36 Vertebral Body Stenting
KEY POINTS
Introduction
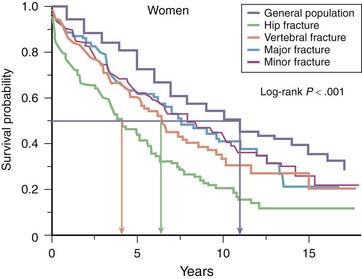
Vertebral body compression fractures (VBCFs) are the hallmark of osteoporosis, and their incidence increases exponentially with increasing age. VBCFs are related to important morbidity and loss of quality of life comparable to that in hip fractures (Figure 36-1).1,2
The treatment of painful VBCFs with percutaneous cement reinforcement has a long history and appears very effective in a very high percentage of patients treated. There are many case series published that support this treatment, with the most recent publication also providing encouraging long-term results.3–5 Furthermore, there is class A evidence based on a large multicenter Randomized Clinical Trial (RCT) comparing percutaneous cement reinforcement after cavity creation with a balloon against conservative treatment. This study clearly shows a superiority of cement reinforcement for pain, activity level, and pain medication in the first year of treatment.6 Although the study is comparing kyphoplasty as a specific technique of reinforcement against conservative treatment, based on several review articles, there is no clinical advantage of kyphoplasty over vertebroplasty.7,8 Most recently, two studies were published comparing vertebroplasty with a sham procedure showing no difference in early outcome. Although the studies show a randomized design with independent assessment, there seems to be a selection bias because the inclusion of patients took several years even though a multicenter study design was used.9,10
Although cement reinforcement can stabilize a fracture and therefore decrease pain, height restoration remains an issue, that is not solved yet. Kyphoplasty was introduced initially with the idea to restore vertebral body height. However, the amount of height gain remained very modest, and its clinical impact remains obscure. With the inflation of the balloon, excellent height reduction can be achieved, but after deflation a major amount of the reduction gets lost.11
The consequences of vertebral height loss and increased kyphosis are reported in several epidemiological studies: impaired quality of life and even an increased mortality are documented (see Figure 36-1).2,12,13
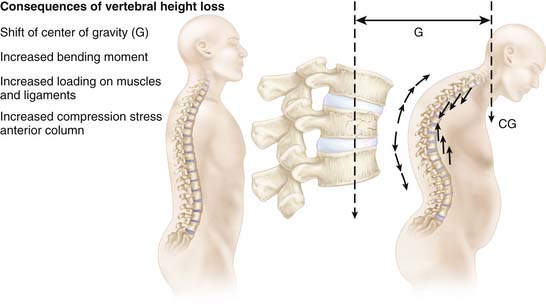
The kyphotic deformity leads to a shift of center of gravity and consecutively to an increased load on the anterior column. Consequently, there is an increased risk for new fractures.14,15 Furthermore the increased kyphosis raises the load of the back muscles enormously (Figure 36-2).16,17
Vertebral Body Stent
In Vitro Testing
Extensive cadaver testing allowed proof of the feasibility of the concept, and in a sophisticated in vitro setup, one could clearly demonstrate the superior potential for height maintenance in comparison to the balloon insertion only with sound significance (Figure 36-3).18
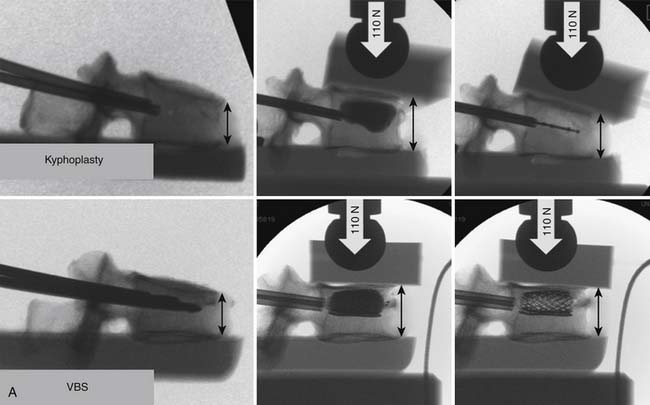
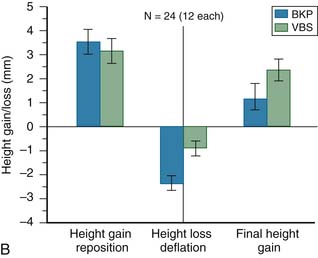
FIGURE 36-3 A, Comparison of a kyphoplasty procedure and a vertebral body stenting system as assessed in a cadaver model with a preload of 110 N.21,22 Initial reduction can be achieved equally well with both systems. After deflation of the balloon there is a significant loss of reduction with the kyphoplasty system (∗), whereas the height can be maintained with the VBS (∗∗). B, Summary of twelve pairs of vertebrae tested. Initial height gain is similar in both techniques. Loss of height is observed with both systems, but significantly less with VBS (p = .024), and consequently the overall height restoration is superior with the VBS system (p = .035). (From Wilke HJ, Neef P, Caimi M, Hoogland T, Claes LE. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine 1999;24-8:755-762; and Sato K, Kikuchi S, Yonezawa T. In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine 1999;24-23:2468-2474.)
Clinical Application
Indications
The use of the vertebral body stent (VBS) is indicated in acute and subacute painful VBCFs with at least 15% of height loss and kyphotic deformity with the potential of reducibility. In consolidated and fixed fractures, the use of a stent is no longer indicated.
Surgical Technique
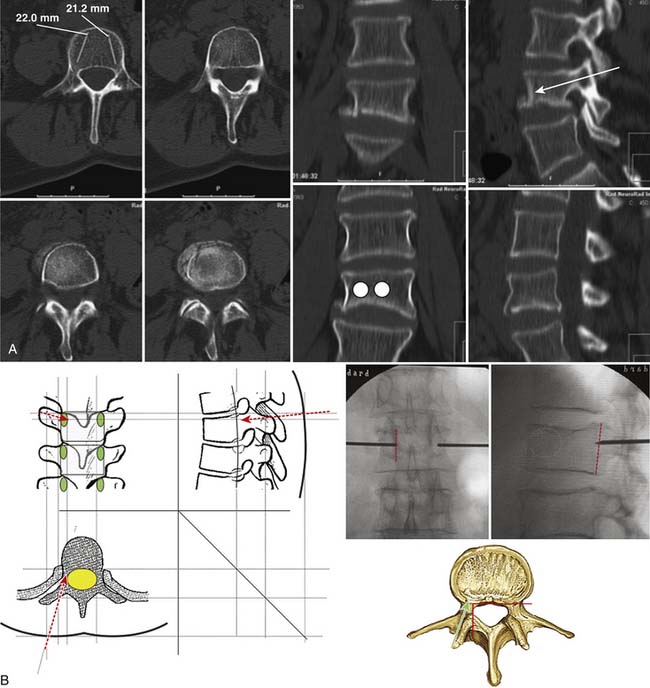
Preferably the procedure is performed under general anesthesia, with the patient placed in hyperextension. Based on the preoperative imaging (either CT scan or MRI and conventional x-rays), the placement of the working cannula and the stent is planned in order to achieve an optimal effect for the fracture reduction (Figure 36-4, A). Intraoperatively this placement is navigated by biplanar C-arm control. The crucial landmarks to be respected are the medial border of the pedicle and the posterior wall of the vertebral body. Depending on the individual anatomical situation, the working cannula is placed transpedicular or parapedicular (Figure 36-4, B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree