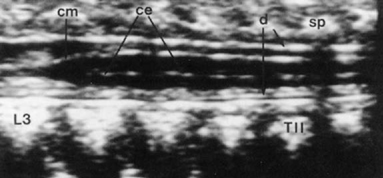
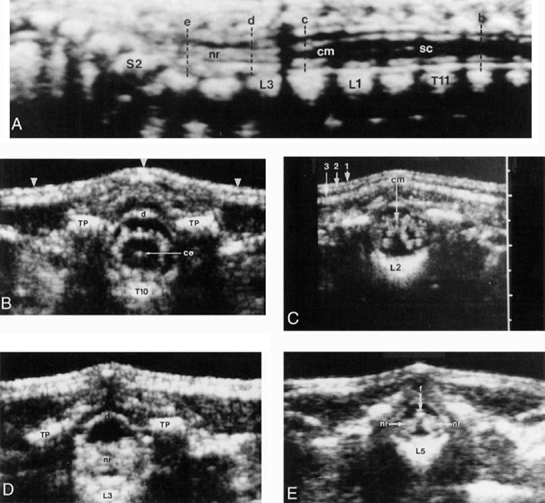
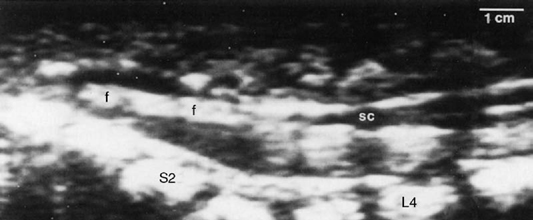
6 Ultrasonographic Evaluation of Tethered Cord Syndrome Marvin D. Nelson Jr. Real-time ultrasonography is an imaging tool that is useful for evaluating neonates with suspected congenital spinal cord malformations and patients with repaired lipomyelomeningocele or myelomeningocele at risk for spinal cord tethering. Ultrasonography provides inexpensive high-resolution images, usually without sedation. The ultrasonic image is produced by transmitting a high-frequency sound beam into the tissue of interest, then “listening” for the reflections (echoes) produced at the interfaces of tissues of different densities. The echoes are usually depicted as shades of white on a black background. A large difference in density between the two tissues produces a stronger returning echo and a brighter area on the image. Interfaces with bone or air reflect 99% of the sound beam, causing a very bright echo at the interface, with no through transmission distal to that point. By using multiple sound sources fired in sequence, a computer can time the echoes and separate them in a rapid series of images, similar to a motion picture, producing a “realtime” image depicting the movement of structures within the field of view of the transducer. At birth, the posterior vertebral arch has yet to ossify in the midline, allowing a sonographic “window” to image the spinal canal and contents in great detail. However, within 8 weeks, the posterior arch is no longer sonolucent. Thereafter, attempts to image the spinal cord are limited to angling the ultrasound beam between spinous processes. Patients with spina bifida have permanent “windows” due to their posterior vertebral arch defects. This allows ultrasonic imaging at the involved levels at any age. The patient is examined prone with the head in a neutral position. Using a 3, 5, or 7 mHz linear array transducer, both longitudinal and transverse static images are made of the spine from the foramen magnum to the coccyx. The spinal cord is then observed for evidence of normal pulsatile movement at all levels and documented by saving the cine clip. Within the spinal canal, the dura (thecal sac) appears as a thin echogenic line around the spinal cord (Figs. 6.1, 6.2). The cerebrospinal fluid (CSF) produces no echoes (anechoic) and appears black on the images. The spinal cord has well-defined echogenic margins because the sound beam is partially reflected off the surface of the cord (Figs. 6.1, 6.2A). The spinal cord parenchyma appears hypoechoic (few echoes, relatively black on the images), with no differentiation between gray and white matter. The central end of the anterior median fissure produces an echo interface that appears as a short linear or oval white dot near the center of the cord2 (Figs. 6.1, 6.2B). The central canal does not produce a separate echo unless it is enlarged, as in hydromyelia. Fig. 6.1 Midline longitudinal sonogram of the distal spinal cord in a normal 1-week-old girl. Not the hypoechoic spinal cord parenchyma. The skips in the central echo (ce) are from shadowing of the overlying spinous processes (sp). d, dura; cm, conus medularis. (From Nelson MD Jr, Sedler JA, Gilles FH. Spinal cord central echo complex: histoanatomic correlation. Radiology 1989; 170:479–481. Reprinted with permission.) In a few neonates, the central canal enlarges in the lumbar enlargement as a normal variant, the so-called ventriculus terminalis.4 Nerve roots, dentate ligaments, and arachnoid septations can be defined around the spinal cord (Fig. 6.2). The individual layers of skin, subcutaneous fat, fascia, and paraspinal muscles are well defined and separated by continuous echogenic lines at each interface (Fig. 6.2C). Most importantly, the exact position of the conus medullaris can be determined relative to the vertebral bodies.5,6 At birth (term gestation) the conus is normally located above the lower border of L3. A spinal cord below the lower border of L3 is considered abnormal. The filum terminale can be seen from its origin at the tapered end of the conus and followed as it courses between the nerve roots of the cauda equina to where it pierces the distal tapered end of the thecal sac at S2 (Fig. 6.2E). The extradural filum is not identifiable within the sacral canal as it courses to insert into the periosteum of the coccyx. The filum should not be larger than 3 mm in diameter. The spinal cord is suspended within the thecal sac by 21 pairs of triangular fibrous bands called dentate ligaments.7 These ligaments are continuous with the pia mater along the lateral surface of the spinal cord between the dorsal and central nerve roots. The ligaments narrow to a point and laterally insert into the dura at regular intervals. The dentate ligaments limit craniocaudal movement of the spinal cord without restricting anteroposterior (AP) movement.7 In real-time scanning mode, the spinal cord is seen to be centered slightly below the midpoint of the spinal canal. From this baseline, the cord intermittently deflects 2 to 3 mm in the AP direction and returns to the baseline position. In the prone position, these “pulses” of the spinal cord match the arterial pulse of the radial artery at the wrist. The movement of the spinal cord is secondary to the vascular pulsations from the radicular arteries and pulsations of the brain.8,9 Normal respiration will change the baseline position of the cord because the thecal sac varies in size with the amount of blood in the surrounding epidural venous plexus. The venous flow is directly related to the changing intrathoracic pressure with respiration. Similarly, a Valsalva maneuver will deflect the spinal cord by the same mechanism.10 Fig. 6.2 Ultrasound study in a normal 3-day-old boy. (A) Midline longitudinal sonogram shows the location of the transverse images in (B-E). cm, conus medullaris; sc, spinal cord; nr, nerve roots of the cauda equina. (B) Transverse sonogram at the T10 level. Note hypoechoic cord parenchyma and central echo (ce), and the echogenic “halo” around the cord produced by the nerve roots, blood vessels, and arachnoid septations. d, dura; TP, transverse process of the T10 vertebral arch. Arrowheads mark the skin surface. (C) Transverse sonogram at the L2 level. Note the tapered conus medullaris (cm) and “X” pattern of the surrounding nerve roots. 1, skin surface; 2, interface of skin with subcutaneous fat; 3, lumbodorsal fascia. (D) Transverse sonogram at the L3 level. nr, bundles of nerve roots of the cauda equina; d, dorsal aspect of the dural sac; TP, transverse process of L3. (E) Transverse sonogram at L5. The filum (f) is seen between the two lateral nerve root bundles (nr) of the cauda equina. Postural changes of the patient also influence the baseline position of the spinal cord. Maximally flexing the neck causes the cervical and upper thoracic spinal cord to move anteriorly. In the sitting position, maximally flexing the patient at the hips causes the thoracic cord to move anteriorly. The amount of spinal cord displacement varies with each individual and is probably related to the degree of curvature of each spine. Of interest, in normal controls, maximal flexion may cause the thoracic spinal cord to move anteriorly against the posterior vertebral body and cease normal pulsations.
How Ultrasonography Works
Imaging the Spinal Canal and Contents
Technique
Findings
Ultrasonographic Findings for Normal Anatomy1–3
Ultrasonographic Findings for Normal Physiological Motion of the Spinal Cord
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







