that surround it. More than in any other part of the nervous system, pathologic lesions impinging on the spinal cord often originate in the membranes or vertebral column that surround it. The neurologic clinician must, therefore, be very familiar with these structures and their relationship to the spinal cord.
Investing Membranes
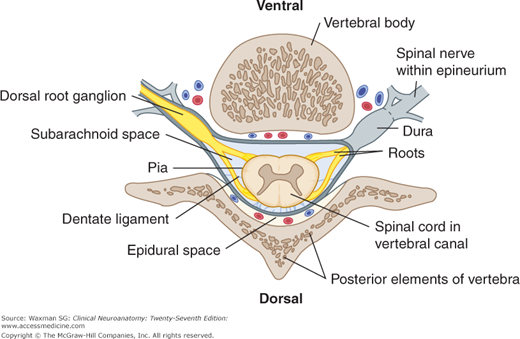
Three membranes surround the spinal cord: The outermost is the dura mater (dura), the next is the arachnoid, and the innermost is the pia mater (pia) (Figs 6–1 and 6–2). The dura is also called the pachymeninx, and the arachnoid and pia are called the leptomeninges.
Figure 6–1
Schematic illustration of the relationships between the spinal cord, spinal nerves, and vertebral column (lateral view), showing the termination of the dura (dura mater spinalis) and its continuation as the filum terminale externum. (Compare with Fig 5–4.)
The dura mater is a tough, fibrous sheath that extends from the foramen magnum to the level of the second sacral vertebra, where it ends as a blind sac (see Fig 6–1). The dura of the spinal cord is continuous with the cranial dura. The epidural, or extradural, space separates the dura from the bony vertebral column; it contains loose areolar tissue and a venous plexus. The subdural space is a narrow space between the dura and the underlying arachnoid.
The arachnoid is a thin, transparent sheath separated from the underlying pia by the subarachnoid space, which contains cerebrospinal fluid (CSF).
The pia mater closely surrounds the spinal cord and sends septa into its substance. The pia also contributes to the formation of the filum terminale internum, a whitish fibrous filament that extends from the conus medullaris to the tip of the dural sac. The filum is surrounded by the cauda equina, and both are bathed in CSF. Its extradural continuation, the filum terminale externum, attaches at the tip of the dural sac and extends to the coccyx. The filum terminale stabilizes the cord and dura lengthwise.
The dentate ligament is a long flange of whitish, mostly pial tissue that runs along both lateral margins of the spinal cord between the dorsal and ventral rootlets (see Fig 6–2). Its medial edge is continuous with the pia at the side of the spinal cord, and its lateral edge pierces the arachnoid at intervals (21 on each side) to attach to the inside of the dura. The dentate ligament helps to stabilize the cord from side to side.
There are eight pairs of cervical nerves. The first seven emerge above each respective cervical vertebra; the eighth (C8) lies below vertebra C7 and above the first thoracic vertebra (see Fig 6–1). Each of the other spinal nerves (T1–12, L1–5, S1–5, and normally two coccygeal nerves, Co1 and Co2) emerges from the intervertebral foramen below the respective vertebra. The cauda equina is made up of dorsal and ventral roots that arise from lumbar and sacral segments of the cord. These roots sweep downward within the dural sac, below the termination of the cord, and give the appearance of a horse’s tail.
As the ventral and dorsal roots (on each side) at each segmental level converge to become a spinal nerve, they are enclosed in sleeves of arachnoidal and dural tissue (see Fig 6–2). The dorsal root sleeve contains the dorsal root ganglion near the point at which both sleeves merge to become the connective tissue sheath (perineurium) of a spinal nerve. The dorsal root (with its ganglion) and the ventral root of the nerve (surrounded by fat and blood vessels) course through the intervertebral foramen, except in the sacral segments where the dorsal root ganglia lie within the sacrum itself.
Spinal Cord Circulation
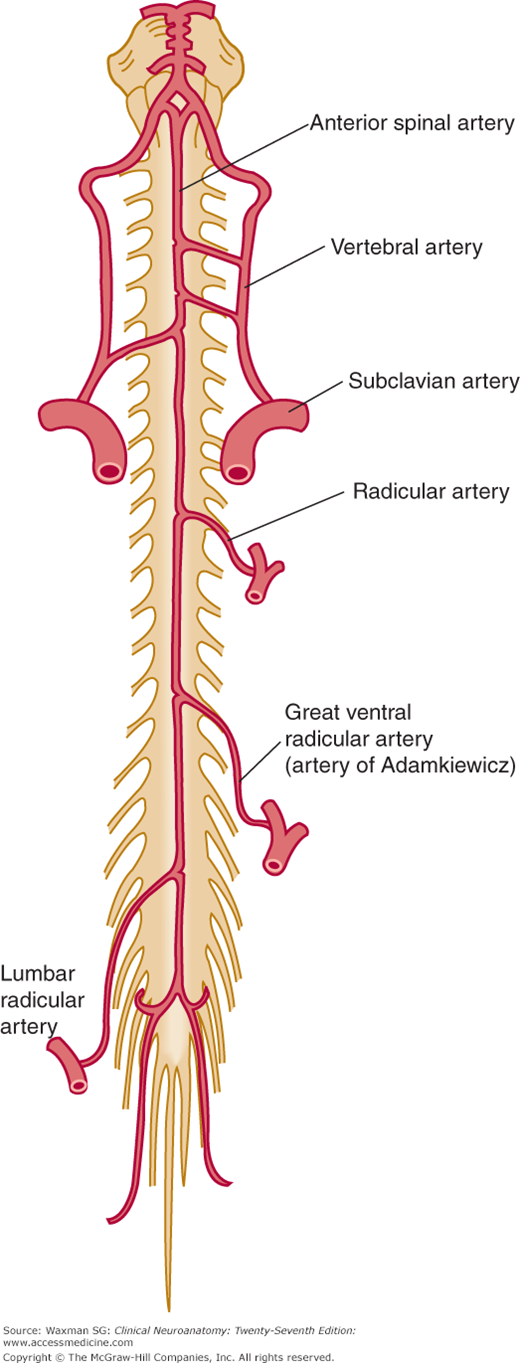
This artery is formed by the midline union of paired branches of the vertebral arteries (Figs 6–4 and 6–5). It descends along the ventral surface of the cervical spinal cord, narrowing somewhat near T4.
This artery is the prolongation of the anterior spinal artery below T4.
These arteries arise from the vertebral arteries and course downward to the lower cervical and upper thoracic segments.
Some (but not all) of the intercostal arteries from the aorta supply segmental (radicular) branches to the spinal cord from T1 to L1. The largest of these branches, the great ventral radicular artery, also known as the artery of Adamkiewicz, enters the spinal cord between segments T8 and L4 (see Fig 6–5). This artery usually arises on the left and, in most individuals, supplies most of the arterial blood supply for the lower half of the spinal cord. Although occlusion in this artery is rare, it results in major neurologic deficits (eg, paraplegia, loss of sensation in the legs, urinary incontinence).
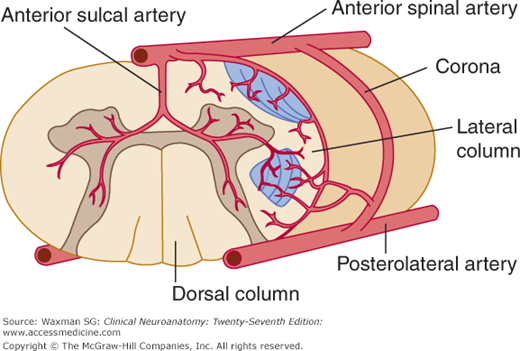
These paired arteries are much smaller than the single large anterior spinal artery; they branch at various levels to form the posterolateral arterial plexus. The posterior spinal arteries supply the dorsal white columns and the posterior portion of the dorsal gray columns.
In each segment, the branches of the radicular arteries that enter the intervertebral foramens accompany the dorsal and ventral nerve roots. These branches unite directly with the posterior and anterior spinal arteries to form an irregular ring of arteries (an arterial corona) with vertical connections. Sulcal arteries branch from the coronal arteries at most levels. Anterior sulcal arteries arise at various levels along the cervical and thoracic cord within the ventral sulcus (see Fig 6–4); they supply the ventral and lateral columns on either side of the spinal cord.
An irregular external venous plexus lies in the epidural space; it communicates with segmental veins, basivertebral veins from the vertebral column, the basilar plexus in the head, and, by way of the pedicular veins, a smaller internal venous plexus that lies in the subarachnoid space. All venous drainage is ultimately into the venae cavae. Both plexuses extend the length of the cord.
Clinical Correlations
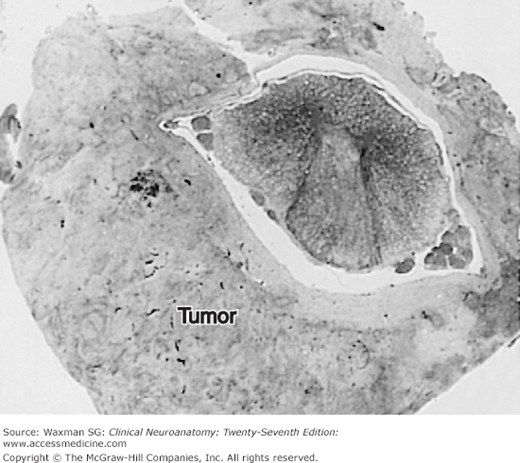
Abnormal masses (tumors, infections, hematomas) may occur in any location in or around the spinal cord. Tumors (eg, meningiomas, neurofibromas) are often located in the intradural extramedullary compartment. Epidural masses, including bone tumors or metastases, can displace the dura locally and compress the spinal cord (Fig 6–3). Spinal cord compression may progress rapidly and can result in paraplegia or quadriplegia. If diagnosed early, however, it may be readily treated. Thus, suspected spinal cord compression requires urgent workup. Intradural extramedullary masses, most often in the subarachnoid space, may push the spinal cord away from the lesion and may even compress the cord against the dura, epidural space, and vertebra. Intramedullary, and therefore intradural, masses expand the spinal cord itself (see Fig 5–24). An epidural mass is usually the least difficult to remove neurosurgically. Clinical Illustration 6–1 describes a patient with an epidural abscess.
Clinical Illustration 6–1
A 61-year-old former house painter with a history of alcoholism was admitted to the medical service after being found in a hotel room in a confused state that was attributed to alcohol withdrawal syndrome. The patient did not complain of pain but said he was weak and could not get out of bed. He had a fever. The intern’s initial neurologic examination did not reveal any focal neurologic signs. The lumbar puncture yielded CSF containing a moderate number of white blood cells and protein of about 100 mg/dL (elevated) with normal CSF glucose. Despite treatment with antibiotics, the patient did not improve, and neurologic consultation was obtained.
On examination, the patient was confused and uncooperative. He stated he was weak and could not walk. Motor examination revealed flaccid paraparesis. Deep tendon reflexes were absent in the legs, and the plantar responses were extensor. The patient was not cooperative for vibratory or position sense testing. He denied feeling a pin as painful over any part of the body; however, when the examiner watched for a facial wince on pinprick, a sensory level T5–6 could be demonstrated. On gentle percussion of the spinal column, there was tenderness at T9–10.
Imaging of the spinal column revealed an epidural mass. The patient was taken to surgery, and an epidural abscess, extending over five vertebral segments, was found. The spinal cord under the abscess was compressed and pale, probably as a result of ischemia (vasospasm leading to inadequate perfusion with blood).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree