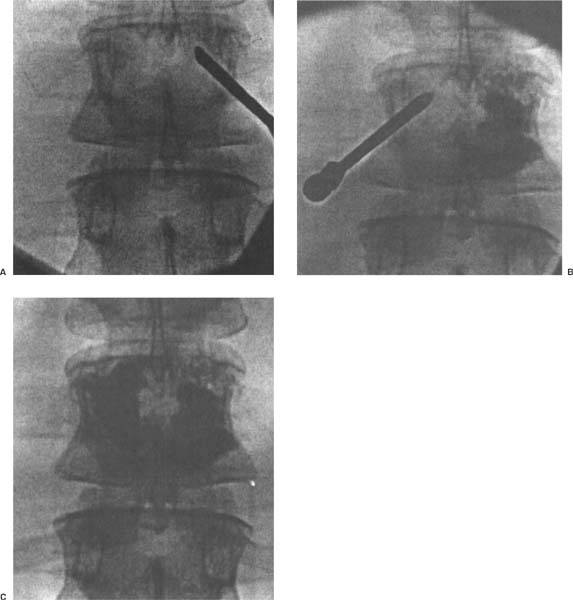
16 Vertebroplasty and Kyphoplasty in the Treatment of Osteoporotic Vertebral Compression Fractures The goals of surgical intervention for osteoporotic vertebral compression fractures include the prevention of neurologic compromise, instability, unacceptable deformity, and pain from deformity or nonunion. 1. History of severe back pain with or without deformity 2. Anteroposterior (AP) and lateral x-ray showing compression fractures either single or multiple 3. Positive MRI and/or bone scan. The procedure is indicated for severe incapacitating back pain as a result of acute or progressive osteoporotic vertebral compression fractures. It is recommended in patients unable to tolerate any further immobilization, not responding to nonoperative management. The procedure has been used for up to three or more acute fractures at a time. 1. Uncorrectable coagulopathy. 2. Breach in the posterior cortex. 3. Retropulsion with canal compromise. 4. Infection. 5. Significant neurologic symptoms. 6. Minor radicular complaints are not a contraindication, but should prompt the search for bone, disc, or tumor compressing the nerve root. 7. Acute traumatic nonosteoporotic fractures should not be treated with methylmethacrylate because it can interfere with bone healing. 1. Inability to tolerate lying prone, or general anesthetic for 1 to 2 hours 2. Acute fractures less than 2 weeks Polymethylmethacrylate (PMMA) will interfere with fracture healing as above, but cortical defects will allow the liquid PMMA to leak from the confines of the vertebral body. Difficulty can arise with severe compression fractures, especially when the superior end plate comes to rest well below the level of the pedicles. Small pedicles are not a contraindication, as long as the surgeon is familiar and comfortable with the extrapedicular approach along the superolateral aspect of the pedicle, avoiding neurologic, vascular, or pulmonary injury. The patient should be able to withstand a general anesthetic, but seduction and local anaesthetic have been used. Patients should not be receiving any anticoagulation prior to the procedure. Magnetic resonance imaging (MRI) is used to diagnose an acute fracture, with an increase in signal intensity at the fracture on T2-weighted images. It also gives information regarding canal compromise, neural impingement, and possibility of tumor. Bone scan is also helpful in subacute fractures. As described by the original inventors in 1984, the technique of percutaneous vertebroplasty involves the injection of liquid PMMA into the vertebral body under pressure via needles placed through the skin posteriorly under fluoroscopic guidance using AP, lateral, or oblique views. Patients are administered a general or local anesthetic. Antibiotics are given only if the patient is immunocompromised. A standard sterile surgical field with gowns and drapes is used. Using fluoroscopic images, a 10-gauge needle with trocar [e.g., Jamshidi biopsy needle (Manan Medical, Northbrook, IL)] is directed into the vertebral body from a posterolateral approach. Biplanar fluoroscopy is used if available, as it decreases operative time significantly. The needle is passed in a transpedicular fashion aiming for a paracentral location within the anterior half of the body centrum. The transpedicular approach is optimal because it will eliminate potential problems with cement leakage along the needle track. Penetration of the inferior or medial cortex of the pedicle is dangerous and poses a threat to neurologic structures. Thus, if the pedicle is too small in diameter, an extrapedicular approach along the superolateral aspect of the pedicle is advocated. The needle is then introduced into the vertebral body at the junction of the pedicle and posterior cortex, avoiding damage to neural structures. Care must be taken to avoid rib fractures when attempting to advance the needle, as it can be difficult at times due to hard cortical bone. PMMA is prepared in the usual fashion, with the addition of 1 g of tantalum or tungsten powder for better localization of the cement on fluoroscopy during injection. Jensen et al. (1997) suggest the addition of 1.2 g of tobramycin in immunocompromised patients. When the PMMA reaches a semiliquid paste consistency (low viscosity), it is injected through the needle with the aid of small syringes attached to the needle via a Leur-Lok mechanism. Injection is performed slowly under fluoroscopic guidance and stopped when the PMMA reaches the posterior cortex, or there is extravasation into the disc space or paravertebral tissues. As long as the PMMA is contained within the vertebral body, thermal injury to neural structures has not been reported. The needle and trocar are left in place until the cement has hardened, and then they are withdrawn. The volume injected varies considerably from 2.5 to 11.0 cc, and averages 7.0 cc. If less than half of the vertebral body is filled with cement, the procedure is repeated through the contralateral side. Patients are kept flat for 4 hours, at which point PMMA has reached approximately 90 % of its maximal strength and then they are permitted activity as tolerated. Patients are discharged after overnight observation, although Jensen has reported that the procedure may be performed on an outpatient basis in healthy patients (Fig. 16–1). Incidence of clinically significant complications ranges from 0 to 12 %, average 5 %. 1. Because the PMMA is injected under pressure, cement extravasation can cause spinal cord or nerve root injury, pulmonary embolism, or further retropulsion of bony fragments into the canal. 2. Complication rate increased with tumor or herniated nucleus pulposus. 3. If compression has resulted in loss of height to less than one-third the original height, especially if the superior end plate is below the level of the pedicles, insertion of the needle can be very difficult and increase the complication rate. For these fractures, CT-guided vertebroplasty may be safer 4. Overuse of fluoro-imaging results in excessive radiation exposure. Within 24 hours, 90 to 95 % of patients have moderate to complete relief of pain. 1. Same as for vertrebroplasty 2. To correct sagittal imbalance resulting from a spinal fracture Same as for vertebroplasty. Same as for vertebroplasty. The same patient population and caveats that apply to vertebroplasty apply to kyphoplasty. The one exception being acute fractures, where it is hoped kyphoplasty offers its greatest benefit with lower potential complications. Kyphoplasty is not recommended for metastatic or hemangiomatous lesions of the spine, but it is indicated in multiple myeloma. Figure 16–1
Vertebroplasty
Goals of Surgical Treatment
Diagnosis
Indications
Contraindications
Relative Contraindications
Preoperative Evaluation and Selection of Patients
Procedure
Complications
Results
Kyphoplasty
Goals of Surgical Treatment
Diagnosis
Indications for Surgery
Indications and Contraindications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree