20 | Traumatic Spondyloptosis of the Cervical Spine |
 | Case Presentation |
History and Physical Examination
A 29-year-old man was riding a bicycle down a steep hill when a large dog crossed his path. With sudden braking, his bicycle tumbled end-over-end, and he landed on the top of his head. He complained of pain at the low-cervical area and had immediate profound weakness of his right leg and left arm. He was immobilized in a cervical collar and on a spine board and flown to a level I trauma center for further evaluation.
Physical examination upon arrival at the hospital revealed grade 3 of 5 strength of the left triceps and intrinsic hand muscles, and grade 3 of 5 right iliopsoas, anterior tibialis, and gastrocnemius-soleus muscles. Other muscle groups were noted to be grade 5/5 strength. He also had intact sensation in all dermatomal areas to pinprick, and normal rectal tone.
Radiological Findings
A lateral cervical spine radiograph was taken but was inadequate to visualize the lower cervical spine (Fig. 20–1A). Swimmer’s view was suggestive of a lower cervical spine injury (Fig. 20–1B), but details of the anatomy were difficult to visualize. Computed tomography (CT) of the cervical spine revealed complete anterior dislocation of the C7 vertebral body on T1 and a comminuted C6 and C7 lamina fracture (Fig. 20–2).
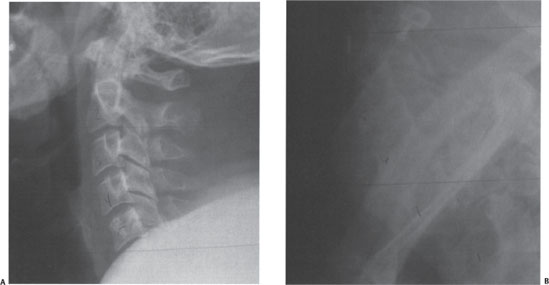
Figure 20–1 (A) Lateral radiograph of the patient shows up to C5. This is an inadequate lateral view to evaluate a trauma patient. (B) Swimmer’s view of the same patient shows a possible anterior dislocation of the C7 body on T1

Figure 20–2 Sagittal computed tomographic reconstruction view confirms complete anterior dislocation of the C7 body on T1.
Diagnosis
Based on the radiographs and physical examination, he was diagnosed with traumatic spondyloptosis of the cervical spine with an incomplete spinal cord injury. Attempted closed reduction with cervical traction in the emergency room was unsuccessful. A magnetic resonance imaging (MRI) scan was then obtained and revealed disk material extruded behind the body of C7 (Fig. 20–3). The patient was placed in halo vest immobilization before being taken to the operating room for decompression, open reduction, and instrumented fixation.
 | Background |
Spondylolisthesis of the cervical spine, especially of a degenerative origin, is a well-described entity encountered in clinical practice. Although spondyloptosis of the lumbar spine has been commonly reported, cervical spondyloptosis is rare. Spondyloptosis of the cervical spine can be of congenital,1–4 neoplastic,5,6 or traumatic7–12 origin.
Numerous classifications of cervical spine injuries have been formulated, but the classification system proposed by Allen et al appears to be the most comprehensive.11 This is a mechanistic classification system describing closed, indirect fractures and dislocations of the lower cervical spine. In a review of 165 lower cervical spine injuries, Allen identified six common, but distinct, patterns of injury, or phylogenies. Each phylogeny is then subdivided into progressive stages based on the degree of osseous and ligamentous injury. The three most common injury patterns are compressive flexion, compressive extension, and distractive flexion. The compressive extension stage 5 (CES5) and the distractive flexion stage 4 (DFS4) injuries represent complete vertebral body width displacement anteriorly, or spondyloptosis. The other less common categories include distractive extension, lateral flexion, and vertical compression.
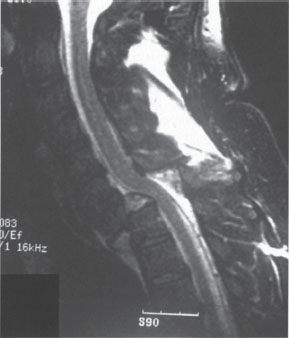
Figure 20–3 Magnetic resonance imaging shows extruded disk material behind the body of C7. Attempted closed reduction without anterior decompression of this injury may further drive the disk material posteriorly into the spinal cord.
Spondyloptosis can occur with and without associated fractures of the posterior vertebral arch. With spondyloptotic injuries, spinal cord injury can occur when the posterior vertebral arch remains intact and may result in the cord being pinched between the vertebral arch of one vertebra and posterior aspect of the body of the subjacent vertebra. Spondyloptosis of the cervical spine is usually associated with a complete or total spinal cord injury.11 In patients with spondyloptotic injuries, complete spinal cord injury appears less common if there is disruption of the vertebral arch.7,9–12 The posterior elements of the fractured vertebra do not displace and, theoretically, cannot impinge on the cord as the vertebral body translates anteriorly. Although it seems logical that fractures of the vertebral arch would have a cord-sparing effect even with smaller degrees of vertebral body displacement, the data from Allen et al do not support this theory.11 Sixty percent of the DFS3 injuries (bilateral facet dislocation with ~50% anterior vertebral body displacement) with bilaminar fracture versus 58.3% DFS3s without bilaminar fracture sustained a complete spinal cord injury. Fractures of the vertebral arch did not appear to be protective against complete spinal cord injury in this subset of patients.
Fractures of the vertebral arch may play a more important role in protecting the spinal cord from injury in spondyloptosis patients. Of the seven patients sustaining a DFS4 injury (spondyloptosis), all but one sustained a complete spinal cord injury. The sole DFS4 patient without any neurological injury did have bilaminar fractures of the vertebral arch. All three patients with CES5 injuries (spondyloptosis) had arch failure consisting of fractures through the articular processes at multiple vertebral levels. None of the CES5 patients incurred a complete spinal cord injury. One patient had radicular symptoms, one had a partial cord injury, and one had a central cord syndrome. Regardless of the mechanism of injury, distraction flexion versus compression extension, the integrity of the vertebral arch may play an important role in determining the incidence and severity of spinal cord injury.
Other than the four patients reported by Allen et al, there are only a few additional cases of traumatic cervical spondyloptosis without complete spinal cord injury reported in the literature.7,9–12 All of these patients had fractures of the posterior elements with disruption of the vertebral arch. None of these patients had a complete spinal cord injury.
 | Authors’ Preferred Method of Surgical Management |
The initial management of any cervical spine injury is temporary stabilization. Any patient with a suspected spine injury should be stabilized in a cervical collar on a spine board. A thorough radiographic evaluation should include a CT scan of the C-spine to include the cervicothoracic junction. Whether MRI should be part of the initial evaluation is controversial. In our institution, an MRI scan is only obtained if the patient has a neurological deficit without CT evidence of a C-spine injury, has had an unsuccessful attempt at closed reduction, or is scheduled for a surgical reduction of the dislocated spine.
Traumatic spondyloptosis is an extremely unstable injury with disruption of the total spinal column. The primary surgical goals are to realign the spine without a new neurological injury, and maintain spinal stability to obtain early functional recovery. If the patient is awake and cooperative, a closed reduction with graduated weight can be performed. If closed reduction is successful, the patient should be immobilized in a halo vest prior to surgical stabilization. In a more common situation where the reduction is unsuccessful, an emergent MRI scan should be obtained to visualize any disk or bone fragments in the spinal canal prior to operative decompression and reduction.
Both anterior and posterior instrumented fixation is recommended in this highly unstable fracture. The anterior approach is performed using the standard Smith-Peterson technique, and decompression of the neural elements is accomplished by diskectomy, partial corpectomy, or full corpectomy of the displaced vertebral body. In most cases of traumatic spondyloptosis, a full corpectomy of the displaced body will be necessary for safe realignment of the spine. We recommend positioning the patient with Gardner-Wells tongs, with 5 lb of traction to stabilize the head. After the anterior decompression, a lateral x-ray can be taken to evaluate if the spine has spontaneously reduced. If not, weights can be increased in a graduated manner with serial intraoperative x-rays to attempt reduction. If reduction is not achieved after several tries, then we recommend committing to an anterior-posterior-anterior procedure. Therefore, if the spinal columns are not fully reduced after an anterior decompression with traction, the wound is closed and the corpectomy trough is left empty. The patient is then turned prone for a posteriorly directed reduction of the spine and instrumented fixation. In the third stage of the procedure, the patient is again placed in the supine position for insertion of the structural graft and anterior plate fixation. We prefer this anterior-posterior-anterior procedure for any significantly displaced cervical spinal dislocations, especially in patients with incomplete neurological injury.
Posteriorly directed reduction can be difficult in cases where the posterior elements are fractured. Often, the posterior instrumentation will have to incorporate spinal segments in addition to the injured levels to achieve solid fixation. With the presence of posterior arch fractures, placement of lateral mass screws and “indirect” reduction to precontoured rods may be necessary. In this case, prebending the rods to anatomical lordosis and locking the rods into the screw heads can achieve satisfactory alignment and stabilization. In some cases, the dislocated facets may have to be burred away to achieve satisfactory alignment.
In our patient, the attempted closed reduction failed, and the MRI revealed a large disk fragment behind the body of C7 (Fig. 20–3). He was taken emergently to the operating room for an open reduction and combined anterior-posterior instrumented fixation. During the anterior approach, it was noted that he also had a significant disruption of the disk and anterior longitudinal ligament (ALL) at the C6-7 level as well. A diskectomy was performed at C6-7, and a full corpectomy was performed at the C7 level. The patient was then turned prone for reduction, posterior instrumentation, and arthrodesis. Finally, the patient was repositioned supine and graft placement with anterior plate fixation was performed (Fig. 20–4).
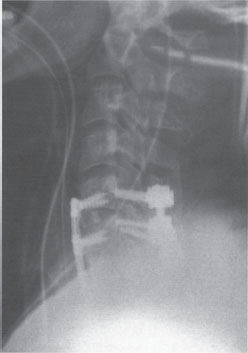
Figure 20–4 The postoperative radiograph showing anterior decompression and strut grafting as well as anteroposterior stabilization using an anterior plate and posterior rod-lateral mass screw construct.



