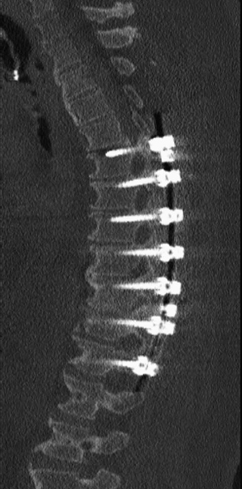
71 A 60-year-old man had a history of abdominal surgery and subsequent peritonitis with resultant septicemia and thoracic osteomyelitis. He was left with disabling midthoracic pain and radiculopathy in the months thereafter. He had no neurologic deficit, but pain to percussion of his thoracolumbar junction. FIGURE 71-1 Sagittal reconstructed CT of the thoracic spine displays the area of previous infection, now beginning to autofuse. Sagittal reconstructed computed tomography (CT) of the thoracic spine displays a T10-T11 area of partial autofusion from chronic osteomyelitis/discitis (Fig. 71-1). Mechanical back pain following a previous osteomyelitis A T6-T12 pedicle screw fusion was completed (Figs. 71-2 and 71-3). Osteomyelitis of the spine is not uncommonly encountered in general practice, particularly if one is in a metropolitan location. The risks in older people are immunocompromise, chronic dialysis, and diabetes. The risks in younger people are intravenous drug abuse and HIV. The treatment is normally medical, with 3 months of a directed antibiotic. The offending pathogen can be discovered through blood cultures and a CT-guided biopsy. Surgery has two roles in this disease: decompression when the patient has neurologic compromise, and in patients with progressive deformity. Deformity can present with mechanical back pain. Instrumentation and autograft or allograft can be used to stabilize an unstable spine while the patient is infected, as long as a course of intravenous antibiotics is maintained.
Thoracic Osteomyelitis
Presentation

Radiologic Findings
Diagnosis
Treatment
Discussion
Thoracic Osteomyelitis
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








