Chapter 9 The following snapshots from overnight PSG tracings highlight some of these uncommon, atypical, and often unrecognized patterns (Figs. 9.1 to 9.19). FIGURE 9.1 A case of sweating in rapid eye movement (REM) sleep. FIGURE 9.2 The effect of lateral head position on sleep-disordered breathing (SDB). FIGURE 9.3 Periodic limb movements in sleep occurring synchronously in cranially and spinally innervated muscles. FIGURE 9.4 Propriospinal propagation of periodic limb movements of sleep. FIGURE 9.5 Expiratory bursts in the rectus abdominis muscle. FIGURE 9.6 Painless limbs and moving toes syndrome. FIGURE 9.7 A case of rhythmical leg movements with rapid blinking in wakefulness.
Uncommon, Atypical, and Often Unrecognized PSG Patterns
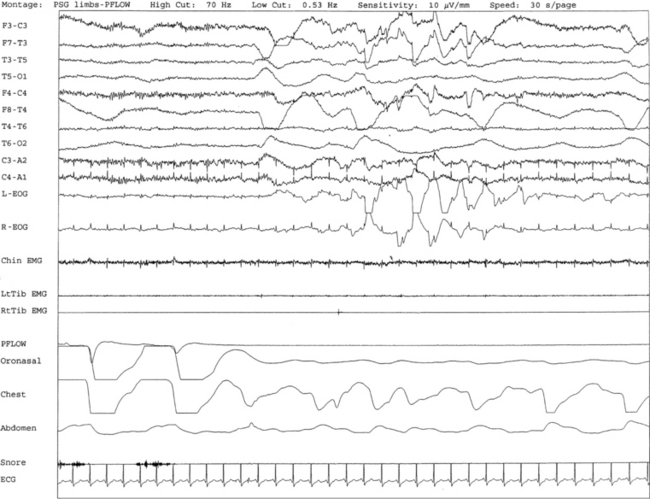
Overnight polysomnogram (PSG) shows evidence of severe upper airway obstructive sleep apnea with an apnea-hypopnea index of 51.3/hr in a 71-year-old man with history of snoring, difficulty breathing in sleep, and excessive daytime sleepiness despite uvulopalatoplasty performed 2 years ago for treatment of obstructive sleep apnea. Medical history is significant for hypertension. In addition, the PSG shows the presence of sweating recurrently and exclusively during REM sleep while being conspicuously absent during non-REM sleep. This is an atypical finding, raising the suggestion of REM sleep dysregulation. This figure shows a 30-second excerpt in REM sleep taken from overnight PSG recording showing sweat artifact as described for Figure 1.7. Top 10 channels, Electroencephalography; L-EOG and R-EOG, left and right electro-oculograms; electromyography of chin; LtTib and RtTib EMG, left and right tibialis anterior electromyography; PFLOW, nasal pressure transducer; oronasal thermistor; chest and abdomen effort channels; snore monitor; ECG, electrocardiography.
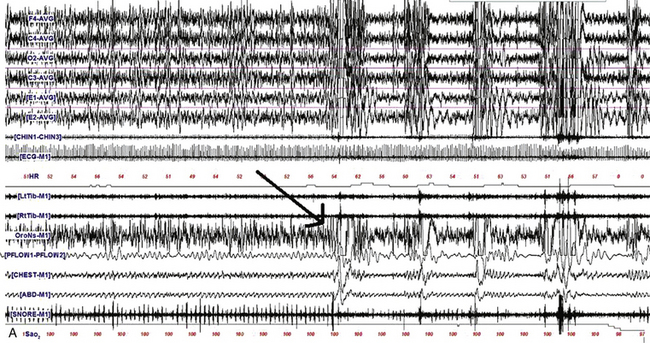
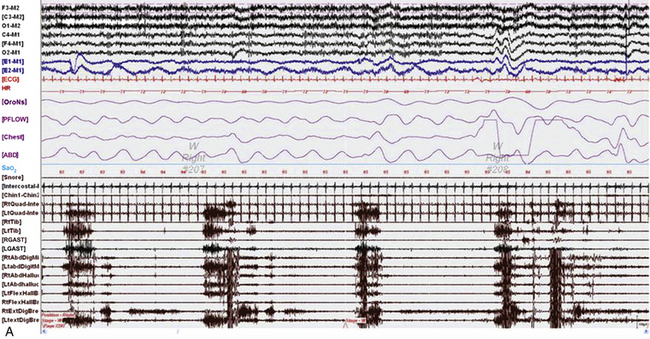
A, A 480-second epoch of polysomnographic tracing from stage N2 sleep in a 63-year-old man showing supine body position with head initially turned to the left and then to the right (arrow marks point of head position change). Note the immediate appearance of respiratory events with the head turned to the right. B, A 480-second excerpt from stage N2 sleep in a 6-year-old boy showing supine body position with head initially supine and then turned to the left (first arrow marks the point of this change). Respiratory events improved after 2 to 3 minutes in the same position (second arrow). Although worsening of obstructive sleep apnea with the supine body position is well known, recent reports have also confirmed that sleep-disordered breathing worsens with the head supine. However, worsening of sleep-disordered breathing with the head turned laterally to one side or the other and the body remaining supine as illustrated in this example is unusual. Top four channels in A and eight channels in B, Electroencephalography (international 10-20 electrode nomenclature); E1-M1 and E2-M1, left and right electro-oculogram; CHIN1-CHIN2, chin electromyography; ECG, electrocardiogram; HR, heart rate; LtTib and RtTib, left and right tibialis anterior electromyogram (EMG); LGAST and RGAST, left and right gastrocnemius EMG; OroNs and PFLOW, respiratory air flow; Chest and ABD, respiratory effort; Sao2, arterial oxygen saturation by finger oximetry; snore channel. (Reproduced with permission from Riar S, Bhat S, Kabak B, Gupta D, Smith I, Chokroverty S. The effect of lateral head position on sleep disordered breathing: a case series. Sleep Med. 2013;14[2]:220-221.)
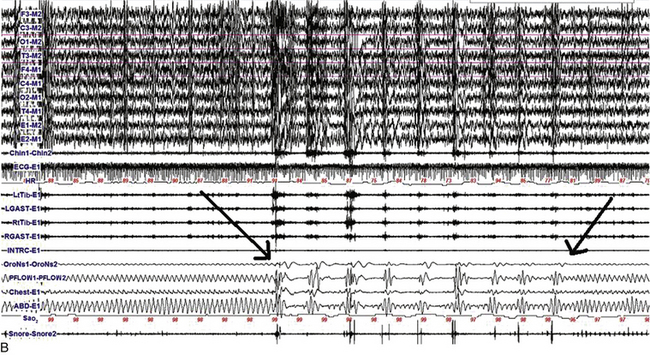
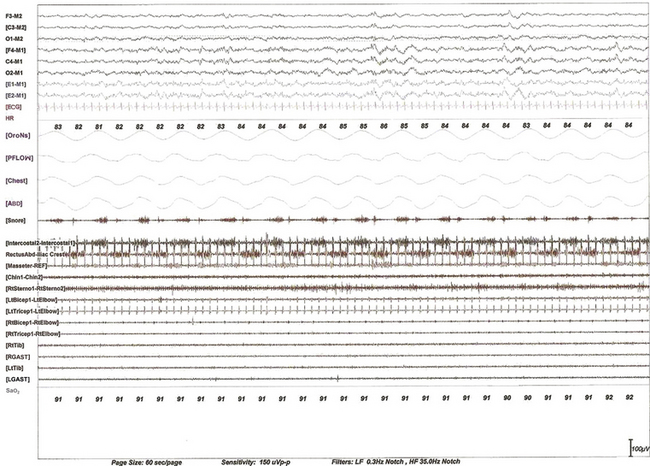
A 60-second epoch from the overnight polysomnogram of a 43-year-old woman referred for excessive leg movements in sleep. Note bursts of periodic limb movements in sleep occurring synchronously in cranially innervated (sternocleidomastoideus, chin, and masseter) and spinally innervated (quadriceps, gastrocnemius, and tibialis) muscles. Top six channels, Electroencephalogram (international nomenclature system); E1-M1 and E2-M1, left and right electro-oculogram, respectively; ECG, electrocardiogram; HR, heart rate; OroNs, oronasal thermistor; PFLOW, nasal pressure transducer; CHEST and ABD, chest and abdominal respiratory effort channels; Sao2, arterial oxygen saturation by finger oximetry; Chin1-Chin2, submentalis electromyogram (EMG); Masseter-REF, masseter EMG; RtSterno1-RtSterno2, sternocleidomastoideus EMG; RtBicep1-RtElbow, LtBicep1-LtElbow, right and left biceps brachii EMG; RtTricep1-RtElbow, LtTricep1-LtElbow, right and left triceps EMG;. RtTib, LtTib, right and left tibialis anterior EMG; RGAST, LGAST, right and left gastrocnemius EMG. Also included is a snore channel.
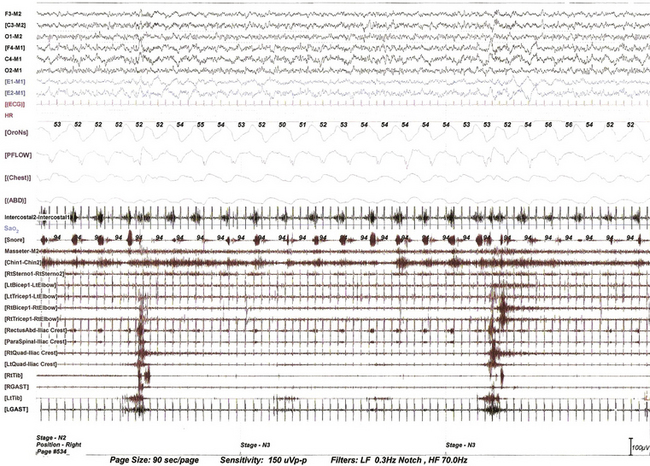
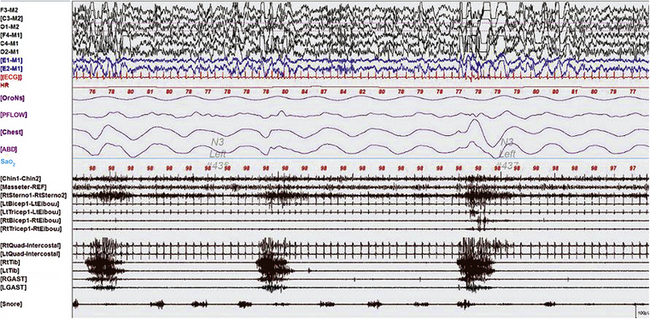
This 90-second epoch of stage N3 sleep is taken from the overnight polysomnographic (PSG) recording using multiple muscle montage in a 66-year-old man with a history of restless legs syndrome (Willis-Ekbom disease), fulfilling all the essential diagnostic criteria for this. Note periodic limb movements in sleep (PLMS) originating first in the tibialis anterior and propagating up the spinal cord to the quadriceps muscle and subsequently to the rectus abdominis, paraspinals, and then to the biceps and triceps muscle at a very slow speed (note prolonged interburst intervals between the lower limb, trunk, and upper limb muscles). This suggests propagation along slowly conducting propriospinal pathways. It is not possible to measure exact interburst latencies using our PSG equipment. Note also the inspiratory muscle bursts in cranially innervated muscles (secondary respiratory muscles). The upper rectus abdominis and paraspinal muscles are picking up inspiratory bursts from neighboring intercostal and diaphragmatic muscles. Top six channels, Electroencephalogram (international nomenclature system); E1-M1 and E2-M1, left and right electro-oculogram, respectively; M1, left mastoid; ECG, electrocardiogram; HR, heart rate; OroNs, oronasal thermistor; PFLOW, nasal pressure transducer; Chest and ABD, chest and abdominal respiratory effort channels; Intercostal, intercostal EMG from the right eighth intercostal space; Sao2, arterial oxygen saturation by finger oximetry; channels 18 to 32, EMGs from masseter, chin (mentalis muscle), sternocleidomastoideus, biceps, triceps, rectus abdominis (right), paraspinal (right thoracolumbar), quadriceps (left and right), gastrocnemius (RGAST and LGAST), and tibialis anterior (RtTib and LtTib) muscles.
A 60-second epoch from the polysomnogram of a 63-year-old woman referred for possible obstructive sleep apnea. This study was performed with a multiple muscle montage. Note the occurrence of alternating muscle bursts in the intercostal electromyogram (EMG) channel (during inspiration, accompanied by snoring as noted in the snore channel) and in the lower rectus abdominis muscle (during expiration). Top six channels, Electroencephalogram (international nomenclature system); E1-M1 and E2-M1, left and right electro-oculogram, respectively; ECG, electrocardiogram; HR, heart rate; OroNs, oronasal thermistor; PFLOW, nasal pressure transducer; Chest and ABD, chest and abdominal respiratory effort channels; Intercostal, right intercostal EMG channel. RectusAbd-Iliac Crest, lower right rectus abdominis EMG channel; Masseter-REF, masseter EMG; Chin1-Chin2, submentalis EMG; Rt Sterno1-Rt Sterno2, right sternocleidomastoideus EMG; Rt Triceps1-RtElbow, Lt Triceps1-LtElbow, right and left triceps EMG; RtTib, LtTib, right and left tibialis anterior EMG; RGAST, LGAST, right and left gastrocnemius EMG; Sao2, arterial oxygen saturation by finger oximetry. Also included is a snore channel.
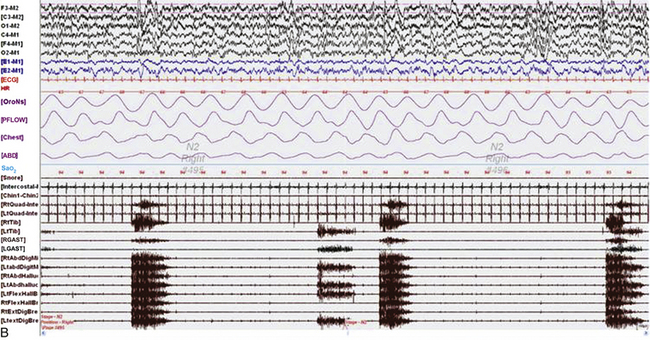
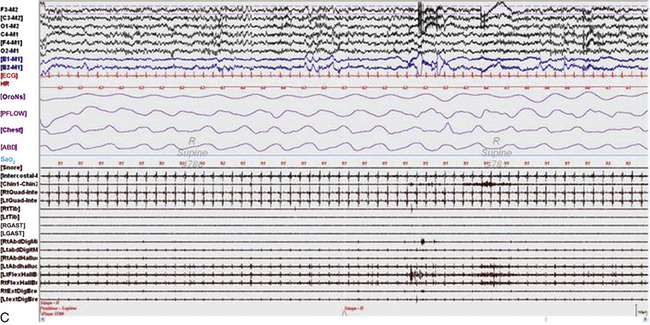
Sixty-second epochs from the overnight polysomnogram with foot montage (see Table 1.6) in a 74-year-old woman with bradykinesia and postural instability. She was on carbidopa/levodopa and complained of painless, involuntary toe movements, which appeared about an hour before her next dose was due and responded to the medication. Note the occurrence of simultaneous dystonic bursts in multiple foot muscles bilaterally occurring in wakefulness (A) and non–rapid eye movement (NREM) sleep stage N2 (B), but markedly reduced in REM sleep (C). This appears to be a variant of painless limbs and moving toes syndrome. Studies have shown that toe movements in painless limbs and moving toes syndrome may be a combination of synchronous and asynchronous, myoclonic (less than 200 msec) and dystonic (greater than 200 msec, mostly 500 to 1000 msec) bursts; they may persist into various stages of sleep and may be associated with cortical arousals. Top six channels, Electroencephalogram (international nomenclature system); E1-M1 and E2-M1, left and right electro-oculogram, respectively; ECG, electrocardiogram; HR, heart rate; OroNs, oronasal thermistor; PFLOW, nasal pressure transducer; Chest and ABD, chest and abdominal respiratory effort channels; Sao2, arterial oxygen saturation by finger oximetry; Chin1-Chin2, submentalis electromyogram (EMG); RtQuad, LtQuad, right and left quadriceps femoris EMG; RtTib, LtTib, right and left tibialis anterior EMG; RGAST, LGAST, right and left gastrocnemius EMG; RtAbdDigM, LtAbdDigMin, right and left abductor digiti minimi EMG; RtAbdHalluc, LtAbdHalluc, right and left abductor hallucis EMG; RtFlexHallB, LtFlexHAllB, right and left flexor hallucis brevis EMG; RtExtDigBre, Lt ExtDigBre, right and left extensor digitorum brevis EMG. Also included are a snore channel and an intercostal EMG (below snore channel).
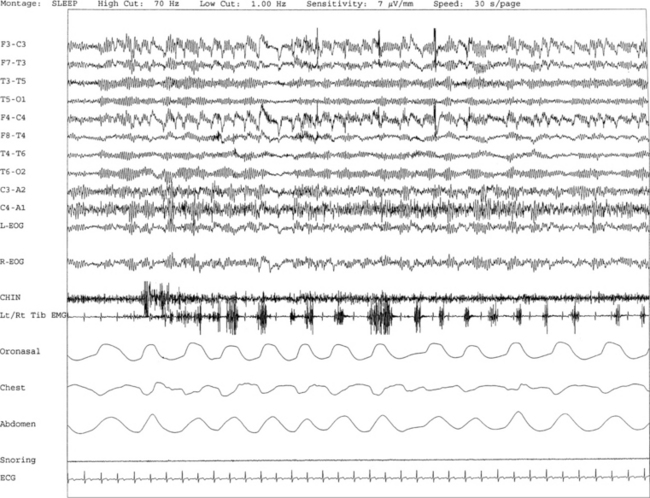
A 70-year-old woman with history of insomnia and early morning awakenings. Normal neurological examination with no evidence of Parkinson’s disease or other neurodegenerative disorders. Nocturnal polysomnogram (PSG) revealed mild obstructive sleep apnea. An unusual pattern of episodes of rhythmical leg movements at approximately 0.5 to 1.5 Hz and rapid blinking are noted repeatedly during periods of wakefulness but not during sleep. The significance of these events limited to wakefulness remains uncertain. One such 30-second epoch is demonstrated. Top 10 channels, Electroencephalogram; L-EOG and R-EOG, left and right electro-oculograms; electromyography of chin; Lt/Rt Tib EMG, left and right tibialis anterior EMG; oronasal thermistor; chest and abdomen effort channels; snore monitor; ECG, electrocardiography.
Uncommon, Atypical, and Often Unrecognized PSG Patterns
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree







