(1)
Cedars-Sinai Spine Center, Los Angeles, CA, USA
The patient is placed in the supine position on a Jackson table with an inflatable bag under the lumbar spine in case extension becomes necessary during the procedure. Shoulder supports should be placed, and straps applied across the thighs and chest to prevent the patient from slipping when placed in the deep Trendelenburg position. The table itself needs to be rigged so the maximum Trendelenburg position can be achieved. This positioning is very important so that the bowel can be kept away from the target area by using gravity rather than retractors. In addition, this position places the L5–S1 disc at a better angle for performance of the discectomy. A Foley catheter and a nasogastric tube are inserted to minimize obstruction to access by either a distended bladder or stomach, and to prevent injury to the bladder from trocar insertion near the symphysis pubis.
With the patient in the moderate Trendelenburg position, a small infraumbilical incision is made and a Veress needle inserted into the peritoneal cavity. Insufflation is then carried out to 15 mmHg, and then a 10-mm trocar is inserted followed by passage of the laparoscope. Two other 10-mm trocars are then inserted under direct vision to prevent inadvertent injury to any peritoneal contents. These trocars are placed at the midclavicular line to the right and to the left of the umbilicus (Figs. 31.1, 31.2). Careful exploration of the peritoneal cavity is then carried out for any other obvious pathology that may interfere with the planned procedure. If adhesions are found, they are then taken down using graspers for traction and endoscissors with cautery for dissection. Adhesions need to be taken down to allow for proper mobilization of the small bowel away from the pelvis and into the upper abdomen. If the bowel should be injured in this process, repair with endoscopic stapling devices can be carried out. If endoscopic repair proves difficult, an open laparotomy is then indicated. Under these circumstances, the endoscopic approach must then aborted because of the resulting contamination by bowel contents. The procedure, however, may be completed via the anterior muscle-sparing extraperitoneal approach if so desired, assuming the contamination is minimal and the peritoneum is not entered during the extraperitoneal dissection.
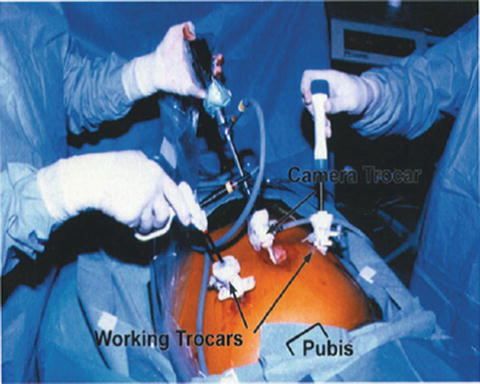
Fig. 31.1
Schematic of proper positioning of the trocars for L5–S1 fusion
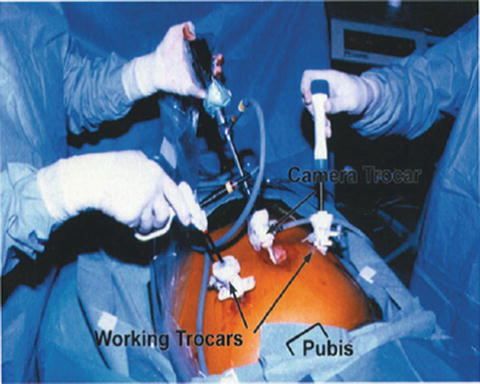
Fig. 31.2
The 10-mm upper trocars are in proper locations with instruments inserted into the peritoneal cavity
After completion of the exploration, assuming there are no abnormal findings, the patient is placed in the deepest possible Trendelenburg position and the bowel is mobilized cephalad; this is done by first grasping the omentum with endoscopic Babcock forceps and draping it up over the stomach. The loops of small bowel are then grasped and carried cephalad to the upper abdomen to expose the sacral promontory. If the Trendelenburg position is adequate, gravity should keep these loops of bowel from obscuring the operative field for the duration of the procedure. The sigmoid colon may then need to be mobilized from its lateral peritoneal attachments using graspers and cautery and then also pushed cephalad toward the left upper quadrant. At this point, a fan retractor needs to be placed through the left trocar to hold the sigmoid colon laterally away from the sacral promontory (Fig. 31.3).
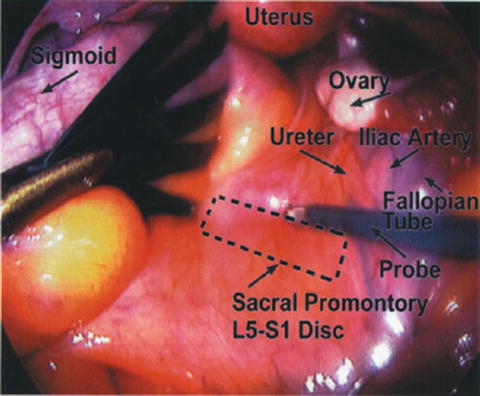
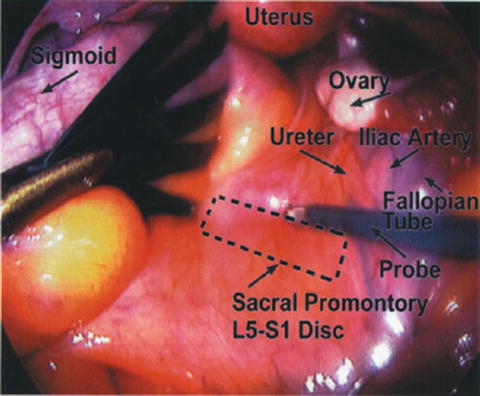
Fig. 31.3
Sacral promontory with sigmoid colon retracted to the left and iliac vessels and ureter under grasper to the right
The aortic bifurcation and both right and left iliac vessels as well as the right ureter can be easily identified at this point. The left ureter is not easy to visualize because it lies under and lateral to the mesocolon. Gentle poking with a blunt grasper is carried out between the iliac vessels until the sacral promontory becomes obvious. In all but the very obese patients, this landmark is easy to visualize and the poking simply serves to confirm its identification. The peritoneum overlying this area is then gently lifted and carefully incised transversely with endoscissors and without using any cautery to avoid injury to sympathetic fibers. There is an avascular plane here that allows incision of the peritoneum without any bleeding whatsoever.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








