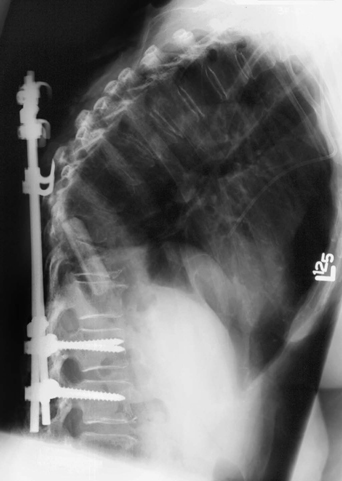
59 A 70-year-old woman presented with metastatic breast cancer and cord compression. She had previously undergone decompression and fusion for acute cord compression. Postoperatively, she regained some ambulation, then presented 3 weeks later with acute back pain and wound dehiscence. The upper thoracic construct failed, as demonstrated on the lateral thoracic x-ray (Fig. 59-1). Hardware extrusion The patient underwent a wound irrigation and debridement with revision of her thoracolumbar fusion. Patients with metastatic spine disease are a challenge when major surgery is planned. The decision making is multifactorial. Life expectancy, the compromised quality of pathologic bone, staging, and overall condition are considered. Additionally, the degree of spine involvement, the presence or absence of cord compression, neurologic status, bone quality, and the patient’s outlook on the disease and a possible major surgery must all be contemplated. If the decision to go to surgery has been made, the option of anterior versus posterior approach is weighed.
Thoracolumbar Instrumentation Failure
Presentation
Radiologic Findings
Diagnosis
Treatment
Discussion
Thoracolumbar Instrumentation Failure
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








