Chapter 20 Musculoskeletal ultrasound imaging
HISTORY
Musculoskeletal ultrasound applications began to emerge in the mid-1980s (Crass et al 1984) as the resolution of scanners improved. Physiotherapy researchers found ultrasound to be ideal for the direct visualization and evaluation of both muscle size and activity (Stokes&Young 1986). By the late 1990s, the development of high-frequency probes, with resolution in some respects superior to MRI, had led to renewed interest in musculoskeletal ultrasound. This continues today as falling costs and increased portability have made high-resolution ultrasound imaging feasible in the clinic and on the ward.
PRINCIPLES
SCANNERS
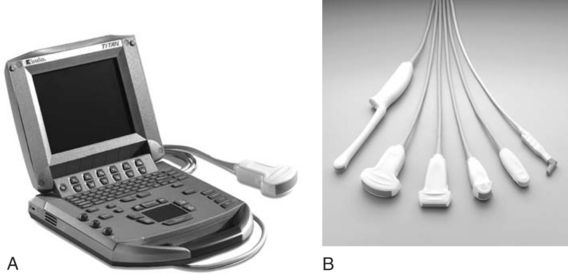
Scanners are typically made up of one or more hand-held probes attached via flexible cables to a central unit, which processes and displays the image (Fig. 20.1). The probes operate at one or more fundamental frequencies, which determine the maximum depth and resolution of the images they generate. At higher frequencies, the shorter wavelengths mean that shorter pulses can be produced, giving better resolution. At lower frequencies, the resolution is reduced but the ultrasound is absorbed less readily as it passes through the body, enabling deeper structures to be examined.
The most commonly used probes are the linear and curvilinear probes (Fig. 20.1B). Linear probes are normally designed to operate at frequencies of 7.5 MHz and above; these produce high-resolution, rectangular images to a depth of around 5 cm. Curvilinear probes generate a fan-shaped image with a wider field of view than a linear probe. They operate at lower frequencies, typically between 2 and 5 MHz, and can produce images to a depth of up to 15 cm but at the cost of lower resolution.
A detailed discussion of resolution and image generation lies beyond the scope of this chapter and the reader will find more comprehensive descriptions in dedicated ultrasound texts, in particular Hedrick et al (2005).
DOPPLER
Colour Doppler
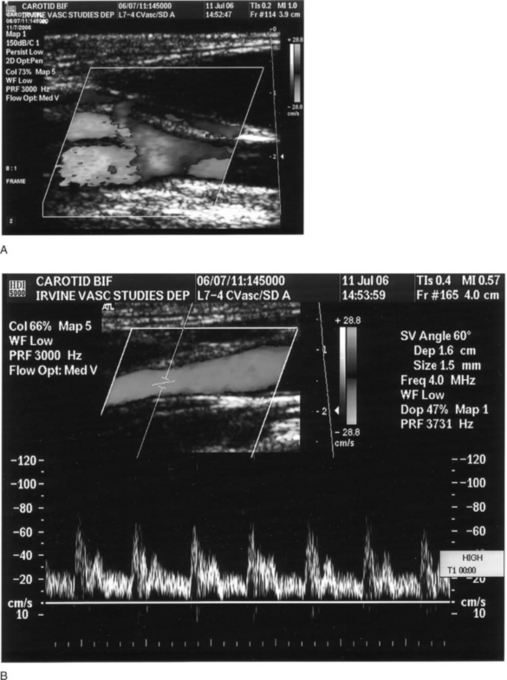
This samples the flow velocities over a wider area of the image and displays the presence of flow by adding colour to the greyscale image (Fig. 20.2A). Blue and red are typically used, although these represent flow either away or towards the ultrasound probe rather than venous and arterial flow.
Pulsed or spectral Doppler
This detects the flow of blood through a small part of the image and displays it in the form of the spectrum of velocities detected against time (Fig. 20.2B).
APPEARANCES: FEATURES OF AN ULTRASOUND IMAGE
Typical appearance of normal tissue
Figure 20.3 demonstrates some typical appearances of soft tissues:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree