, Katsuro Tomita1 and Hiroyuki Tsuchiya1
(1)
Kanazawa University, Kanazawa, Japan
Conventionally, because of the difficulty in surgical approach and the anatomical proximity of the major vessels to the involved vertebra(e), curettage and resection of vertebral tumors have been commonly practiced, including removal of the malignant tissue in a piecemeal fashion. The disadvantages of these conventional approaches are clear, including a high possibility of tumor cell contamination of the surrounding structures and difficult identification of a demarcation zone separating neoplastic tissue from healthy tissue. These factors may contribute to incomplete resection of the tumor as well as recurrence of the spinal malignant neoplasm [1 , 2].
To reduce local recurrence as much as possible and to increase survival rate, we have developed a new surgical technique of spondylectomy (vertebrectomy) termed total en bloc spondylectomy (TES) [1 – 5]. Using this technique, we were able to excise the tumor mass with a wide or narrow margin, but sometimes with an minimal intralesional margin in the pedicle.
Indications for Total En Bloc Spondylectomy
The TES operation was designed primarily for patients who met the following criteria: a primary malignant tumor, aggressive benign tumor, or solitary metastasis that did not spread into or invade adjacent visceral organs, showed little or no adhesion to the vena cava or aorta, and did not show multiple metastases. A contiguous involvement of three or fewer vertebrae represented a relative indication for the TES operation.
The indications for surgical treatment of spinal metastases are neurologic deficit, intractable pain, and spinal instability. The oncologic factors to be considered include the success of treatment of the primary tumor, whether the metastases are solitary and localized, if the metastases are limited and can be controlled, and if there is a life expectancy of at least 12 months.
To provide a more informative staging, a new surgical classification was devised that incorporated a description of the affected anatomical site and the extent of the tumor. The anatomical site of the neoplasm was classified as follows: (1) vertebral body, (2) the pedicle, (3) the lamina and spinous process, (4) spinal canal (epidural space), and (5) paravertebral area (Fig. 53.1). The numbers used to denote the anatomical sites reflect the common sequence of tumor progression. The number of anatomical sites is also related to the surgical classification as described here. Using the anatomical and surgical classification, the new surgical classification of vertebral tumors was designed (Fig. 53.2). The classification concept was modified from the surgical staging system of Enneking and coworkers [6]. For instance, type 3 lesion in our classification involves the vertebral body (anatomical site 1), the pedicle (anatomical site 1), and the lamina (anatomical site 3). We considered type 1, 2, and 3 lesions as intracompartmental and types 4, 5, and 6, as extracompartmental. Type 7 tumor is a multiple skip lesion. The TES operation is recommended for type 2, 3, 4, and 5 lesions, relatively indicated for type 1 and 6 lesions, and not recommended or contraindicated for type 7 lesions.
Fig. 53.1
Definitions of anatomical sites of the vertebra. (From Tomita N, et al: Int Orthop 18:292, 1994)
Fig. 53.2
Schematic diagram of surgical classification of vertebral tumors. (From Tomita N, et al: Int Orthop 18:292, 1994)
Surgical Technique
The TES technique consists of two steps: en bloc resection of the posterior element and en bloc resection of the anterior column. The following is a description of each step.
Step 1: En Bloc Laminectomy (En Bloc Resection of the Whole Posterior Element of the Vertebra)
1.
Exposure
The patient is placed prone over the Relton–Hall four-poster frame to avoid compression to the vena cava. A straight vertical midline incision is made over the spinous processes and is extended three vertebrae above and below the involved segment(s). The paraspinal muscles are dissected from the spinous processes and the laminae, and then retracted laterally. If the patient underwent posterior route biopsy, the tracts are carefully resected in a manner similar to that used in a limb-salvaging procedure. After a careful dissection of the area around the facet joints, a large articulated spinal retractor is applied. By spreading the retractor and detaching the muscles around the facet joints, a wider exposure is obtained. The operative field must be wide enough on both sides to allow dissection under the surface of the transverse processes. In the thoracic spine, the ribs on the affected level are transected 3 to 4 cm lateral to the costotransverse joint, and the pleura is bluntly separated from the vertebra (Fig. 53.3).
Fig. 53.3
Operative schema of the posterior exposure
To expose the superior articular process of the uppermost vertebra, the spinous and the inferior articular processes of the neighboring vertebra are osteotomized and removed with dissection of the attached soft tissues, including the ligamentum flavum.
2.
Introduction of the T-Saw Guide
To make an exit for the T-saw guide through the nerve root canal, the soft tissue attached to the inferior aspect of the pars interarticularis is dissected and removed, using utmost care so as not to damage the corresponding nerve root. A C-curved malleable T-saw guide is then introduced through the intervertebral foramen in a cephalocaudal direction. In this procedure, the tip of the T-saw guide should be introduced along the medial cortex of the lamina and the pedicle so as not to injure the spinal cord and the nerve root (Fig. 53.4). After passing the T-saw guide, its tip at the exit of the nerve root canal can be found beneath the inferior border of the pars interarticularis. In the next step, a threadwire saw (T-saw; flexible multifilament threadwire saw, 0.54 mm in diameter7; Fig. 53.5) is passed through the hole in the wire guide and is clamped with a T-saw holder at each end. The T-saw guide is removed, and tension on the T-saw is maintained. When two or three vertebrae are resected, the T-saw is inserted into a thin polyethylene catheter (T-saw catheter) and both are passed under the lamina. This procedure is also applied to the contralateral side.
Fig. 53.4
Operative schema of introducing the T-saw guide
Fig. 53.5
Photograph of the thread-wire saw (T-saw) compared with a Gigli saw and a match
3.
Cutting the Pedicles and Resection of the Posterior Element
While tension is maintained, the T-saw is placed beneath the superior articular and transverse processes with a specially designed T-saw manipulator. With this procedure, the T-saw placed around the lamina is wrapped around the pedicle. With a reciprocating motion of the T-saw, the pedicles are cut and then the whole posterior element of the spine (the spinous process, the superior and inferior articular processes, the transverse process, and the pedicle) is removed in one piece (Fig. 53.6). The cut surface of the pedicle is sealed with bone wax to reduce bleeding and to minimize contamination by tumor cells. To maintain stability after segmental resection of the anterior column, a temporary posterior instrumentation is performed (Fig. 53.7). When one vertebra is resected, segmental fixation at two above and two below is recomended. However, if two or three vertebrae are resected, more than two above and two below segmental fixation is mandatory.
Fig. 53.6
Operative schema of the pediclotomy
Fig. 53.7
Operative schema of setting the posterior instrumentation
Step 2: En Bloc Corpectomy (Resection of the Anterior Column of the Vertebra)
1.
Blunt Dissection Around the Vertebral Body
At the beginning of the second step, the segmental arteries must be identified bilaterally. The spinal branch of the segmental artery, which runs along the nerve root, is ligated and divided. This procedure exposes the segmental artery, which appears just lateral to the cut edge of the pedicle. In the thoracic spine, the nerve root is cut on the side from which the affected vertebra is removed. The blunt dissection is done on both sides through the plane between the pleura (or the iliopsoas muscle) and the vertebral body. Usually, the lateral aspect of the body is easily dissected with a curved vertebral spatula. Then, the segmental artery should be dissected from the vertebral body. By continuing dissection of both lateral sides of the vertebral body anteriorly, the aorta is carefully dissected posteriorly from the anterior aspect of the vertebral body with a spatula and the surgeon’s fingers (Fig. 53.8a, 53.8b). When the surgeon’s fingertips meet anterior to the vertebral body, a series of spatulas, starting from the smallest size, are inserted sequentially to extend the dissection. A pair of the largest spatulas is kept in the dissection site to prevent the surrounding tissues and organs from iatrogenic injury and to make the surgical field wide enough for manipulating the anterior column.
Fig. 53.8
(a, b) Operative schema of anterior dissection around the vertebral body
2.
Vascular Anatomy Around the Vertebral Body
It is important to understand vascuar anatomy around the vertebral body [8]. The first four segmental (posterior intercostal) arteries commonly run directly upward apart from the vertebral column and turn more transversely over the costovertebral joint (Fig. 53.9). The azygos vein cephalad to T4 ascends away from the vertebral column (Fig. 53.10). This anatomical specificity in the upper thoracic area indicates that there is a decreased chance of critical damage to these vessels during isolation of the affected vertebral body and paired discs posteriorly in total en bloc spondylectomy.
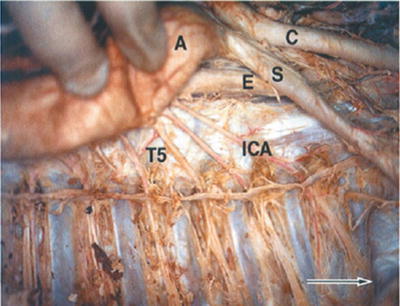
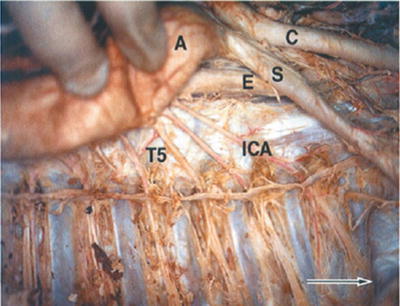
Fig. 53.9




Topographic view of the aortic arch and posterior intercostal arteries at the upper thoracic spine on the right side in the cadaveric study.8 The highest aortic arch level was at T3–T4, and the subsequent thoracic aorta descends in direct contact with the vertebrae at T5 or below. The second to fourth posterior intercostal arteries originate from the aorta at T5. C, common carotid artery; S, subclavian artery; E, esophagus; A, aortic arch; T5, T5 vertebral body; ICA, intercostal artery. Arrow indicates the cranial direction. (From Kawahara N, et al: Spine 21 (12):1402, 1996)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








