Fig. 19.1
Selective intra-arterial DSA images of the segmental artery at the level of T12 on the right side (a). The vessel originates from the thoracic aorta. After giving off branches for the supply of the vertebral body, nerve root, and dura (arrow), it continues as an intercostal artery. Above the level of T5, the upper thoracic segmental arteries (arrowheads) are supplied from a common trunk (b)
In the lower lumbar region, the level of the aortic bifurcation is variable. The median sacral artery originates at the junction between both common iliac arteries (Fig. 19.2). The sacrum and sometimes the lower lumbar spine are supplied by the iliolumbar trunk originating from the internal iliac arteries (Fig. 19.2).
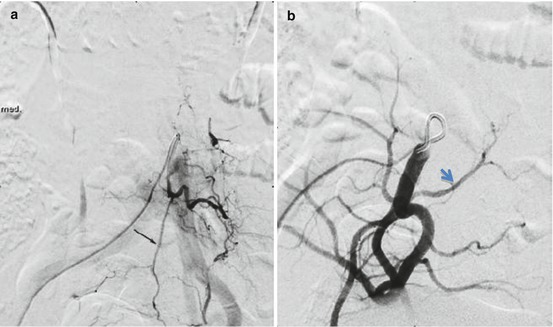
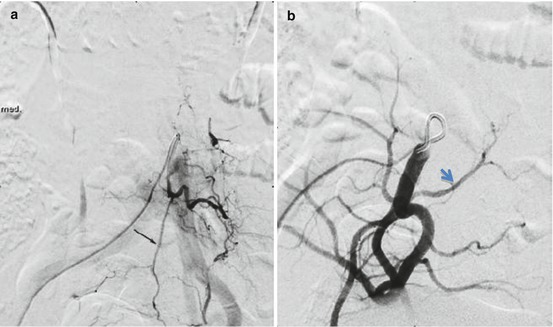
Fig. 19.2
Median sacral artery (arrow) originating together with the left L5 segmental artery from the aortic bifurcation (a). Selective injection of the internal iliac artery on the right side with iliolumbar truncus (arrowhead, b)
At the level of the intervertebral foramen, small branches to the dura and the nerve roots (radicular arteries) take off from the segmental arteries. The spinal cord arterial supply is provided by the anterior spinal artery running longitudinally at the ventral surface of the spinal cord. In the posterior fossa, the anterior spinal artery arises from the junction of two arteries originating from the V4 segments of the vertebral arteries (Fig. 19.3). The anterior spinal artery is fed by radiculomedullary arteries arising at different levels, but not in every segment. Radiculomedullary arteries can be identified due to the ascending course following a nerve root and a hairpin-shaped curve at the junction with the anterior spinal artery (Fig. 19.4). A larger radiculomedullary artery is frequently located at the thoracolumbar junction between T11 and L2. This artery of the lumbar enlargement (Adamkiewicz) is an important but not the only supply to the lower part of the anterior spinal cord with some variation in the number and location of radiculomedullary arteries. The posterolateral portions of the spinal cord are supplied by two posterior spinal arteries and a pair of posterolateral spinal arteries which are part of a pial arterial network. Feeders come from radiculopial arteries, which show also a hairpin shape, but are located lateral to the midline (Fig. 19.4). In the upper cervical spine, the posterior spinal artery equivalent is called lateral spinal artery.

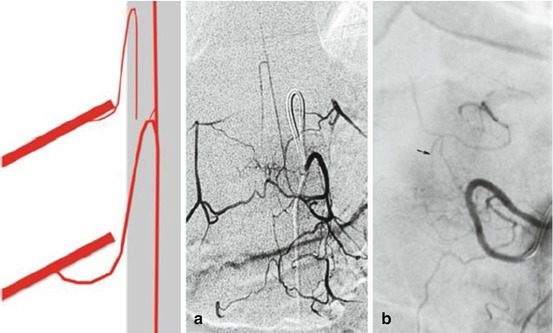

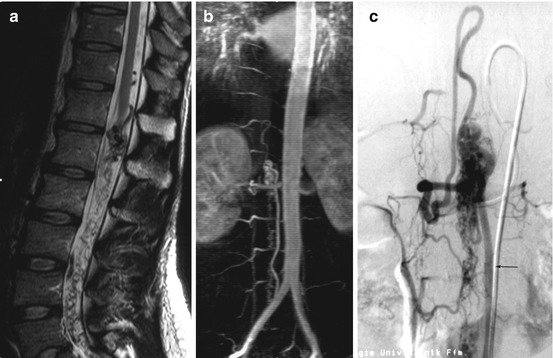
Fig. 19.3
Segmental arteries arising from the left vertebral artery. Note the weak opacification of the anterior spinal artery fed by radiculomedullary branches at single levels (arrow)
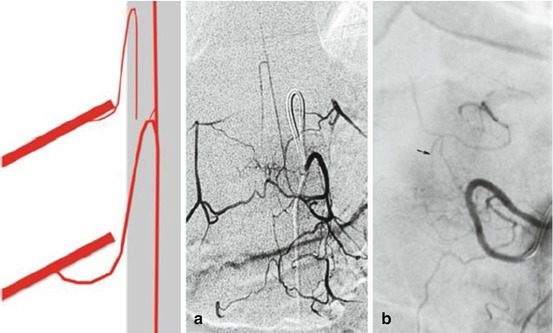
Fig. 19.4
Typical hairpin shape of a radiculomedullary artery supplying the anterior spinal artery in the midline (a). Note the paramedian course of the smaller radiculopial artery (schematic representation and b) showing also a hairpin shape which is sometimes difficult to distinguish from anastomotic arteries dorsal to the vertebral arch and spinal process (arrows)
Radial perforators are originating from this pial network (vasa corona) for the supply of the parenchyma. From the anterior spinal artery sulcocommissural branches are arising in the ventral sulcus of the spinal cord penetrating alternate into the left or right parenchyma and supplying the central gray matter and surrounding structures. This is the intrinsic system of the spinal cord supply, whereas the extrinsic system is supplied by the vasa corona. Therefore, in the case of an occlusion of the anterior spinal artery, infarcts may occur in the territory of these sulcocommissural branches (intrinsic system), whereas the periphery is still supplied via the pial network (extrinsic system; see also Chap. 20) (Fig. 19.5).
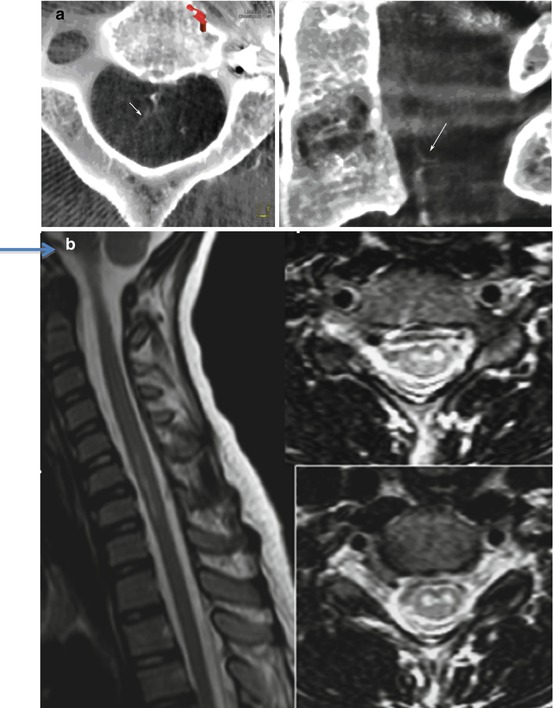
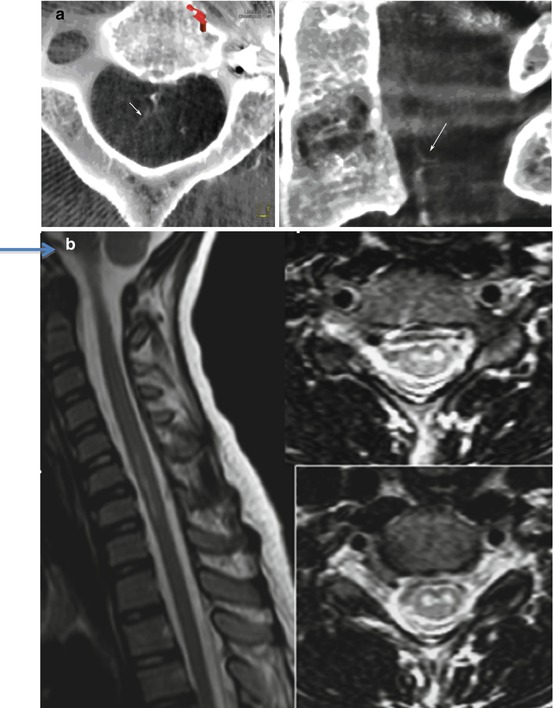
Fig. 19.5
Flat panel CT angiography (CTA) showing sulcocommissural branches arising from the anterior spinal artery at the level of C2 (a). MRI shows a patient with a spinal infarction after occlusion of the anterior spinal artery (b) Note that the periphery of the spinal cord is preserved due to supply via the pial network (extrinsic system)
19.2.2 Veins
The spinal cord is surrounded by a venous network with dominating longitudinal veins at the ventral and dorsal surface of the spinal cord. These venous anastomoses are connected with radicular veins connecting the spinal cord drainage to epidural veins. Normally, a valve-like mechanism prevents reflux from epidural veins into intradural veins.
The epidural venous plexus is draining through the intervertebral foramina into longitudinal venous channels which are connected with the azygos and hemiazygos venous system. Spinal cord veins are visible in the late phase of selective spinal angiograms, especially if varicose enlargement occurs in the presence of AV (arteriovenous) shunts due to vascular malformations (Fig. 19.6).
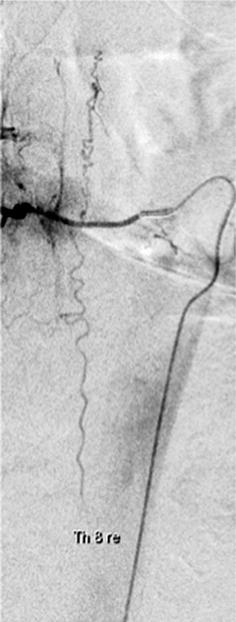
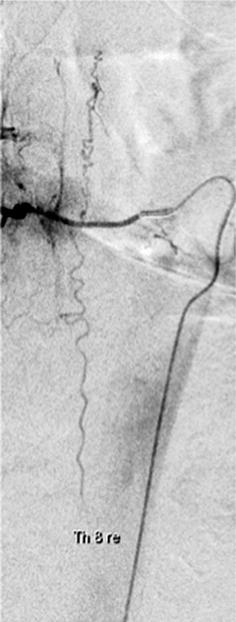
Fig. 19.6
Varicose enlargement of an ascending and descending spinal cord vein in a case with dural AV fistula (AVF)
19.3 Basics of Spinal Angiography
19.3.1 DSA
In former times, spinal angiography was regarded as a difficult, time-consuming, and dangerous examination for imaging of the spinal cord vessels. Adequate catheter techniques, modern nonionic contrast material, and additional use of MRI for targeted examinations have improved feasibility and safety of spinal angiograms.
MRI together with contrast-enhanced and time-resolved MR angiography (MRA) may help a lot to localize, e.g., dural AV fistulas (AVF) and other vascular spinal lesions and may abandon catheterization of all segmental arteries; of the external carotid, vertebral, and cervical arteries; and of the iliac arteries.
Spinal angiograms are performed via the transfemoral route with the use of selective catheters with a shape adapted to the course of the initial segments of the segmental arteries. In our experience, the “Michaelsen-type” catheter or renal shape for the lumbar arteries covers most of the anatomic situations. For catheterization of the internal iliac artery, “Sidewinder I” configurations are favorable as well as “vertebral configured” catheters for the cervical vessels, especially the vertebral arteries.
A systematic approach with exact localization of the catheterized segments is mandatory to be sure that the spinal angiogram is complete and that all radicular feeders can be analyzed especially when spinal arteriovenous malformations (AVM) are assumed.
During catheterization, the catheter tip must be turned away from the ventrally located visceral arteries or the lateral renal arteries. In elderly patients suffering from arteriosclerosis, it is sometimes not easy to find and differentiate a narrowed ostium of a segmental artery from adjacent plaques. Catheterization must be performed gently and dissections have to be strictly avoided. The extent of spinal angiography varied for different indications and is explained in the pathology section.
After catheterization of a segmental artery, we manually inject a few milliliters of nonionic contrast material and perform a DSA series with 2 f/s during breath holding. In the lumbar region, temporary arrest of bowel movements by intravenous injection of butylscopolamine or glucagon is mandatory for good image quality.
19.3.2 MRI, MRA, and CTA of the Spinal Vasculature
On contrast-enhanced T1W MR images, frequently normal spinal veins can be detected. With modern MR equipment, there is a wide range of normal findings (Fig. 19.7).


Fig. 19.7
Contrast-enhanced and time-resolved MRA in a patient with radicular pain at the level of T1. MRA shows pathological veins in projection on the upper thoracic spine (a, b). Selective angiography of the left upper thoracic segmental artery shows the opacification of a mainly venous vascular malformation
MRI and MRA are frequently used to localize a vascular lesion at the spine and to guide selective angiography and to avoid injection of all potential spinal arteries. Contrast-enhanced MRA techniques like contrast-enhanced TOF or time-resolved MRA as well as multiplanar reconstructions of contrast-enhanced GRE images allow for reliable visualization of pathological vessels (see Chap. 5). Frequently, the localization of AV shunts can be estimated correctly but should be confirmed by selective angiography (Fig. 19.7). Multidetector or flat panel CTA is also used for imaging of spinal vessels and vascular pathologies (see Fig. 19.5).
19.4 Common Vascular Diseases of the Spine and Spinal Cord
19.4.1 Spinal Cord AVM and Perimedullary AV Fistula
Vascular malformations involving the spinal cord or the surrounding pial vessels are rare diseases and uncommon. They may become symptomatic with subarachnoid or parenchymal hemorrhage or with ischemic neurological deficits related with AV shunting. MRI and MRA are the methods of choice if spinal AVMs are suspected, and angiography is often not needed for screening or even for making the diagnosis (Fig. 19.8).