♦ Preoperative
Operative Planning
- Appropriate imaging
- Magnetic resonance imaging (MRI)
- Computed tomography myelogram if MRI inconclusive or with artifact
- Flexion/extension x-rays
- Oblique lumbar x-rays
- Discogram (optional)
- Magnetic resonance imaging (MRI)
Patient Counseling Regarding Surgical Risks
- Cerebrospinal fluid leaks
- Pseudoarthrosis
- Nerve root injury (foot drop)
- Wound infection
- Hardware misplacement or migration
- Basic spine tray
- Interbody spine tray (interbody curettes and rasps, ¼-in osteotome, interbody dilators, pedicle screw awl, guide, tap)
- High-speed drill (Midas Rex with AM-8 bit)
- Kerrison punches
- Optional: mini open retractors
- X-tube (Medtronic)
- Pipeline (DePuy)
- X-tube (Medtronic)
Operating Room Set-up
- Headlight
- Loupes
- Microscope (optional)
- Bipolar cautery and Bovie cautery
- Intraoperative fluoroscopy
- X-ray compatible table
- Cell saver (optional for mini-open cases)
Anesthetic Issues
- Patient’s pulmonary function should be sufficient to tolerate prone position
- Intravenous antibiotics: cefazolin 2 g (for adults) or vancomycin in the case of a penicillin allergy
- Foley catheter for prolonged surgery
- Steroids (optional)
- Electrophysiological monitoring (optional)
- Dynamic compression stockings
♦ Intraoperative
Positioning
- On a standard operating room table, the patient is placed prone on chest rolls to recreate physiological lumbar lordosis.
- The operating table is placed in reverse position with the base of the table under the patient’s knees. This facilitates intraoperative fluoroscopy.
- The surgeon must avoid placing the patient in a flat-back or kyphotic position.
- For L4–L5 level fusions, the operating table is kept parallel to the floor. For L5–S1 fusion, the operating table maybe placed in 20 to 30 degrees of reverse Trendelenburg to facilitate the view of the inferiorly angled L5–S1 disc space.
- Arms brought forward to facilitate anesthetist’s access to intravenous lines.
Depilation
- Electric razors, conventional disposable razors
- Hair removers require application and removal 24 hours in advance
- Betadine sterile scrub for 5 minutes, toweled off, and followed by Betadine paint. Paint is allowed to completely dry prior to incision.
- DuraPrep (iodine/isopropyl alcohol): single painted surface allowed to completely dry
Incision Planning
- May be approximated by the lateral iliac crest landmark or with fluoroscopy prior to incision
Exposure
- Subperiosteal dissection of the posterior spinal elements, including the transverse processes for the levels to be fused
- Curved Weitlaner retractors are adequate for slender patients. Curved cerebellar retractors or Zelpi retractors (Life Instruments Inc., Braintree, MA) may be helpful for more sizeable patients.
- Soft tissue overlying the spine is removed in preparation to harvest local autologous bone for bone graft.
- For mini-open procedures with expandable retractors, muscle splitting Wiltse approach is adequate.
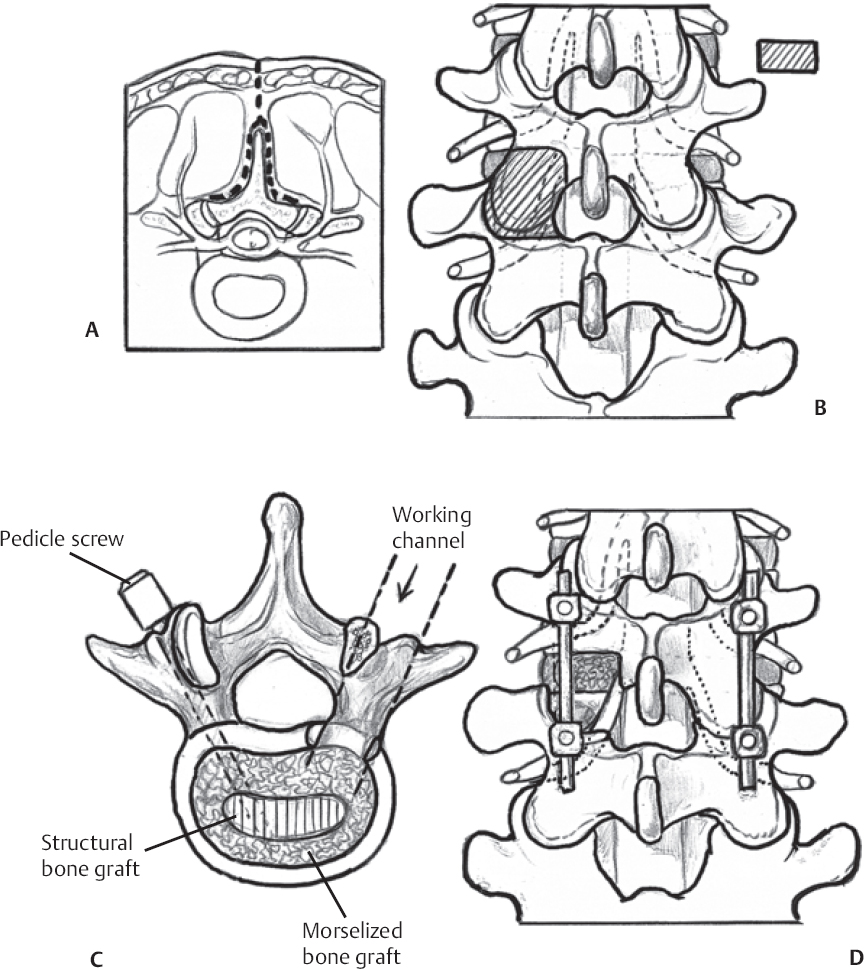
Decompression (Fig. 124.1A)
- A laminectomy, facetectomy, or both may be performed depending on the clinical presentation. A unilateral laminotomy and complete facetectomy are performed on the more symptomatic side.
- Bilateral laminectomies are reserved for patients in whom preoperative imaging has revealed clinically significant bilateral neural element compression.
- All bone is collected and morselized for autograft.
Pedicle Screw Placement, Disc Distraction, and Endplate Preparation
- After adequate decompression, pedicle screws are placed in the standard fashion. A rod is secured after distraction of the levels.
- The disc space is identified, and a standard discectomy is performed.
- The posterior lip of each endplate may be removed with the use of a ¼-in osteotome, while carefully protecting the thecal sac and nerves.
- Endplates are prepared with rasps and curettes.
Interbody Fusion (Fig. 124.1B)
- After complete disc removal from a posterolateral approach, several interbody dilators are used to distract the disc space.
- An appropriate size cage is selected using specifically designed trials.
- A portion of the previously collected cancellous autograft, along with either iliac crest bone graft or recombinant bone morphogenetic protein-2 (rh-BMP-2 [INFUSE, Sofamor Danek, Memphis, TN]) sponge, is packed into the anterior disc space and into the cage. Interbody cages made of allograft, polyetheretherketone, titanium, and carbon fiber are all available.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree