Chapter 65 Trauma Surgery
Cervical Spine
Injury to the cervical spine should be suspected in any patient complaining of neck pain after trauma. Initial management of the multiply injured patient will be dictated by established advanced trauma life support (ATLS) protocols, with priority directed to management of airway, breathing, and circulatory compromise. The “chin lift and jaw thrust” method of securing an airway may decrease the space available for the spinal cord (beyond that seen with nasal or oral intubation) and should be avoided in the patient with a known or suspected cervical spine injury. Spinal precautions (to include cervical spine immobilization) should be maintained throughout the early stages of evaluation and resuscitation of the multitrauma patient.1 The most common causes of injury to the neck are motor vehicle accidents (MVAs), diving into shallow water, and sport-related activities. A thorough history of a given accident may further influence clinical suspicion for the presence of a cervical spine injury. Did the patient strike his or her head? Was there evidence of cranial impact to the windshield from inside the vehicle? Was the patient ejected? Was there any indication of weakness or paralysis noted at the accident scene? Was the patient neurologically intact at the scene with later deterioration in neurologic function? Information gathered through such questioning will guide clinical suspicion for neck injury and may provide important prognostic information when neurologic compromise is present. Obtaining information regarding prior history of injury, underlying preexisting cervical spine disease, or systemic conditions (e.g., ankylosing spondylitis) is important as well.
The physical examination of the patient with known or suspected cervical spine injury begins at the patient’s head and progresses distally. It is complete only after a thorough evaluation of the entire musculoskeletal system has been performed.1 Abrasions or lacerations about the scalp, face, or neck provide mechanistic clues, alerting the examining physician to the potential for underlying spine trauma. The dorsal cervical spine should be palpated carefully to evaluate for focal tenderness, stepoff, or hematoma. Range of motion should be prohibited until the radiographic evaluation of the neck has been completed. All voluntary motion of the arms, hands, fingers, legs, feet, and toes should be observed, graded, and recorded, along with any noted sensory or deep tendon reflex compromise. Incomplete spinal cord lesions are described by a constellation of characteristic neurologic findings determined by the anatomic location of an injury. Examples include Brown-Séquard syndrome, central cord syndrome,2 anterior cord syndrome, and posterior cord syndrome (Table 65-1). A rectal examination is essential (particularly in the neurologically injured patient in order to document the degree of sacral sparing, if any) and should be accompanied by bulbocavernosus reflex testing to assess for spinal shock. Spinal shock is the transient loss of all motor, sensory, and reflex function distal to the level of an acute spinal cord injury. The classification of a neurologic deficit as complete or incomplete cannot be determined until spinal shock has resolved.3
TABLE 65-1 Incomplete Spinal Cord Injury Syndromes
| Syndrome | Characteristics |
|---|---|
Central cord syndrome | The central cord syndrome is the most commonly encountered of all incomplete spinal cord injuries. It is characterized by upper extremity motor weakness with relative sparing of the lower extremities. Expected neurologic recovery is fair to poor. |
Anterior cord syndrome | Anterior cord syndrome results from damage to the interior two thirds of the spinal cord with sparing of the posterior third. There is loss of motor function and pain and temperature sensation. There is preservation of vibration and position sense. Potential for recovery is variable. |
Posterior cord syndrome | Posterior cord syndrome is the least common. Injury to the posterior columns results in loss of vibration and position sense. There may be sparing of crude touch. Potential for functional recovery is fair. |
Brown-Séquard syndrome | Brown-Séquard syndrome is an uncommon injury pattern secondary to injury to half of the spinal cord. This is characterized by ipsilateral motor weakness and loss of proprioception, and contralateral loss of light touch, pain, and temperature sensation. Prognosis for ambulation is excellent in this setting. |
The radiographic evaluation often begins with the ATLS screening series that includes a cross-table lateral view of the cervical spine from the occiput to C7. Care should be taken that the lower part of the cervical spine is completely visualized; superimposition of the shoulders may be overcome with caudally directed manual traction on the patient’s arms. Experience at multiple centers has demonstrated that most missed cervical fractures and subluxations are those present at the lower aspect of the cervical spine.4,5 A swimmer’s view often proves useful for complete visualization of the cervicothoracic junction.6 An open-mouth odontoid view, an anteroposterior view, and a lateral plain radiograph of the entire spine should be obtained if a fracture is found because of the frequent occurrence of noncontiguous spinal injuries. Radiographic findings suggestive of cervical instability are summarized in Table 65-2.
TABLE 65-2 Radiographic Findings Suggestive of Cervical Instability
| Direct Evidence of Instability | Indirect Evidence of Instability |
|---|---|
| Angulation >11° between adjacent segments7 | Increased retropharyngeal soft tissue margin10 |
| AP translation >3.5 mm7 | Avulsion fractures at or near spinal ligament insertions |
| Segmental spinous process widening on lateral view8 | Minimal compression fractures of the anterior vertebral bodies11–14 |
| Facet joint widening3 | Nondisplaced fracture lines through the posterior elements or vertebral body |
| Malalignment of spinous processes on AP view | |
| Rotation of facets on lateral view9 | |
| Lateral tilt of vertebral body on AP view9 |
AP, anteroposterior.
Segmental injuries are common and the presence of injury at one level should prompt a careful search for subtle injuries elsewhere in the spine. CT should be routinely used to provide a more accurate delineation of osseous injuries. Sagittally reconstructed images are helpful in illustrating the sagittal alignment of the spine as well as injuries at the cervicothoracic junction. Such reconstruction is often helpful in demonstrating those fracture lines passing in the plane of the transaxial CT cuts.12 MRI is used further to evaluate the nature and extent of neural and connective soft tissue injury. As such, MRI may be used to identify intracanalicular associated disc herniations, spinal cord contusions, ligamentous disruption, and occult fractures.10,15 Flexion and extension dynamic radiography is frequently used in the awake, neurologically intact patient with isolated neck pain and negative plain radiographs.11 These films are often repeated in patients with persistent neck pain to rule out masked instability secondary to acute muscle spasm.
Soft Tissue Neck Injuries
Isolated soft tissue injury is a common occurrence that has been variably described as whiplash, cervical sprain, cervical strain, acceleration injury, and hyperextension injury.4,16,17 Each of these is nearly always the result of an excessive acceleration force acting violently to extend the neck beyond normal restraints. The overwhelming majority of these injuries occur as the result of MVAs.18,19
Symptoms may include nonfocal neck pain with or without accompanying radicular symptoms, isolated cervical radiculopathy, cervical myelopathy, and various incomplete spinal cord syndromes. Closed head injuries may be associated with these injuries. Intracranial manifestations include chronic headache, concussion, extra-axial/intracranial bleeding, and sympathetic dysfunction. Psychiatric changes, including sleep disturbance, depression, mood changes, or frank personality changes, also may occur.16
The most common radiographic finding is the loss of normal cervical lordosis as seen on a lateral plain radiograph.8 Delayed flexion and extension radiographs are again obtained approximately 1 week after resolution of acute muscle spasm to evaluate for evidence of potential destabilizing soft tissue disruption if an obvious injury is not present.3,11 Bone scan has a limited role in screening for occult fractures in selected patients with atypical chronic pain.8 If the bone scan is positive, a CT may then be performed for further evaluation. Early intervention and treatment are based on the presenting injury subtype, including its pathomechanics and severity, and the overall medical status of the patient. In the setting of a whiplash-type injury, initial use of a soft collar will improve comfort in many patients, although use should be limited to a 2- to 4-week period to minimize dependence, muscle atrophy, and decreased neck range of motion.20 Isometric exercises and gentle, supervised range of motion should be initiated as soon as symptoms permit (or within 2 weeks of injury). The regimen should be performed several times a day and should include neck flexion and extension, rotation, and lateral flexion. Enlisting the assistance of a physical therapist may be beneficial, particularly in the early phases of recovery.
Transient Quadriplegia
A neurapraxia-type injury to the cervical spinal cord resulting in transient quadriplegia is most commonly seen in athletes participating in contact sports. The incidence among collegiate football players is 7.3 per 10,000 athletes. Plain radiographs are negative in this setting. The mechanism of injury is most often axial compression combined with hyperflexion or hyperextension. Sensory and motor neurologic deficits are bilateral and usually persist from several minutes to 48 hours after trauma. There is an association with developmental cervical stenosis, although effective guidelines for identification of predisposed athletes have been difficult to establish. Efforts to establish sensitive and specific screening methods to reliably identify at-risk athletes are under way.17,21
Injuries to the Occipitocervical Articulation
The occipital condyles are paired, semilunar-shaped projections from the inferior aspect of the occiput that articulate with the atlantal lateral masses. This articulation bears little intrinsic osseous stability, depending instead on the external and internal craniocervical ligaments for constraint. The internal craniocervical ligaments (tectorial membrane, cruciate ligament, and paired alar and apical ligaments) confer most of the intrinsic occipitoatlantal stability.22 Injury to the craniocervical junction commonly occurs through three primary forces: distraction, compression, and rotation.23 Injuries may be mild and stable or life threatening (with complete osteoligamentous disruption).24
Occipital Condyle Fractures
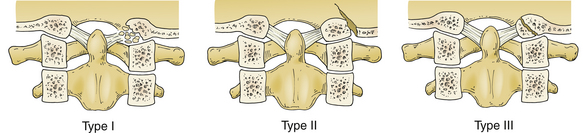
Occipital condyle fractures are most often identified incidentally on head CT in the unconscious patient, although awake patients with complaints of deep suboccipital pain or occipital headache should be suspected of having sustained an injury to the occipitocervical junction.25,26 The incidence is not high, with one trauma center estimating an incidence of 1.7/1000 per year.27 The neurologic examination in survivors is often negative, although mild cord injury and lower cranial nerve injury have been reported. Classification of occipital condyle fractures is based on CT morphology25,28 (Fig. 65-1). A type I fracture is a comminuted fracture of the condyle resulting from impaction of the condyle by the lateral mass of C1. The mechanism is often a direct blow to the head. A type II injury is characterized by the presence of a related basilar skull fracture. Type III injuries are avulsion fractures occurring at the attachment site of the alar ligaments. They may be bilateral in up to 50% of cases and, in this circumstance, are associated with an atlanto-occipital dislocation. Treatment of stable type I and II injuries is cervical immobilization in a hard collar, cervicothoracic brace, or halo vest for 8 to 10 weeks. Type II fractures demonstrating separation of the occipital condyle from the occiput may have inadequate lateral column support, thus requiring 8 to 12 weeks of halo-vest immobilization. Instability is commonly noted in type III injuries and is demonstrated by occipitoatlantal anteroposterior displacement, longitudinal diastasis, or joint incongruity. Injuries identified as unstable are best managed with a dorsal occipitocervical arthrodesis.23,29–32 Recently, Maserati et al. performed a retrospective review of 24,745 consecutive trauma patients over a 6-year period and identified 100 patients with 106 occipital cervical fractures (0.4% incidence). They concluded that immobilization in a rigid cervical collar with delayed radiographic follow-up was adequate as long as there was no evidence of occipitocervical misalignment, which would necessitate the need for occipitocervical fusion or halo fixation.33
Occipitocervical Dislocation/Dissociation
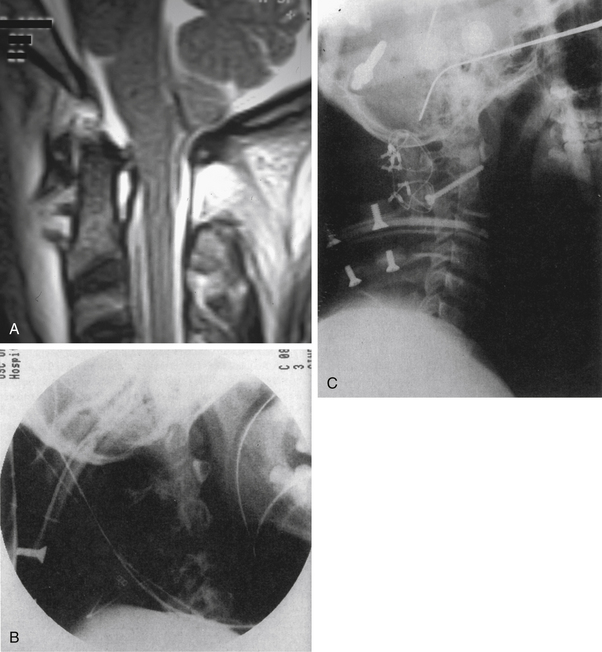
Until recently, few cases of patients surviving this entity had been reported.29–31,34–36 Most reports of survival from occipitocervical dislocation/dissociation have been in children.37 Occipitocervical dislocation or dissociation often results from high-energy trauma, is highly unstable, and is frequently fatal (Fig. 65-2). High-resolution CT (with or without MRI) is often required to evaluate these injuries because they may be difficult to appreciate on plain radiographs unless significant displacement is present (Fig. 65-3A). MRI is often required to evaluate these injuries. Occipitocervical instability (subluxation and dislocation) is classified according to the direction of displacement of the occiput.25,33,38 Type I injuries are ventral subluxations of the occipital condyle relative to the atlantal lateral masses. These represent the most commonly observed injury pattern. Type II injuries are vertical displacements of the occipital condyles greater than 2 mm beyond normal. C1-2 distraction injuries are included in this category. Type III injuries are dorsal occipital dislocations and are exceedingly rare. In evaluating these injuries, more than 2 mm of subluxation at the atlanto-occipital articulation indicates a functional loss of integrity of the major occipitocervical stabilizers such as the alar ligaments and the tectorial membrane.28,39 The treatment of occipitocervical instability is through closed or open reduction and surgical stabilization.40 Traction is to be avoided in these injuries (Figs. 65-3B and C). There has been a recent trend toward performing occiput-to-C1 fusion (C0-1 fusion) using transarticular screw fixation, instead of occipitocervical fusion, in order to maintain mobility across the C1-2 junction.35,37

FIGURE 65-2 Lateral plain radiograph revealing longitudinal diastasis of the occipital-C1 articulation.
Injuries to the First Cervical Vertebra
Traumatic Transverse Atlantal Ligament Avulsion
Insufficiency or avulsion of the transverse atlantal ligament (TALA) may occur after a violent flexion force to the upper cervical spine. Associated head injuries are common, and although survival after acute traumatic rupture had previously been thought unusual, it is now being reported with increasing frequency.41,42 Findings range from normal to transient quadriparesis. Permanent quadriparesis is rare given the fatal sequelae that typically follow complete injury at this leve1.42–44 Associated clinical signs include cardiac and respiratory changes secondary to brainstem compromise, or dizziness, syncope, and/or blurred vision as a result of vertebral artery disruption. Symptoms may be exacerbated by neck flexion. A lateral plain radiograph often demonstrates abnormal translation (>5 mm) at the atlantodens interval.45,46 Conservative treatment strategies have generally failed to provide satisfactory results, and the treatment of choice in most patients is a C1-2 arthrodesis. Acute disruption of the transverse ligament may also be noted in association with a Jefferson-type burst fracture of C1.47–51 Treatment in this circumstance should consist of cervical immobilization for 10 to 12 weeks, awaiting union of the C1 arch. Persistent instability after completion of cervical immobilization may then be addressed with a C1-2 fusion.48,52 An atlas nonunion has been reported to result in basilar invagination with significant splaying of the C1 lateral masses.53
Traumatic Rotatory Subluxation
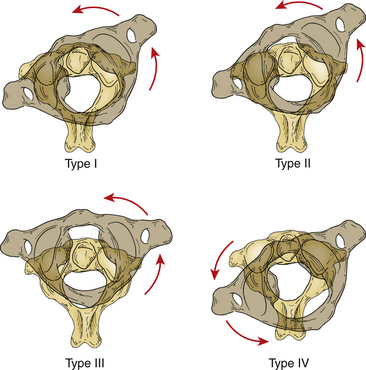
Acute trauma is an unusual cause of acute C1-2 rotatory subluxation. The clinical presentation of C1-2 rotatory subluxation is the complaint of neck pain with findings of torticollis, and it is more commonly seen in children than adults. Four types of fixed C1-2 rotatory injuries have been described54 (Figs. 65-4 and 65-5). Type I injuries involve fixed rotational changes without associated subluxation. In the type II pattern there is 3 to 5 mm of displacement of C1 on C2 (with one lateral mass acting as a pivot while the other rotates ventrally). Type III injuries have more than 5 mm of forward displacement of both lateral masses. Type II and III injuries are both associated with transverse ligament incompetence, and neurologic involvement is common. Associated C2 fractures (type II and III odontoid fractures) have been reported with severe rotatory atlantoaxial subluxation.55,56 Conservative treatment consists of halo or Gardner-Wells traction-reduction, followed by external immobilization for 2 to 3 months. Delayed instability is managed with a dorsal stabilization procedure. Severe rotations with associated cervical fractures (i.e., C2) need to be fixed with intraoperative fusion.55 Fixed or irreducible deformities as well as delayed presentation of this condition are again best managed with surgical stabilization.
Fractures of the First Cervical Vertebra
Fractures of C1 occur either as an isolated injury or often in combination with a fracture to the C2 vertebra. The most common associated cervical spine injuries are a type II odontoid fracture and spondylolisthetic fracture of C2.48,57,58 Fractures of C1, seen in up to 10% of all spine injuries, are encountered with relative frequency.59,60 Neurologic injury is unusual.46
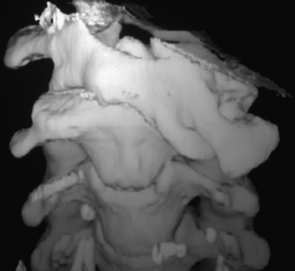
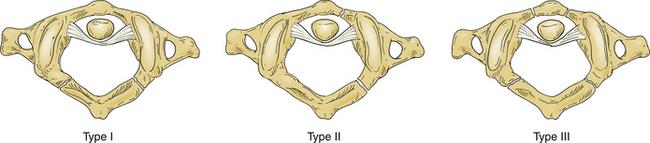
Fractures of C1 are classified generally into three categories. This classification scheme has proven useful in determining treatment options, expected clinical course, and prognosis61 (Fig. 65-6). Type I fractures are limited to involvement of the dorsal arch, are often bilateral, and typically occur at the junction of the lateral masses and dorsal arch. This is the most common pattern of C1 fracture and likely occurs secondary to hyperextension in conjunction with an axial load. A type II atlas fracture is a unilateral lateral mass injury that occurs as the result of an asymmetrically applied axial load. Intra-articular extension is not common but is reported.46,62 A type III (or Jefferson) fracture is a burst-type fracture that involves three or more fractures through the ventral and dorsal aspects of the C1 ring. The mechanism of this second-most-common pattern is that of a pure axially applied load.63,64
Plain radiographs are useful in the evaluation of these injuries and often demonstrate widening of the retropharyngeal soft tissue shadow from C1 to C3 (although these changes may take 6 or more hours to develop).65,66 The open-mouth odontoid view shows lateral displacement of the lateral masses in a Jefferson-type fracture and may appear normal with the more common type I dorsal arch fracture. If total combined lateral displacement of the C1 lateral masses over C2 is greater than 6.9 mm,65,67 the transverse ligament has been disrupted, resulting in an unstable injury.48,59,68 Type II fractures appear radiographically as unilateral displacement of the affected lateral mass on an open-mouth odontoid radiograph. Improvements in technique and image quality have made CT in the plane of the C1 ring helpful in fully defining these injuries. The most important factor governing treatment and outcome is the simultaneous occurrence of other injuries.48,57,69 Treatment of isolated C1 fractures has traditionally been nonoperative, although some European centers have reported the successful surgical reduction and stabilization of markedly displaced Jefferson burst fractures. Results with nonoperative treatment have been good,49 although mild neck pain is a chronic sequela in up to 80% of these patients.59 There has been no reported correlation between fracture union/nonunion and functional outcome.51
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree