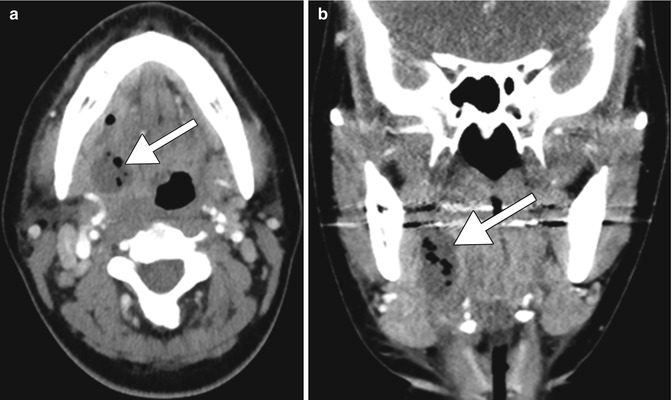
Fig. 1.1
Embolic infarct. This smoker presented with acute left hemiplegia. Non-contrast axial CT image (a) shows a hypoattenuation within the right MCA territory (arrow). 3D CTA image (b) shows occlusion of the right MCA (expected location encircled)
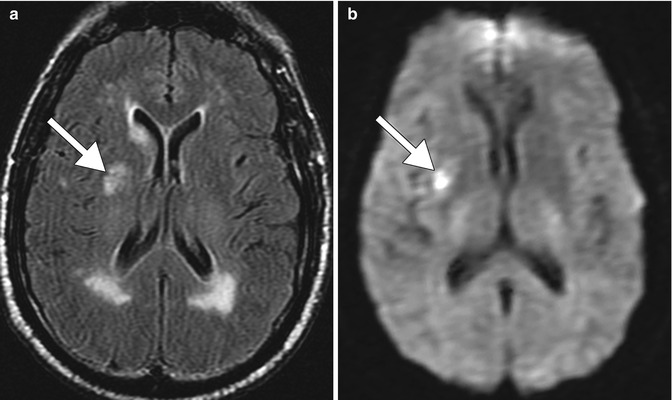
Fig. 1.2
Lacunar infarct and small vessel ischemic disease. The patient is a smoker who presented with acute neurological deficits. Axial FLAIR (a) and DWI (b) images show a recent right basal ganglia lacunar infarct (arrows). There is also diffuse, confluent periventricular white matter T2 hyperintensity as well as mild scattered, punctate subcortical white matter T2 hyperintense foci without corresponding restricted diffusion, which is consistent with chronic small vessel ischemic disease
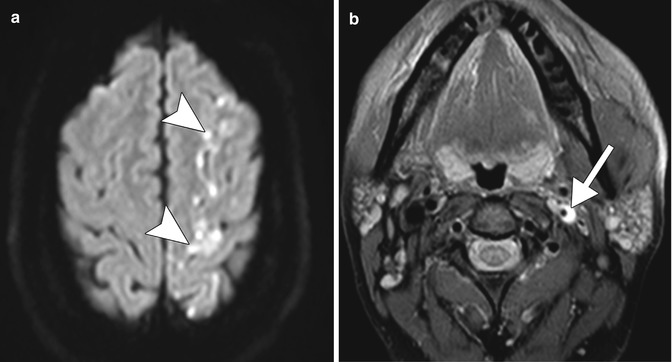
Fig. 1.3
Carotid dissection. Axial DWI (a) shows restricted diffusion in the left ACA-MCA watershed territory (arrowheads). The axial fat-suppressed T1 MRA (b) shows hyperintensity surrounding the narrow left internal carotid artery flow void, compatible with intramural hemorrhage (arrow)
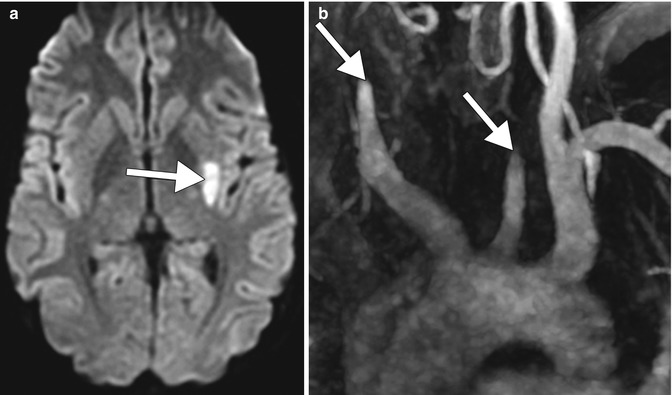
Fig. 1.4
Takayasu arteritis. Axial DWI (a) shows a focus of restricted diffusion in the left external capsule (arrows). MIP MRA (b) shows lack of flow-related enhancement beyond the proximal common carotid arteries bilaterally (arrows)
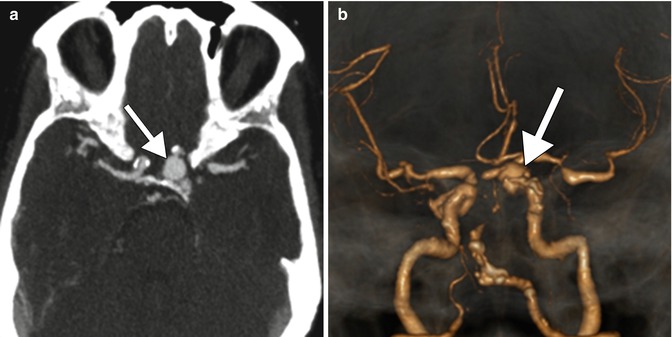
Fig. 1.5
Cerebral aneurysm. A former 20-pack-year smoker underwent evaluation for a suspected stroke. Axial (a) and 3D volume rendered (b) CTA images show a left paraclinoid internal carotid artery saccular aneurysm (arrow). There is also extensive atherosclerotic narrowing of the cerebral vasculature noted in both the anterior and posterior circulation bilaterally
1.3.2 Cerebral Aneurysm
Besides smoking, additional risk factors that predispose to aneurysm formation include fenestrated arteries (Fig. 1.6), fibromuscular dysplasia, neurofibromatosis, alpha-1-antytripsyn deficiency, and connective tissue disorders, such as Ehlers-Danlos syndrome and Marfan’s syndrome and polycystic kidney disease. Otherwise, the differential diagnosis of a cerebral aneurysm on radiologic imaging includes an infundibulum (usually manifests as a triangular dilatation with the vessel arising from the apex that measures less than 2 mm), pseudoaneurysm, and mycotic aneurysm (Fig. 1.7).
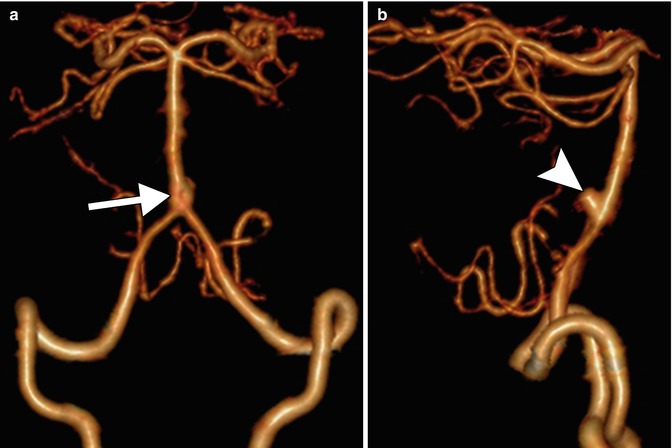
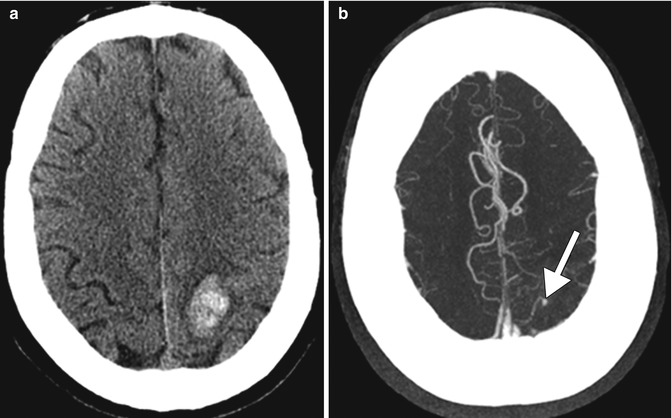
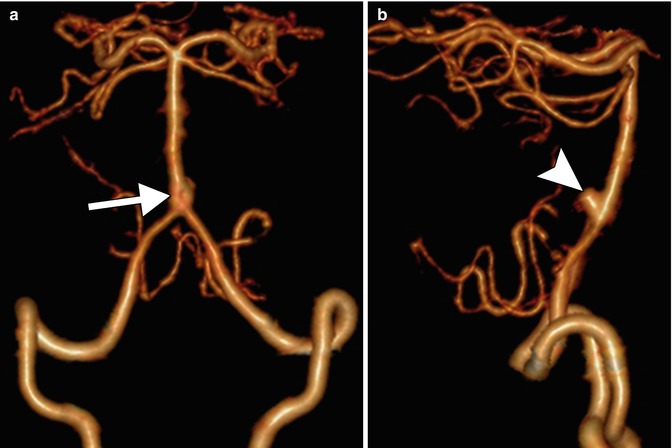
Fig. 1.6
Arterial fenestration. Frontal projection 3D volume rendered CTA image (a) shows a fenestration of the proximal basilar artery (arrow). Lateral projection 3D volume rendered CTA image (b) shows a dorsally oriented aneurysm arising from the caudal aspect of the fenestration (arrowhead)
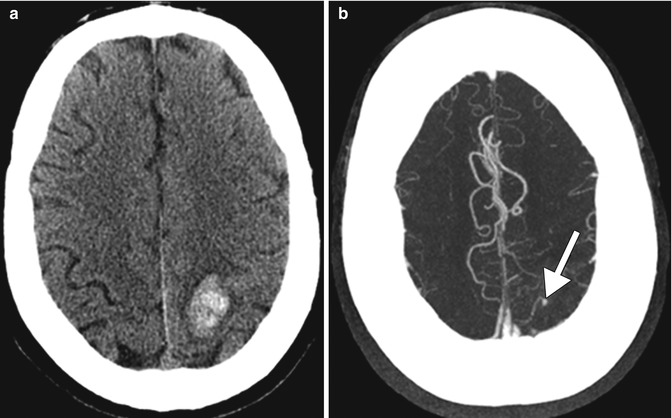
Fig. 1.7
Mycotic aneurysm. Axial CT image (a) shows left peri-rolandic hemorrhage. Axial MIP CTA image (b) shows a small outpouching arising from a cortical artery (arrow)
1.3.3 Cerebral Venous Thrombosis
1.3.4 Head and Neck Cancer, Squamous Cell Carcinoma
Tobacco smoking, along with alcohol, is well established as the dominant risk factor for head and neck squamous cell carcinoma (HNSCC). This risk is correlated with the intensity and duration of tobacco use and is synergistic with concomitant alcohol consumption. There are more than sixty recognized compounds in tobacco that have a specific carcinogenic potential. In particular, nitrosamines and polycyclic hydrocarbons can alter the molecular profile of an individual and causes mutations. Nicotine, originally thought only to be responsible for tobacco addiction, is also involved in tumor promotion and progression with antiapoptotic and indirect mitogenic properties. Other factors that can increase the risk of HNSCC include HPV infection and certain occupational exposures. Imaging with contrast-enhanced CT and MRI allows depiction of the anatomy of the larynx and submucosal tumor extension.
Dual-energy CT improves the diagnostic performance and interobserver reproducibility of evaluations of laryngeal cartilage invasion by squamous cell carcinoma. CT, MRI, and PET-CT also provide information regarding cervical nodal disease, systemic metastases, and synchronous malignancies.
On CT or MRI, head and neck squamous cell carcinomas often manifest as ill-defined enhancing masses. Aggressive features of HNSCC include tissue invasion and necrosis (Fig. 1.8). The most common sites of head and neck squamous cell cancer are the floor of the mouth, tongue, soft palate, anterior tonsillar pillar, and retromolar trigone. In addition to locoregional spread, HNSCC can metastasize to distant organs hematogenously, most commonly to the lungs and bones. Metastasis to the brain is an infrequent, but carries a poor prognostic outcome (Fig. 1.9). Besides smoking, alcohol (refer to Chap. 2), betel nuts (refer to Chap. 8), and HPV are the other major risk factors for head and neck squamous cell carcinoma. Interestingly, HPV-positive squamous cell carcinomas generally have a more favorable prognosis and tend to have tumors that are relatively well-defined and large cystic nodal metastases (Fig. 1.10). Otherwise, the differential for other malignant cancers in the head and neck include thyroid cancer, lymphoma, salivary gland cancer, and sarcoma. Furthermore, head and neck abscesses can sometimes resemble necrotic or ulcerated head and neck squamous cell carcinomas and nodal metastases (Fig. 1.11).
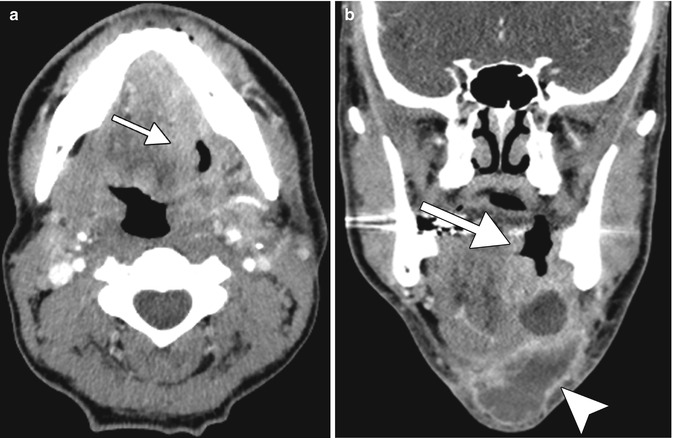
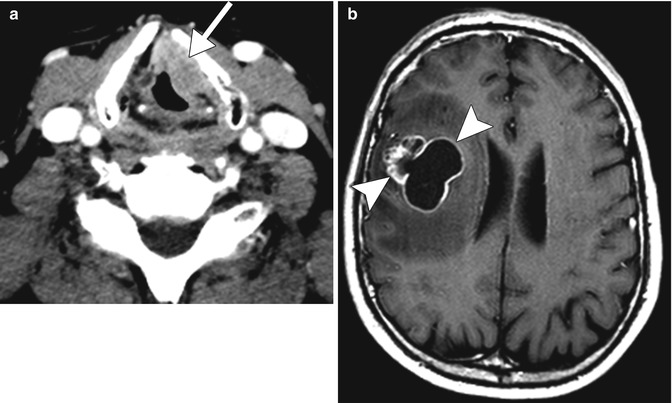
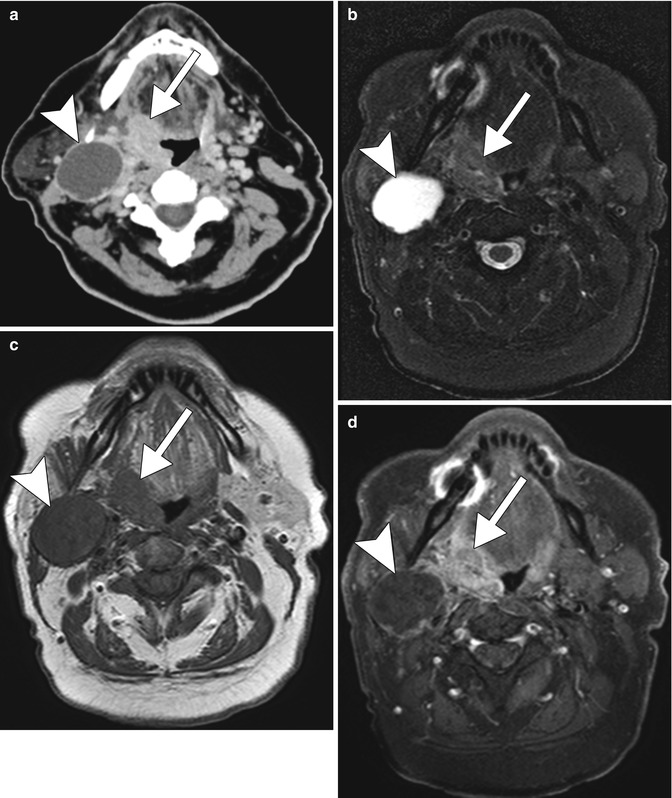
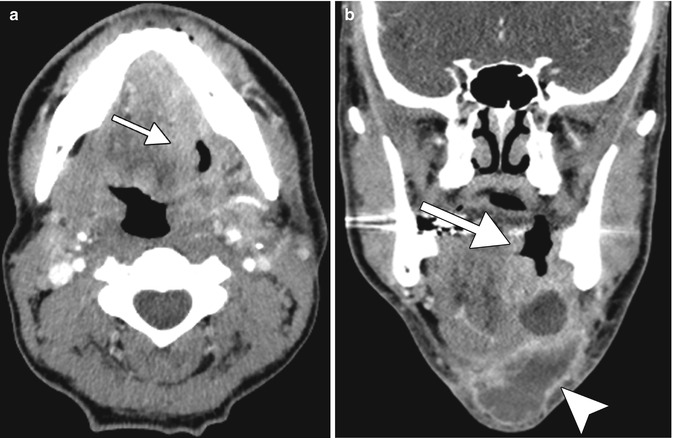
Fig. 1.8
Oral squamous cell carcinoma in a 30-pack-year male smoker. Axial (a) and coronal (b) post-contrast CT images show an ulcerating mass in the left floor of the mouth and oral tongue (arrows) with associated submental necrotic cervical lymphadenopathy (arrowhead)
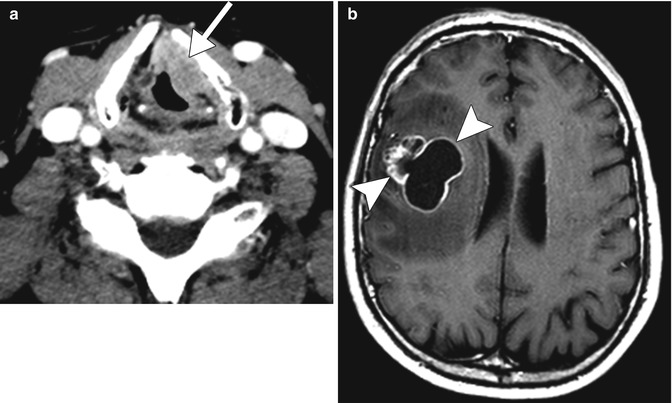
Fig. 1.9
Laryngeal squamous cell carcinoma with brain metastasis. This 25-pack-year smoker had been recently diagnosed with laryngeal squamous cell carcinoma when he developed generalized seizures. Axial CT image (a) shows a left vocal cord mass (arrow) that also involves the paraglottic fat and anterior commissure. Post-contrast T1-weighted MRI image (b) demonstrates a heterogeneous metastatic lesion in the right frontal lobe (arrowheads)
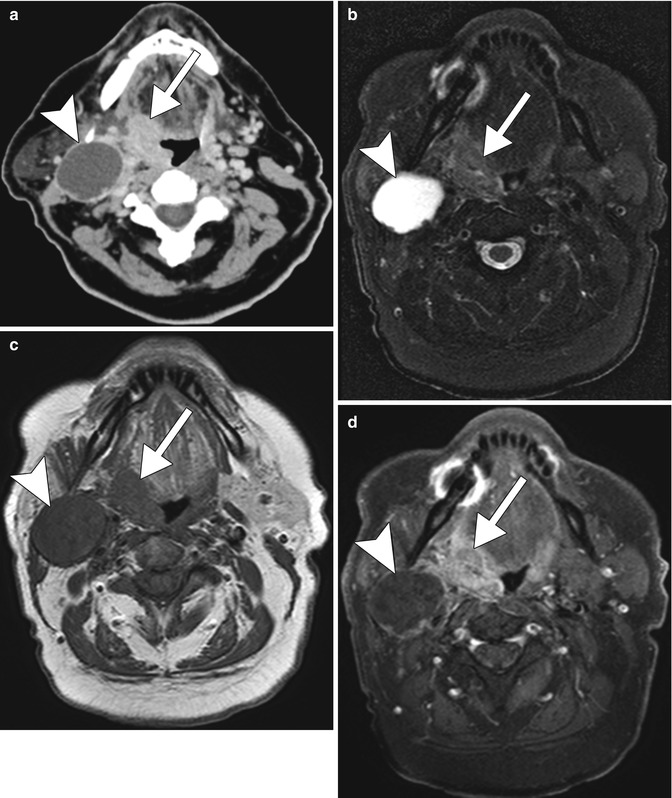
Fig. 1.10
HPV-positive squamous cell carcinoma. Axial CT (a) and axial fat-suppressed T2-weighted (b), axial T1-weighted (c), and axial fat-suppressed post-contrast T1-weighted (d) images show a relative well-demarcated right palatine tonsil tumor (arrows) and a large metastatic lymph node with cystic necrosis (arrowheads)