Chapter 128 Vertebroplasty and Kyphoplasty
Osteoporotic Vertebral Compression Fractures
Osteoporosis and associated fragility fractures are major threats to the health of aging populations worldwide.1 At 50 to 79 years of age, the incidence of a new vertebral compression fracture (VCF) in Europe is 1% per year in women and 0.6% per year in men, and at 75 to 79 years of age, the incidence is 2.9% per year in women and 1.4% per year in men.2 In the United States, approximately 750,000 people are affected, and only one third receive treatment.3 Despite nonsurgical management, including analgesia, bed rest, physiotherapy, and back bracing, pain sometimes resolves slowly and can persist.4 The resulting vertebral deformity can cause height loss, kyphosis, reduced pulmonary function, and mobility and balance impairment. VCFs are associated with an increased incidence of mortality and morbidity, including back pain, loss of height, kyphotic deformity, increased risk of future fracture, and reduction in quality of life.5 Osteoporotic VCFs are clearly a clinically significant health problem with continuously increasing economic and social ramifications. The National Osteoporosis Foundation predicts that the number of vertebral body compression fractures will double in the next 15 years due to the aging population and increasingly sedentary lifestyles.
Nonsurgical Treatment
In recent rears, various osteoporosis treatments have been developed to reduce the risk of fracture.6,7 As a treatment for VCFs, traditional, nonoperative management includes bedrest, analgesics, and bracing. However, these types of medical management fail to restore spinal alignment, and the lack of mobility itself can result in secondary complications, including worsening osteoporosis, atelectasis, pneumonia, deep vein thrombosis, decubitus ulcer, and pulmonary embolism. An alternative approach is supervised ambulatory mobility by a physiotherapist plus hydrotherapy.8 In one third of patients, severe pain, limited mobility, and poor quality of life persist despite appropriate nonoperative management. Whether the pain has or has not resolved, no patient after a VCF spontaneously achieves a realigned spine, corrected sagittal contour, or restoration of vertebral height.
Surgical Treatment
Historically, the only alternative to nonoperative management for symptomatic vertebral fractures was open surgical decompression (ventral or dorsal decompression and stabilization via internal fixation hardware and bone grafting), and this was usually reserved for those patients with gross spinal deformity or neurologic impairment (<0.5%).9 The reason for this surgical caution was the adverse risk/benefit ratio in this elderly population with poor bone quality and multiple comorbid conditions.
Percutaneous vertebroplasty (PVP) is a minimally invasive method that involves the percutaneous injection of polymethylmethacrylate (PMMA) into a collapsed vertebral body to stabilize the vertebra. Originally developed for osteolytic metastasis, myeloma, and hemangioma, the procedure resulted in quick, effective pain relief and a low complication rate.10–12 PVP is now also increasingly used for the treatment of osteoporotic vertebral fractures.13 However, PVP does not expand the collapsed vertebra, potentially locking the spine in a kyphotic posture. In addition, the PMMA bone filler has associated problems (epidural leakage, thermal necrosis, inability to integrate with bone, handling difficulties, toxicity to patient and operator).14,15
Kyphoplasty is an advanced minimally invasive technique with a number of potential advantages over PVP, including lower risk of cement extravasation and better restoration of vertebral body height.16 A cannula is introduced into the vertebral body, followed by insertion of an inflatable bone tamp, which when deployed, reduces the compression fracture and restores the vertebral body toward its original height, while creating a cavity to be filled with bone cement. The cement augmentation is therefore done with more control into the low-pressure environment of the preformed cavity with viscous, partially cured cement.
Vertebral Augmentation
Percutaneous Vertebroplasty
Background
Percutaneous vertebral augmentation (vertebroplasty, PVP) was first reported by Galibert et al. in 1984 and initially involved the augmentation of the vertebral body with PMMA to treat a hemangioma. PVP was reportedly not performed in the United States until 1994. Originally targeted for osteolytic metastasis, myeloma, and hemangioma, PVP resulted in early appreciable pain relief and a low complication rate.12,17 Its indications subsequently expanded to osteoporotic vertebral collapse with chronic pain, further to include treatment of asymptomatic vertebral collapse and even prophylactic intervention for at-risk vertebral bodies.18 Nevertheless, the treatment of acute fractures in ambulatory patients and prophylactic treatment remain controversial.19 In fact, vertebral augmentation itself is somewhat controversial, with questions concerning a lack of defined indications, expected complications, outcome measures, and the need for long-term follow-up data.14
An open question in PVP is the mechanism of pain relief. The most intuitive explanation involves simple mechanical stabilization of the fracture. However, another possibility is the analgesic result from local chemical, vascular, or thermal effects of PMMA on nerve endings in surrounding tissue.13,20 Supporting this concept is the lack of correlation between cement volume and pain relief.21,22 Further evidence against an effect resulting solely from mechanical stabilization is the fact that PVP typically does not restore lost vertebral body height and therefore does not correct altered biomechanics.19,23
Technique
Injection of opacified PMMA is performed via a transpedicular or paravertebral approach under continuous fluoroscopic guidance to obtain adequate filling and to avoid PMMA leakage. For complex or high-risk cases, CT and fluoroscopic guidance are sometimes combined.10,19 In routine cases, PVP can be performed under local anesthesia with slight sedation in less than 1 hour,1 although general anesthesia is sometimes required because pain may intensify during cement injection.13 Preceding PMMA injection, intraosseous venography is often used to determine the filling pattern and identify sites of potential PMMA leakage (outline the venous drainage pattern, confirm needle placement within the bony trabeculae, and delineate fractures in the bony cortex). However, others have dispensed with routine venography.23
Contraindications to vertebroplasty include coagulopathy, absence of facilities to perform emergency decompressive surgery in the event of a complication, and extreme vertebral collapse (>65–70% reduction in vertebral height).13
Results
Searching the literature with the term percutaneous vertebroplasty in PubMed, there are 766 papers found from 1987 to March 2010.10,12,19,23–37 The first paper on vertebroplasty was published in 1987, treating C2 hemangioma in France.17 Reportedly, pain has been reduced in 70% to 90% of patients.
There are several case control studies published recently. Alvarez et al. conducted a prospective, double-cohort study,38 which consisted of 101 consecutive patients who underwent PVP and 27 patients who refused PVP treatment and were managed conservatively. The results showed that the patients elected for PVP had significantly more pain and functional impairment before the procedure than the patients in the group who did not have PVP (P < .001). The pain, functional, and general health scores of the PVP group were improved from the preoperative mean values (P < .001) in all postoperative periods. Compared with the conservative treatment group, there was a significant difference at 3 months. However, no statistical differences in function were observed between these groups at 6 months and 12 months postoperatively.
Diamond et al. designed a prospective, nonrandomized, “intention-to-treat” 2-year study.39 Participants included 126 consecutive patients (39 men and 87 women, 51 to 95 years of age) with acute osteoporotic vertebral fractures. Of these patients, 88 received treatment by PVP and 38 by conservative therapy. Outcomes in the PVP-treated patients showed 60% reduction in visual analogue pain scores from 20 to 8 (P < .001); a rapid return to normal function (29% improvement in physical functioning from 14 to 18 (P < .001); and lower rates of hospitalization (43% reduction in the mean number of hospital bed-days occupied), which were better than those treated conservatively (P < .001 for the comparison of all variables at 24 hours). Lower pain scores persisted in the vertebroplasty-treated group at 6 weeks (P < .001), but no differences between the two groups were evident at 12 and 24 months. In the vertebroplasty-treated group compared with the control group, the rates of new vertebral fractures (clinically and by radiographic assessment: hazard ratio, 1.13; 95% confidence interval [CI], 0.52–2.46; P = .76) and death (hazard ratio, 1.07; 95% CI, 0.42–2.76; P = .89) showed no significant difference.
Voormolen et al. prospectively assessed the short-term clinical outcome of patients with subacute or chronic painful osteoporotic VCFs treated with PVP compared with optimal pain medication (OPM) (VERTOS study sponsored by Vertos Medical Inc.).40 The investigators randomized the patients into two groups: treatment by PVP or OPM. After 2 weeks, patients from the OPM arm could change to the PVP arm. Patients were evaluated 1 day and 2 weeks after treatment. Their results showed that 18 patients treated with PVP, compared with 16 patients treated with OPM, had a significantly better Visual Analogue Scale (VAS) and used fewer analgesics 1 day after treatment. Two weeks after treatment, the mean VAS was less but not significantly different in patients treated with OPM, whereas these patients used significantly fewer analgesics and had better Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFO) and Roland-Morris Disability (RFD) scores. Scores in the PVP arm were influenced by occurrence of new VCF in two patients. After 2 weeks of OPM, 14 patients requested PVP treatment. All scores, 1 day and 2 weeks after PVP, were significantly better compared with scores during conservative treatment.
In Rousing’s randomized controlled study, 50 patients (41 females) were included from January 2001 until January 2008. Patients with acute (<2 weeks) and subacute (2–8 weeks) osteoporotic fractures were included and randomized to either PVP or conservative treatment. Their results showed reduction in pain from initial visit to 3-month follow-up was comparable in the two groups (P = .33); for approximate VAS, 8.0 to 2.0, intragroup difference was significant (P = .00). Reduction in pain in the PVP group was immediate 12 to 24 hours after the procedure (P = .00). There was no significant difference in the other parameters when comparing the results at inclusion and after 3 months within both groups and between the groups after 3 months. This study found two adjacent fractures in the PVP group and none in the conservative group. The investigators’ conclusions suggested that the majority of patients with acute or subacute painful osteoporotic compression fractures in the spine will recover after a few months of conservative treatment.
Recently, two new studies, reported in the New England Journal of Medicine,41,42 were multicenter, randomized controlled trials that used sham procedure as a control. In the Buchbinder study,41 the number of patients enrolled was 78, and 35 of 38 underwent PVP, and 36 of 40 underwent sham procedure in four Australian centers and completed the 6-month follow-up (91%). At 3 months, the mean reductions in the score for pain in the vertebroplasty and control groups were 2.6 ± 2.9 and 1.9 ± 3.3, respectively. Similar improvements were seen in both groups with respect to pain at night and at rest, physical functioning, quality of life, and perceived improvement. The researchers concluded that there was no beneficial effect of vertebroplasty compared with a sham procedure.
In another randomized, controlled trial, called the Investigational Vertebroplasty Safety and Efficacy Trial (INVEST) by Kallmes et al.,42 68 patients underwent PVP and 63 underwent sham procedure. Both groups had immediate improvement in disability and pain scores after the intervention. Although there was a trend toward a higher rate of clinically meaningful improvement in pain (a 30% decrease from baseline) in the vertebroplasty group (64% vs. 48%, P = .06), the two groups did not differ significantly on any secondary outcome measure at 1 month. The investigators also concluded that improvements in pain and pain-related disability associated with osteoporotic compression fractures in patients treated with vertebroplasty were similar to the improvements in a control group.
Complications
The principal risk of PVP, which involves the forced injection of low-viscosity PMMA cement into the closed space of the collapsed vertebral body, is cement extravasation. Extravasation rates are as high as 65% when cement is used to treat osteoporotic fractures.12,30 The likelihood is greater when using cement with a liquid rather than paste consistency or with higher PMMA volume.27 However, in most settings, the majority of extravasations have no clinical relevance, at least in the short term.23
The consequence of an extravasation depends on its location. In epidural or foraminal extravasation, nerve root compression and radiculopathy is the major risk. This occurred in 11 of 274 patients (4%) treated by Deramond.10 Three of those patients required surgical nerve root decompression. Others have been described with a 5% rate of radiculopathy, as well.9,21,43 Extravasation into perivertebral veins can cause cement embolism to the lungs; deaths attributed to cement embolism have been documented. However, two reported deaths attributed to pulmonary embolism were believed to be unrelated to the procedure; no cement material was detected by chest radiograph of the first patient,13,44 and the second pulmonary embolism arose from deep venous lower extremity thrombosis.10 On the other hand, extravasation into adjacent discs or paravertebral tissue, although common, generally produces no patient symptoms and carries little clinical significance; many such extravasations can be avoided by careful needle positioning.10
Other operative and long-term complications of PVP are specific to PMMA as a filler.18,23,45 The physician may work with PMMA in large batches to keep it liquid and to extend the working time for vertebroplasty. However, its high polymerization temperature (86–107°C within cement core)46 can damage adjacent tissue, including the spinal cord and nerve roots,15 leading to an inflammatory reaction and transitory exacerbation of pain.13 When injecting PMMA monomer, physician vigilance and caution are required. Absorption of PMMA monomer during the injection can induce hypotension by virtue of its cardiotoxic and dysrhythmogenic properties.47 Keeping in mind that placing a material in the spine affords proximity and access to the chest and the heart, vertebral augmentation with PMMA demands meticulous attention to technique.
Overall, the risk of complications that carry clinical significance following PVP for osteoporotic vertebral fracture is thought to be 1% to 3%, and most potential complications can be avoided with good technique.10
Kyphoplasty
Background
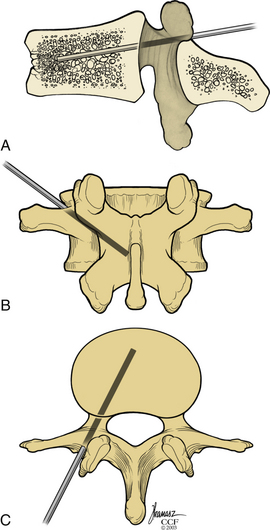
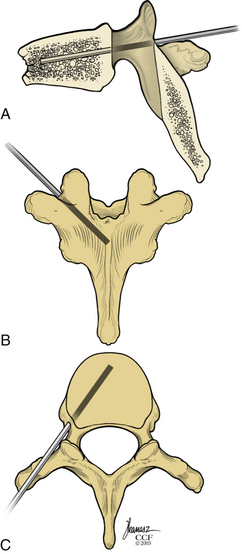
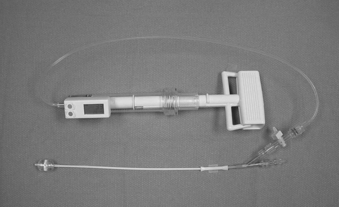
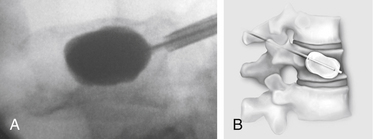
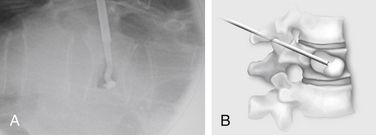
Kyphoplasty is an advanced surgical technique having evolved from a marriage of vertebroplasty with balloon angioplasty. It has a number of potential advantages, including lower risk of cement extravasation and better restoration of vertebral body height. A cannula is introduced into the vertebral body, via a transpedicular (Fig. 128-1) or extrapedicular route (Fig. 128-2), followed by insertion of an inflatable bone tamp (IBT; Fig. 128-3), which when deployed, reduces the compression fracture and restores the vertebral body toward its original height. This then creates a cavity to be filled with bone cement. The cement augmentation can now be completed with more control into the low-pressure environment of the preformed cavity with viscous, partially cured cement. Using a cannula for bone filler with a steel stylet as a plunger enables the operator to apply cement at considerably higher viscosity than is possible with injection through a 5-mL syringe and 11-gauge needle. Both the higher cement viscosity and controlled fill reduce the risk of cement extravasation. Filling is performed under continuous lateral fluoroscopic guidance similar to vertebroplasty. The procedure can be performed under general anesthesia or local anesthesia with intravenous sedation, and most of the patients are able to return home the same day of procedure.
Technique
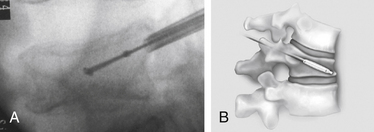
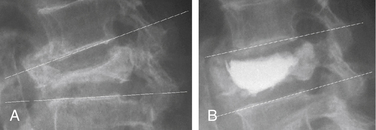
With the patient under general or local anesthesia in the prone position on a radiolucent spinal frame, two C-arms are positioned for anteroposterior and lateral fluoroscopic images. Once positioned the C-arms and patient are not moved, to ensure repeatable images throughout the case. Two 3-mm incisions are made at the vertebral level, parallel to the pedicles in both planes. Then a guidewire or biopsy needle is advanced into the vertebral body via a transpedicular or extrapedicular approach, depending on the fracture configuration and the patient’s anatomy. The guidewire is then exchanged for the working cannula using a series of obturators. Once the working cannula is positioned, the surgeon reams out a corridor to accommodate the IBT and positions the IBT under the collapsed end plate (Fig. 128-4). To deploy the IBT, inflation proceeds slowly under fluoroscopy until maximum fracture reduction is achieved or the balloon reaches a cortical wall (Fig. 128-5). At this point, the surgeon deflates and removes the IBT, mixes the cement, prefills the cement cannulae, and allows the cement to partially cure in the cement cannulae. Once partially cured, PMMA is slowly extruded into the vertebral body through each pedicle under continuous lateral fluoroscopic guidance (Fig. 128-6). This technique permits a controlled fill. In most instances, the volume of cement can slightly exceed that of the bone cavity to interdigitate filler from the central bolus with the surrounding bone. Once filling is complete and the cement has hardened, the surgeon removes the cannula and closes the 3-mm incisions.
Results
Our published data from the Cleveland Clinic showed that kyphoplasty provided a safe and effective treatment for pain and disability in patients with vertebral compression fractures secondary to osteoporosis and multiple myeloma.16,48–51 Outcome data were obtained by administering the 36-Item Short Form Health Survey (SF-36) and the VAS for pain rating; in addition, the patients underwent detailed neurologic and radiographic examinations preoperatively and postoperatively. In our experience, there were no clinically significant cement leaks and no perioperative complications attributable to the IBT or tools. Using SF-36 data (preoperative and postoperative), available on more than 210 patients with average follow-up periods of 10.8 months, SF-36 scores improved in every category, statistically significant in all but the General Health modality. Physical function improved from 15.0 to 30.0 (P < .001). Role physical improved from 9.3 to 27.3 (P = .004). Bodily pain improved from 22.0 to 32.0 (P ≤ .001). Vitality improved from 30.0 to 40.0 (P ≤ .001). Social function improved from 37.5 to 50.0 (P ≤ .001). Role emotional improved from 33.3 to 66.7 (P = .39). Mental health improved from 64.0 to 72.0 (P < .001). General health was unchanged from 52.0 to 55.0 (P = .051). The VAS scores improved from a preoperative level of 7.0 to an initial postoperative level of 3.2 (P < .0001). At the last follow-up examination, the value remained unchanged at 3.4 (P < .0001).
Ledlie et al. reported functional and radiographic outcomes in the first 117 consecutive patients with 151 fractures.52 This report focused on the results for the subset of 77 patients completing follow-up. With regard to pain, rated by the patient using a 10-point VAS, the mean pain score decreased from 8.9 ± 1.5 before surgery to 2.8 ± 2.9 at 1 week postoperatively; this value remained low, at 1.5 ± 1.8 at 2 years postoperatively. The proportion of patients fully ambulatory increased from 45% before surgery to 85% at 1 week postoperatively and 88% at 2 years.
Garfin et al. reported clinical results of a total of 155 subjects with 214 VCFs who underwent balloon kyphoplasty at 19 study centers from August 2000 to June 2001.53 Mean pain ratings decreased from 15.0 (maximum score, 20) before surgery to 6.0 within 7 days after kyphoplasty (P < .001), a 60% reduction, and remained decreased throughout follow-up to 24 months. The mean number of days of the previous 28 days spent in bed decreased from 8.8 at baseline to 1.9, 2.2, 0.7, and 1.4 at 1, 3, 12, and 24 months, respectively, after kyphoplasty.
Wardlaw et al. reported the results of their randomized controlled trial at 21 sites in eight countries.54 In this report, 300 patients randomly assigned by a computer-generated sequence to receive kyphoplasty treatment (n = 149) or nonsurgical care (n = 151). Among them, 138 participants in the kyphoplasty group and 128 controls completed follow-up at 1 month. By use of repeated measures mixed effects modeling, all 300 randomized participants were included in the analysis. The mean SF-36 physical component summary score improved by 7.2 points (95% CI, 5.7–8.8), from 26.0 at baseline to 33.4 at 1 month, in the kyphoplasty group, and by 2.0 points (95% CI, 0.4–3.6), from 25.5 to 27.4, in the nonsurgical group (difference between groups 5.2 points, 95% CI, 2.9–7.4; P < .0001). The frequency of adverse events did not differ between groups. These results suggested that balloon kyphoplasty is an effective and safe procedure for patients with acute vertebral fractures and helps inform decisions regarding its use as an early treatment option.
In addition to good clinical results, height restoration by kyphoplasty has been reported in several studies (Fig. 128-7). Our initial results showed height restoration in 70% of 70 fractured vertebrae treated with kyphoplasty.16 In patients in whom the vertebral fractures were reduced by kyphoplasty, vertebral height increased by a mean of 46.8%.
Ledlie et al. reported their radiographic measurement results for ventral and midline points of the fractured vertebrae using the two nearest normal vertebrae as reference points.55 Pairs of preoperative and 2-year follow-up radiographs for 85 treated fractures were evaluated for vertebral height measurement. Mean preoperative ventral height (Ha), midheight (Hm), and dorsal height (Hp) were 61.3% ± 23.8%, 61.0% ± 20.1%, and 86.5% ± 18.4%, respectively. Compared to preoperative heights, mean Ha, Hm, and Hp were significantly higher (P < .001) at all postoperative intervals. Following kyphoplasty (1–6 weeks), mean Ha, Hm, and Hp were 81.2% ± 20.9%, 86.9% ± 17.9%, and 95.1% ± 10.1%, respectively. At 2-year follow-up, mean Ha, Hm, and Hp were 80.9% ± 19.8%, 88.1% ± 16.6%, and 91.4% ± 12.8%, respectively. There was no correlation between height increase and patient age, gender, fracture level, or fracture age.52
Garfin et al. reported the results of midline height restoration rates. The mean preoperative midvertebral height was 65% of the predicted height. Eighty-two percent of patients had at least 10% lost height restored during the pretreatment and post-treatment interval. The mean percent midvertebral lost height restored was 32% overall and 44% in those with measurable height restoration.53
Complications
Many kyphoplasty studies provided details on the number of cement leakage complications. In a meta-analysis, Taylor showed that a total of 189 (9%) cement leakages were reported in 2239 vertebrae that underwent kyphoplasty.56 This corresponds to 81 cement leaks per 1000 fractures undergoing kyphoplasty per year. One leak (0.001%) was reported by Majd57 to be symptomatic L1 radiculopathy. A few cases also reported inappropriate cement injection and needle placement in the early phase.58 In our series of patients,16,49 cement extravasation was seen in less than 10% of cases. No problems were identified clinically as a result of these extravasations immediately after surgery or at final follow-up. In one patient, a myocardial infarction occurred as a result of fluid overload during the procedure.
Ledlie et al. reported three complications in their series.52 Two weeks after kyphoplasty, a patient with a history of deep vein thrombosis (no evidence of PMMA leakage to the lungs by CT) had a pulmonary embolism. A second patient with preexisting metastatic, cardiac, vascular, severe chronic obstructive pulmonary disease required mechanical ventilation and subsequently died 5 days postoperatively. A third patient had perioperative confusion and generalized weakness that gradually resolved (negative brain CT and neurologic workup). No complication was related to the kyphoplasty technique. Minor cement extravasations were observed in 11.3% (17/151) of treated fractures, but none of the leaks was associated with any clinical consequence.
Garfin et al. also reported that the extravasation of PMMA outside the vertebral body occurred in 21/214 (10%) of treated levels.53 All PMMA extravasations were asymptomatic, the cement remained in the immediate area of the treated vertebrae, and no medical or surgical intervention was required to remove the extravasated PMMA.
Phillips et al. reported that asymptomatic cement leaks were observed in 6 of 61 vertebral fractures (9.8%).59 In this series as well, there were no clinical consequences attributable to the bone tamp or cement deposition.
Two papers reported “redo” vertebral augmentation in case the previous vertebral segmentation failed to relieve pain.60,61 A report by Gaughen et al. concerned six patients whose initial vertebroplasty resulted in substantial improvement in pain. These six patients developed recurrent pain between 8 days and 167 days after initial vertebroplasty and underwent “redo” vertebroplasty. After repeat vertebroplasty, five of the six patients reported a reduction of at least 3 points in their pain rating, with a mean reduction of 6.5 points and a mean postoperative pain level of 3.5 points (11-point scale). Four of six patients reported impaired mobility before repeat vertebroplasty, and all four demonstrated a postoperative improvement in mobility. The mean increase in mobility was 1.50 points, and the mean postoperative mobility impairment was 0.25 points (5-point scale). The investigators concluded that the clinical outcomes of the patients within this case series suggest that repeat percutaneous vertebroplasty performed at previously treated vertebral levels for recurrent pain offers therapeutic benefit. Although the repeating of this procedure is technically demanding, “redo” vertebral augmentation could be performed over a previously treated kyphoplasty or vertebroplasty.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree