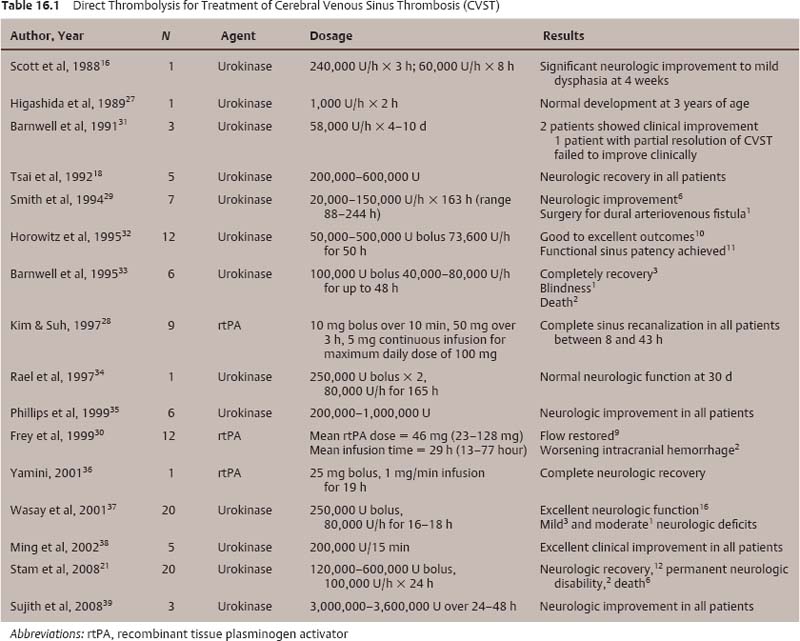
Chapter 16 Cerebral venous sinus thrombosis (CVST) is a relatively rare disease that accounts for less than 1% of all strokes.1 The exact incidence of CVST is unknown, but ranges from 0.03% to as high as 9% on autopsy series.2–5 Various factors are believed to contribute to CVST. Hypercoagulable states, infection of cranial sinuses and otitis, as well as the use of oral contraceptives have all been implicated as causative factors. Interestingly, as high as 40% of cases are thought to be idiopathic.6 CVST is more common in young women, particularly during puerperium.7,8 Headache is the most common presentation and is estimated to occur in up to 80% of cases.8 Other symptoms related to elevated intracranial pressure are common including nausea with or without emesis and visual disturbances. Focal neurologic deficits or seizures may occur in conjunction with venous hypertension or related cerebral infarction or hemorrhage.9 The natural course of CVST is variable, and treatment guidelines are not well established. The goal of therapy is to recanalize the affected venous sinus (es) to improve clinical signs and symptoms. Patients with elevated intracranial pressure secondary to venous hypertension should be treated aggressively with mannitol, hyperventilation, and/or cerebrospinal fluid diversion in accordance with their neurologic status. Seizures should be controlled with anticonvulsants. Systemic and/or direct thrombolysis should be initiated once the patient has been stabilized from a respiratory and hemodynamic standpoint. Rapid deterioration in a patient’s neurologic status requires emergent intervention. Multiple publications have described the successful treatment of CVST with resolution of neurologic symptoms using heparin. Two small randomized controlled trials have evaluated the effects of systemic heparinization in the treatment of CVST.10,11 One study found an eightfold increased likelihood of patients with CVST having improved neurologic function at 3 days, 8 days, and 3 months after systemic anticoagulation with heparin compared with controls.11 A retrospective analysis of a subgroup of patients with CVST in this study showed that systemic heparinization in the setting of intracranial hemorrhage was safe. The second study, however, failed to demonstrate improved outcomes in patients who received low-molecular-weight heparin relative to controls.10 Neither study demonstrated improved overall survival with heparin therapy. The International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) was a multinational prospective observational study that enrolled 624 adult patients diagnosed with CVST.12 Although the choice of therapy was not regimented, 520 (83%) of the patients were anticoagulated acutely with either intravenous (IV) heparin (64%) or low-molecular-weight heparin (35%). At a median follow-up of 16 months, 57% of patients were asymptomatic and ~32% of patients had mild or moderate impairments. Patient factors predictive of worse outcome on multivariate analysis included coma at the time of presentation, thrombosis of deep cerebral veins, cancer, and central nervous system infection. Systemic thrombolysis using urokinase and recombinant tissue plasminogen activator (rtPA) has been performed in animals 13 and human case reports exist.14 Although evidence suggests that these agents may effect sinus recanalization, the increased anecdotal risk of hemorrhagic complications makes them less attractive options. The goal of systemic heparin therapy is to maintain the activated partial thromboplastin time at 2 to 2.5 times normal. Once the patient’s neurologic condition has stabilized, Coumadin therapy is initiated with an INR goal between 2 to 3 for 6 months. Prolonged anticoagulation (> 6 months) is recommended for patients with hereditary thrombophilias or recurrent CVST.15 Direct thrombolysis is reserved for patients who derive no clinical benefit from systemic anticoagulation or for patients with rapidly deteriorating neurologic status. Various techniques for direct thrombolysis have been described in multiple case series (Table 16.1). The earliest published reports involved prolonged local infusions of urokinase into the superior sagittal sinus through direct sinus cannulation following either midline craniotomy 16 or percutaneous transcranial puncture.17 Advances in endovascular technology have nearly obviated the need for direct sinus cannulation. Since its initial description by Tsai and colleagues, 18 transfemoral venous puncture has become the preferred method of accessing the intracranial venous sinuses. Sinus recanalization, as confirmed by serial intracranial venography, is typically achieved through prolonged infusions of urokinase (no longer commercially available in the United States) or rtPA. Patients typically remain on systemic anticoagulation for 6 months following direct thrombolysis. Direct chemical thrombolysis may be augmented by various mechanical thrombolytic techniques. Balloon catheter thrombectomy, 19–21 rheolytic therapy using the AngioJet catheter system (Possis Medical, Minneapolis, MN), 22–26 and snare devices 27 have been used successfully to achieve sinus recanalization in combination with various systemic or direct thrombolytic therapies. Only one prospective study of direct thrombolysis for CVST has been published to date.21 It used a combination of mechanical and chemical thrombolytic techniques on 20 patients, 12 of which were comatose prior to treatment. Fifteen patients underwent chemical thrombolysis with direct urokinase infusion into the superior sagittal and straight sinuses combined with thrombosuction via a rheolytic catheter and thrombectomy using a Fogarty catheter. Nine patients fully recovered, but six patients died of complications related to CVST.
Venous Sinus Thrombosis Recanalization Techniques
 Background
Background
 Indications
Indications
 Techniques
Techniques
Systemic Thrombolysis
Direct Thrombolysis
Procedural Description
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree