Chapter 22 Traumatic Skull and Facial Fractures
• Linear skull fractures do not require stabilization or treatment when the scalp is closed. Depressed skull fractures may need exploration depending on the extent of the injury to the underlying brain, frontal sinus, or facial bones. Closed depressed fractures are usually repaired for cosmetic reasons. Compound depressed skull fractures with brain involvement are often neurosurgical emergencies. It becomes an emergency to treat the underlying brain injury, perform a watertight closure of the dura, and débride the devitalized scalp.
• Growing skull fractures, although rare, occur in children under 2 to 3 years of age and require surgical repair. If there is a tear in the dura accompanying a skull fracture after trauma, the pressure of the brain pulsations in a growing brain may enlarge the fracture and dural opening. The brain can herniate through this skull defect, causing a pulsatile mass under the scalp.
• Basilar skull fractures may present with periorbital ecchymoses, hemotympanum, or ecchymosis over the mastoid. The management of these fractures is usually conservative unless a cerebrospinal fluid (CSF) leak is present. Many traumatic CSF leaks will spontaneously resolve in a week. Those that do not may be managed by CSF drainage, or in some cases surgical repair to avoid infection, once the location of the leak is identified.
• Frontal sinus fractures can be diagnosed on computed tomography (CT) and are managed differently depending on whether the frontal or posterior wall is disrupted. Orbital fractures are managed based on the extent of the injury to the globe, optic nerve, and orbital contents. Patients with a fluctuating or worsening visual acuity will require decompression of their optic nerve and relief of globe pressure. There are two indications for surgery of orbital “blow-out” fractures: (1) muscle or ligament entrapment with diplopia or (2) enophthalmus (backward dislocation of the globe) caused by prolapse of the orbital contents through the fracture. Le Fort fractures are often injuries to the entire midface region. Their surgical management depends on the extent and stability of the maxillary fracture.
Skull Fractures
The second factor is the ratio of the impact force to the impact area. If the impact, even one of high energy, is dispersed over a large area, as in a blunt head injury to an individual wearing a motorcycle helmet, it often produces no skull fracture, even though the brain may be severely injured. Parenthetically, it should be noted that some helmets, by the efficiency of their very force-transferring protection, have created basal skull fractures by transferred energy absorbed from protection of the vault and face and then transmitted through the mandible via the chin strap to the skull base. However, if the impact, even one of low energy, is concentrated in a small area, such as from a hammer blow, it often produces a small depressed fracture with multiple linear skull fractures radiating from the site of impact.
Linear Skull Fractures
Management
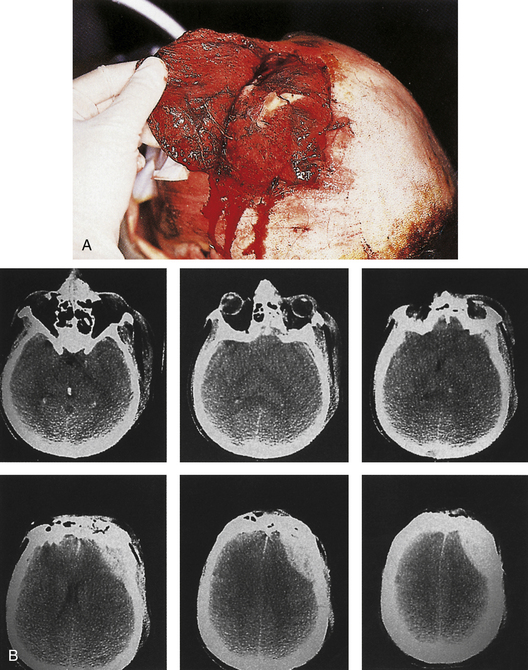
Linear skull fractures require no stabilization or exploration when the scalp is closed, and when there is no evidence of epidural hematoma or underlying dural or cortical injury. Even when a scalp laceration is present, very seldom is surgical exploration with bone removal necessary. Exceptions would include a machete injury to the skull producing a linear skull fracture with underlying dural laceration and brain damage. The skull fracture does, however, show that significant head trauma has occurred, and a careful assessment of the brain, facial structures, and cervical spine is required. Open linear fractures are débride of foreign material, devitalized soft tissue, and bone fragments; preferably, the damaged soft tissue at the edges of the laceration is excised to healthy, noncontused bleeding tissue (if the tissue excision can be tolerated and will permit primary closure) and the laceration is closed after thorough cleansing. If there is insufficient vascularized soft tissue present to permit excision of the contused devitalized tissue, a rotation flap and skin graft to the donor area may have to be considered (Fig. 22.1).
Growing Skull Fractures in Children
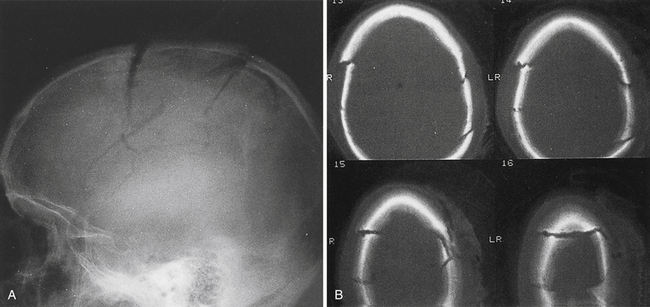
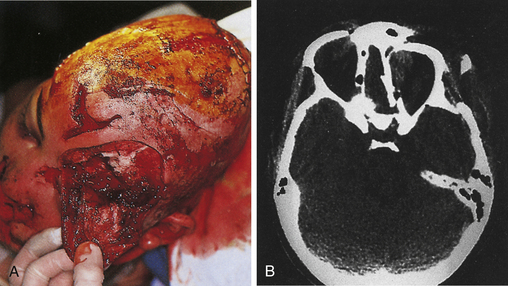
A rare complication after linear skull fracture in young children (usually younger than 2 or 3 years) is a “growing” skull defect at the fracture site. In these cases, the dura is torn under the linear skull fracture. The pathogenesis is thought to be an expanding pouch of arachnoid passing through the torn dura and skull fracture, acting as a one-way valve that traps cerebrospinal fluid (CSF) and causes progressive pressure erosion of the fractured edges to enlarge the fracture. Alternatively, the growth of the brain, which produces pulsating, spreading tensile pressure forces on the edges of an unrepaired dural laceration, may also cause a skull defect to enlarge. These vectors of force by the brain may sometimes cause herniation through the skull defect, causing a new neurological deficit (Fig. 22.2). These lesions are surgically repaired with closure of the dura or with a dural patch and replacement or repair of the bone defect. Some surgeons routinely take a skull film at 1 year after linear skull fracture treated nonoperatively to detect such growing skull fractures. For this reason it is worthwhile for the primary care doctor to examine the scalp and skull of any child with a known skull fracture under the age of 2 or 3.
Comminuted Fractures
Management
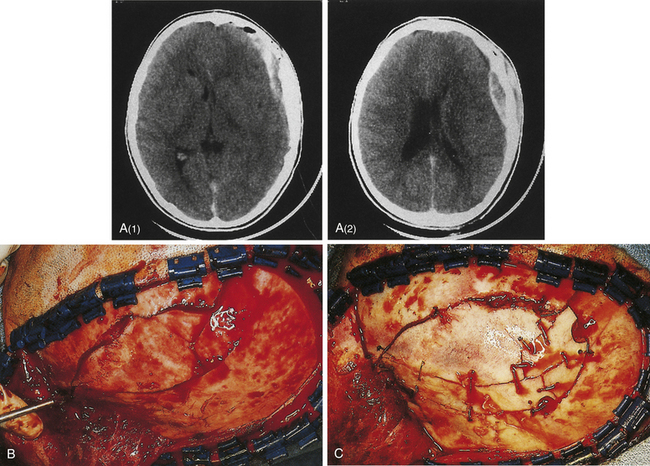
If the skin is closed, and no depression of bone fragments greater than the thickness of the skull is demonstrated on CT, management is as that for linear skull fractures. However, in many of these cases, surgery is performed for the underlying intracranial injury, such as an epidural hematoma (Fig. 22.3). After the intracranial injury has been corrected, the bone fragments are primarily replaced as a bone cranioplasty after cleaning.
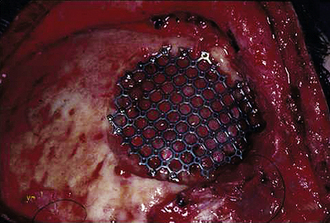
Missing bone can be replaced with a titanium mesh screen. If the skin is open, and free bone fragments are present, cleansing or débridement of the contaminated fragments is performed, before dural and scalp closure (Fig. 22.4). Bone too contaminated may be discarded, and a titanium screen is then used to span the bone defect (Fig. 22.5).
Depressed Skull Fractures
Management
Combined therapy of depressed fractures of the cranial vault extending to involve the frontal sinus or facial bones is covered in the sections on facial fractures. When a depressed skull fracture on the convexity also includes facial fractures, the intracranial injury is typically repaired first with removal of intracerebral hematoma and repair of dural laceration if present (Figs. 22.6 and 22.7).
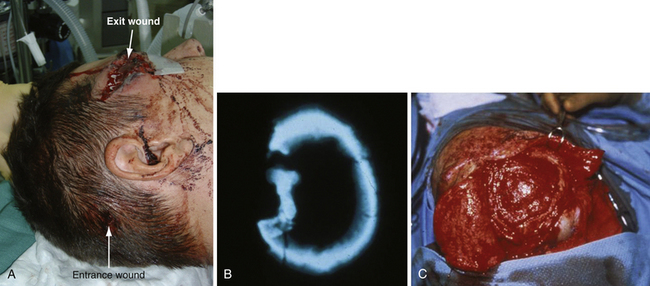
A compound depressed fracture is a neurosurgical emergency because of the risk of bacterial infection of the cranial cavity. The initial surgery is performed within 24 hours and usually within the first 12 hours. The major objectives are removal of contaminated bone fragment and foreign material; débridement of devitalized scalp, dura, and brain; and provision of a watertight closure of the dura. Often, foreign material or hair wedged between bone fragments cannot be seen through the overlying scalp incision, so simple irrigation and closure may be inadequate for débridement of foreign material. Dural closure is essential to prevent CSF leaks from the wound and brain herniation into the fracture area. Dural closure is essential to prevent CSF leaks from the wound and brain herniation into the fracture area. Dural closure also presents intracranial spread of infection from a scalp wound. Reconstruction of the calvarium is performed during the initial surgery if considered safe: otherwise a cranial defect is left and the cosmetic repair is performed later. The major reasons to consider deferred calvarial reconstruction are to shorten additional anesthesia and blood loss by major head injury or multitrauma, especially with hemorrhage; gross contamination of wounds where the bone fragments cannot be adequately cleaned; and a delay of more than 24 hours for the initial surgery.
The scalp laceration associated with a compound depressed skull fracture is usually stellate and may contain areas of contused/devitalized tissue. These areas require débridement to normal vascularized scalp to allow prompt healing and prevent breakdown of the partially viable scalp covering the fracture site (see Fig. 22.1). Scalp breakdown can many times be treated locally but occasionally will require early flap coverage. If early flap coverage is not successful, the replaced cranial bone may require débridement of any dead or nonviable necrotic bone or portion of the skin flap; a subsequent flap rotation and delayed cranioplasty will be required in stages.
Basilar Skull Fractures
Fractures of the base of the skull occur in 3.5% to 24% of head-injured patients. This wide variation results from differences in study populations and the difficulty in obtaining radiographic verification of the fractures. Linear fractures in the skull base carry a risk of meningitis, whereas this risk is extremely low in fractures of the convexity unless the scalp, bone, and dura are all violated. The dura is easily torn in a basal skull fracture; this places the subarachnoid space in direct contact with the paranasal sinuses or middle ear structures, providing a pathway for infection. For example, a persistent fistula allows a continuous CSF leak, and bacterial colonization of the meninges will eventually develop.
Petrous bone fractures can either be either longitudinal or transverse, relative to the long axis of the petrous pyramid. Longitudinal fractures are more common and usually involve the tympanic membrane or external ear canal, thereby producing otorrhea. Transverse fractures result from higher-energy impacts and can damage middle ear ossicles or the facial nerve. These fractures occur with or in continuity with linear, comminuted, or depressed skull fractures and not infrequently are large linear extensions of vault fractures, crossing the base of the anterior and middle cranial fossae (Fig. 22.8).
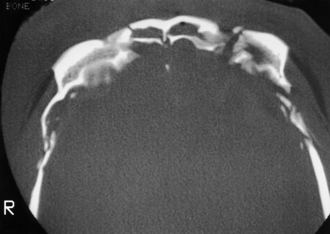
FIGURE 22.8 Type III frontobasilar fracture involves both the lateral and the central segments of the anterior skull.
Diagnosis
Clinical signs of basal skull fractures include bilateral periorbital ecchymoses (spectacle hematoma) (Fig. 22.9), anosmia, or CSF rhinorrhea for anterior skull base fractures, as well as hemotympanum, blood in the external auditory canal, seventh or eighth cranial nerve palsies, ecchymoses over the mastoids (Battle’s sign), or CSF otorrhea for temporal bone fractures (Fig. 22.10). Frequently, the CSF leak is first detected several days or weeks after the trauma. This delay often occurs because the CSF leak was hidden in bloody nasal discharge from facial fractures, or less frequently, it is the result of delayed development of hydrocephalus with rupture of the arachnoid at the fracture site. A larger clear ring surrounding a central blood-tinged clot when a few drops of bloody discharge are placed on a paper towel indicates that CSF is probably mixed with the blood. This sign (the “double ring”) can also be noted on the patient’s pillow during rounds.
Basal skull fracture with CSF rhinorrhea is common after head injury and has an estimated incidence in the United States of 150,000 cases per year. A clear, watery nasal discharge containing glucose indicates CSF rhinorrhea. An intermittent CSF leak from the paranasal sinuses can often be demonstrated by having the patient sit on the edge of the bed with the head close to the knees for 2 minutes and watching for clear fluid to drip from the nose. CSF mixed with blood may form a halo on a piece of gauze it touches. Testing for beta-2 transferrin presence in the fluid confirms the protein found almost uniquely in CSF.
Maxillofacial Injuries
Assessment
Facial sensation is noted in the supraorbital, supratrochlear, infratrochlear, infraorbital, and mental nerve regions of the trigeminal nerve distribution for both pinprick and light touch sensation. Diminished sensation in the distribution of a specific sensory nerve indicates injury from transaction, impact, or continued compression of the nerve as the result of a fracture. The facial nerve is tested by comparing facial expression bilaterally. Extraocular movements and pupil response are compared, evaluating symmetry, pupil size, and the speed of pupil reaction bilaterally to both direct and consensual responses to light.
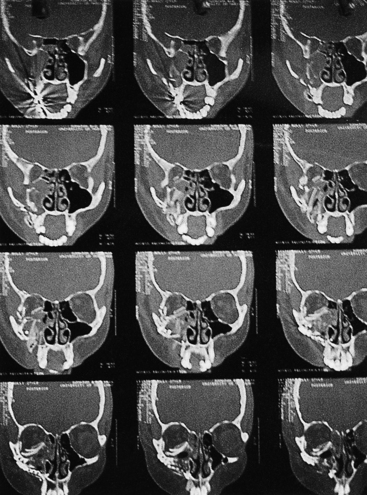
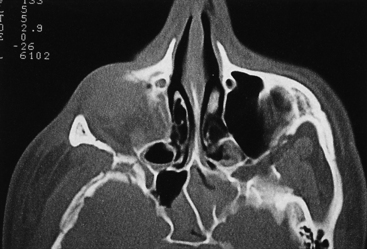
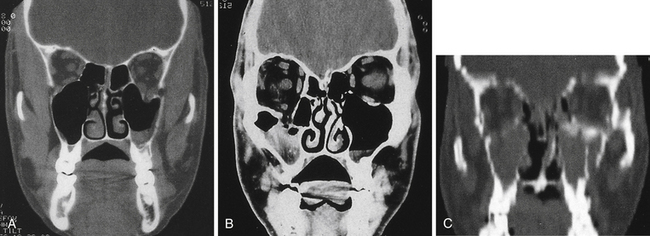
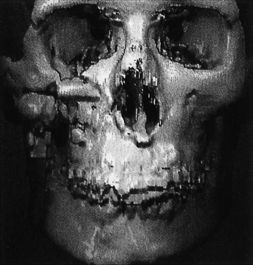
The early management of maxillofacial injuries is based entirely on a good clinical examination and facial CT scans (Fig. 22.11). Soft tissue windows are necessary on the CT scan to evaluate the brain and orbital soft tissue fully. Axial (Fig. 22.12) and coronal CT bone windows (direct or reformatted) are crucial to reveal details of fractures of the upper face and orbit. Coronal sections (Fig. 22.13) begin with the nasal pyramid and continue posteriorly through the orbital apex. Axial scans begin at the superior aspect of the skull and progress through the brain with standard axial brain imaging. The size and spacing of the cuts at the level of the frontal sinus are reduced to 5 mm or less to obtain the required detail. When a mandible fracture is suspected, the axial CT scanning is continued through the entire mandible and temporomandibular joints, visualizing both the horizontal and vertical portions of the mandible and the temporomandibular joints. Although three-dimensional reconstruction with shading (Fig. 22.14) adds spatial information, it does not provide the detail of two-dimensional axial and coronal images. In some cases, special reconstructions, as one performed in the longitudinal axis of the optic nerve in orbital injury, provide additional information.
Associated Conditions
Profuse Hemorrhage
Cutaneous bleeding that accompanies facial lacerations is usually controlled with digital pressure, which allows precise identification of the bleeding vessel for control or ligature. Blind probing in facial tissue or unselective cautery or ligature placement can damage branches of the facial nerve and should be avoided.
Coma and Brain Injury
Coma or unconsciousness should not prevent or delay the treatment of facial fractures; many patients with facial fractures are in a coma for several weeks before waking up. In patients with maxillofacial fractures, neurological deficits from frontal lobe symptoms may be subtle or absent despite contusions imaged on brain CT scans. Confusion, somnolence, personality change, irritability, and difficulty in thinking are some of the milder symptoms of frontal brain contusion. In patients with Glasgow Coma Scale scores of 14 or less, and especially when traumatic brain abnormality is visualized on CT scan, an intracranial pressure monitoring device may be employed in those patients who require anesthesia. A fiberoptic intracranial pressure (ICP) monitor or intracranial ventricular pressure monitor is used in the operating room during the facial repair, thus allowing optimal modification of the anesthesia and if necessary CSF drainage in patients in whom multiple injuries require early surgical intervention.
Facial Fracture Classification by Anatomical Region
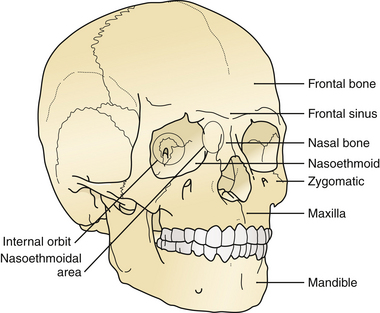
The treatment of maxillofacial fractures is organized by anatomical region (Fig. 22.15). The frontal bone region includes the frontal bone, the supraorbital rims bilaterally, and the frontal sinus (Fig. 22.16). The upper midface region includes the zygoma laterally, the internal orbital area, and the nasoethmoidal area centrally. The lower midface consists of the maxillary alveolus. The mandible consists of the horizontal portion containing the teeth and the vertical portion that includes the angle, ramus, coronoid, and condylar process. The pattern and displacement of the fractures in each anatomical region determine treatment. Orbital fractures are classified by their position on the orbital rim and by their involvement of the internal section of the orbit. Orbital rim fractures are divided into supraorbital, the nasoethmoid medically, and the zygomatic region inferolaterally (Fig. 22.17). The section of the internal orbit consists of the orbital floor, the lateral orbit, and the medial (ethmoidal) orbit. Maxillary fractures are classified according to the patterns of Le Fort, based on the fracture’s location in the maxilla where it is separated from intact upper facial units.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree