Chapter 13 Vestibular rehabilitation
Introduction
This chapter will focus on the assessment and treatment of patients who have a primary problem in the vestibular system. Vestibular dysfunction is characterized by a number of signs and symptoms, including vertigo, gait and balance impairment, nausea and nystagmus (Table 13.1).
Table 13.1 Signs and symptoms of vestibular disorders
| Primary symptoms and signs | Associated problems |
|---|---|
| Vertigo | Neck and back pain |
| Dizziness/light-headedness | Physical deconditioning |
| Nausea and vomiting | Agoraphobia |
| Oscillopsia | Hyperventilation |
| Nystagmus | Falls |
| Disequilibrium/impaired balance | Hearing loss/tinnitus |
| Panic/anxiety | |
| Gait abnormality | |
| Fatigue |
Patients with such dysfunction present the physiotherapist with specific problems and require specialized assessment and treatment techniques, collectively referred to as vestibular rehabilitation. Vestibular rehabilitation has its roots in the empirical work of Cawthorne and Cooksey who, in the 1940s, first documented the important role of exercise in recovery after a vestibular injury (Cooksey, 1945).
There is now a moderately strong evidence base to support the role of physiotherapy in the management of patients with vestibular disorders (Hillier & Holohan, 2007; Hilton & Pinder, 2004) and vestibular rehabilitation is recognized as a specialist area within physiotherapy.
Vertigo is defined as the sensation of motion when no motion is occurring relative to the Earth’s gravity (Monsell et al., 1997). The sensation can be of the patient moving in relation to the environment or the environment moving in relation to the patient. It is generally accepted that true vertigo involves a spinning sensation and usually indicates inner-ear pathology (Blakley & Goebel, 2001). The word ‘dizziness’ is used to describe non-rotatory vertigo. These definitions should be considered when taking the patient’s history as they will give clues to the underlying pathology.
Incidence and prevalence of dizziness and balance disorders
The prevalence of dizziness has been estimated to be one in five in the 18–64 age group with 50% of these reporting postural unsteadiness (Yardley et al., 1998b). Prevalence rises to one in three in the over-65s (Colledge et al., 1994) and dizziness is the most common complaint of patients presenting to primary care in those aged over 75 (Sloane, 1989). However, approximately 40% of patients with a complaint of dizziness do not consult their general practitioner, demonstrating a probable underestimation of the problem (Yardley et al., 1998b). There is a very low prevalence of dizziness in the under-25s and women are more likely to experience dizziness. Dizziness rarely results in hospitalization and the majority of patients are managed at primary care level with medication (Sloane, 1989).
Normal anatomy and physiology
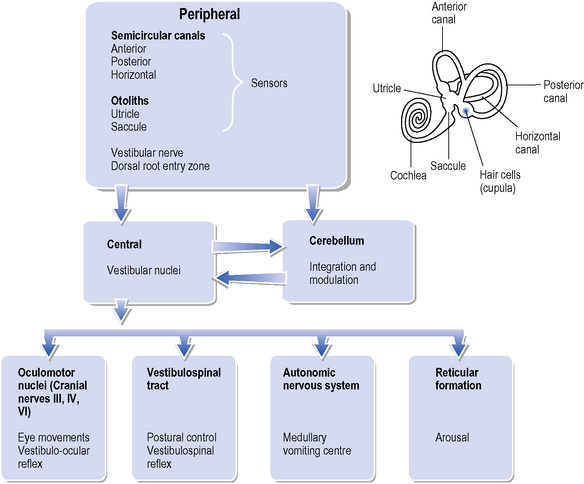
The anatomy and physiology of the vestibular system are extremely complex and the reader is referred to Cohen (1999) and (Schubert & Minor, 2004) for a detailed description. A brief organizational overview is shown in Figure 13.1. The vestibular system has both sensory and motor functions and is generally divided into peripheral and central components. The peripheral system consists of the vestibular end organ and the vestibular nerve up to and including the dorsal root entry zone. The central system includes the vestibular nuclei in the brainstem and their central connections.
Peripheral vestibular system
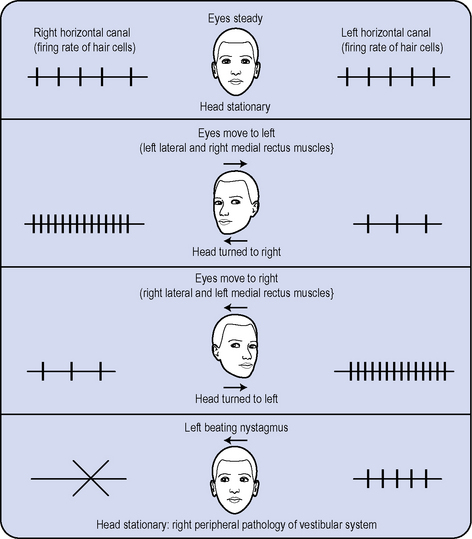
The vestibular end organ includes the semicircular canals (SCC) and the otoliths (utricle and saccule). There are three SCCs on each side (horizontal, anterior and posterior) and they are oriented at approximately 90° angles to each other (Figure 13.1). Each canal is coupled functionally with a canal in the opposite end organ, i.e. both horizontal canals are coupled, as are the left anterior and right posterior, and the right posterior and left anterior canals. Specialized sensors known as hair cells are located in the semicircular canals in a region known as the cupula (Figure 13.1) and respond to angular velocity of head movement in different planes. Each canal responds best to movement in its own plane. For example, if the head turns to the right, the hair cells in the right horizontal SCC increase their firing rate and those in the left horizontal SCC decrease their firing rate (Figure 13.2). Thus the central nervous system (CNS) gains information relating to the velocity and direction of head movement.
The peripheral system is a tonically active system, i.e. it always has a certain firing level (about 70–100 spikes per second), which will increase or decrease with head movement. The CNS interprets any asymmetry in the firing rate as movement. This fact is of utmost importance when considering a patient who has loss of vestibular function on one side (i.e. decrease or absence of firing) since there will be a relative increase of firing on the intact side even when the head is not moving (Figure 13.2). This asymmetry and the resultant disturbance in cortical spatial orientation are thought to form the basis of vertigo (Brandt, 2000a). Afferent nerve fibres arising from hair cells collect to form the vestibular nerve, which enters the brain at the pontomedullary junction.
Central vestibular system
The vestibular nerve sends fibres to two main areas: the vestibular nuclei (in the pons and the medulla) and the cerebellum (Figure 13.1). The vestibular nuclei are responsible for integrating information received from the vestibular end organ with that received from other sensory systems and the cerebellum. Vestibular nuclei send fibres to the oculomotor nuclei, vestibulospinal tracts, contralateral vestibular nuclei, reticular formation, thalamus, cerebellum, autonomic nervous system and the cortex. The parietal and insular areas of the cortex appear to be a specialized vestibular area (Brandt et al., 2002). The symptoms of nausea, vomiting and anxiety associated with vestibular disorders are thought to be a result of abnormal activation of the autonomic and reticular pathways respectively (Figure 13.1).
Classification and causes of vestibular disorders
Vestibular disorders are classified anatomically into peripheral or central, depending on which area the pathology affects. Common peripheral and central vestibular disorders are shown in Table 13.2. It is important to note that dizziness is not always caused by pathology affecting the vestibular system; there may be many other causes, including postural hypotension, cardiac disorders, psychiatric disorders and hyperventilation, and these should be evaluated prior to referral to physiotherapy. The exact cause of dizziness frequently remains uncertain and a trial of vestibular rehabilitation may be suggested in the absence of a specific diagnosis. The pathologies of disorders that can affect the central vestibular system (particularly cerebrovascular accidents, traumatic brain injury and multiple sclerosis) are considered in other chapters.
Table 13.2 Peripheral and central vestibular disorders
| Peripheral | Central |
|---|---|
| Viral – vestibular neuritis/labyrinthitis | Ischaemia, e.g. lateral medullary syndrome (Wallenburg’s syndrome) |
| Benign paroxysmal positional vertigo (BPPV) | |
| Perilymph fistula | Vertebrobasilar insufficiency |
| Ménière’s disease | Infection |
| Vascular occlusion | Head injury |
| Iatrogenic (ototoxic drugs, surgery) | Degenerative disease, e.g. multiple sclerosis |
| Head injury | Friedreich’s ataxia |
| Acoustic neuromas (may have a central component) | Base-of-skull abnormalities, e.g. Arnold–Chiari malformation |
| Tumours of the cerebellopontine angle | |
| Drugs | |
| Epilepsy | |
| Migraine |
Peripheral disorders
Vestibular neuritis
This condition is also called neuronitis and is a common peripheral vestibular problem thought to be caused by a virus. It results in hair cell loss and unilateral vestibular paresis (or hypofunction). Patients present with an acute onset of vertigo, nausea and vomiting that is severely incapacitating and worsened by head and eye movements. On examination a spontaneous horizontal nystagmus can be seen, the fast phase of which beats away from the involved side. This is due to the asymmetrical tonic firing of the vestibular nerves (Figure 13.2). Balance and gait abnormalities are also evident. Hearing is not generally affected; if it is, the condition is called labyrinthitis. These symptoms generally resolve over a period of 2–6 weeks.
Benign paroxysmal positional vertigo
Benign paroxysmal positional vertigo (BPPV) is the commonest cause of vertigo in peripheral vestibular disorders. It has a lifetime prevalence of 2.4% (Marom et al., 2009) and is more common in females (Baloh et al., 1987). Its aetiology is unknown in many cases but it can occur as a result of an earlier vestibular neuritis or head trauma. The name encompasses the following associated features:
BPPV is thought to be caused by detached utricular otoconia entering one of the SCCs and either floating free in the canal (canalithiasis) or adhering to the cupula (cupulolithiasis; Epley, 1980). This has the effect of making the SCC with the displaced otoconia in it responsive to gravity when normally it is not. The SCCs usually respond to head movement in their respective planes and increase or decrease their firing rate during head movement, returning to normal tonic firing level when the head has stopped moving. However, the displaced otoconia are heavier, continue to move in the canal and stimulate the hair cells in the canal to continue firing. The central vestibular system interprets this as further movement and generates a VOR for that canal, and the patient develops nystagmus and vertigo.
This nystagmus, following movement into the provoking position, has a latency of 1–50 seconds, is generally transient in nature (it stops when the otoconia come to a resting position) and is most commonly torsional towards the affected ear. If the patient repeatedly moves into the provoking position the vertigo and nystagmus will decrease due to habituation of the response (Baloh et al., 1987).
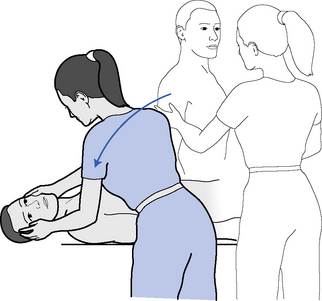
The diagnosis of BPPV is generally made using the Hallpike–Dix manoeuvre (Figure 13.3, Table 13.3) in which the head is moved into a provocative position. BPPV is most commonly caused by canalithiasis affecting the posterior SCC, but can also affect the anterior and, very rarely, the horizontal canal (Baloh et al., 1993; De la Meilleure et al., 1996).
Table 13.3 Oculomotor and positional tests of the vestibular patient
| Oculomotor examination | Details and expected findings |
|---|---|
| Spontaneous nystagmus Room light (visual fixation) Frenzel lenses (no visual fixation) | For the first four tests the patient is asked to hold the head stationary. Patient looks straight ahead. The eyes are observed for a nystagmus and the direction is noted. Frenzel lenses both remove visual fixation and magnify the eyes (Figure 13. 9). Nystagmus due to an acute unilateral peripheral vestibular disorder will have a fast phase away from the side of the lesion (Figure 13.2) and will be suppressed by visual fixation (i.e. focusing on something). Thus it is unlikely to be seen without Frenzel Lenses. |
| Gaze evoked nystagmus* | Patient is asked to watch examiner’s finger as it moves from left to right (about 30°) stopping at 30°. Normally the eyes will remain steady on the examiner’s finger. If abnormal the eyes will make saccadic movements in an effort to remain on the examiner’s finger. |
| Smooth pursuit* | Ability to track examiners moving finger, from side to side and up and down with the eyes when the head is stationary. Normally the eyes make smooth movements, abnormalities include slow or saccadic movements of the eyes. |
| Saccades* | The examiner holds two objects and asks the patient to look from one to the other (left to right, right to left, up to down and down to up starting from a mid position and moving about 30°). An abnormal response would be that the eyes over or under shoot the target |
| VOR cancellation* | Ability to suppress the vestibulo-ocular reflex and move the eyes in phase with the head. Patient is asked to follow a moving target as the examiner moves the head in the same direction. |
| Vestibulo-Ocular reflex- Halmagyi head thrust test (Halmagyi & Curthoys, 1988; Halmagyi et al., 2001) Slow head movement Fast head movement | A normal VOR is when the eyes are able to stay fixated on a stationary target when the head moves. The patient is asked to keep their eyes steady on a target (usually the examiner’s nose) whilst the examiner moves patient’s head in a small range of movement (about 30°) from side to side and then up and down slowly. This is repeated with faster movements of the head. Patients with vestibular deficits are unable to keep the eyes steady and may use a saccadic movement to return their eyes to the target. For example in right vestibular hypofunction, if the head is moved to the right, the eyes may make a saccadic movement to the left. Abnormalities are more often seen with faster head movements. |
| Fukuda Step Test (Fukuda, 1959) | Also known as Unterberger’s test. The patient is asked to close their eyes and march with high steps on the spot for 50 steps which they count themselves. The examiner stands behind the patient to ensure patient safety. The patient is observed for rotation and/or progression forwards from the start position. It is considered abnormal if the patient rotates more than 30° or progresses forwards more than 50 cm |
| Dyanmic Visual Acuity (Tian et al., 2002) | Tests visual acuity when the head is moving and is an indicator of VOR function. The patient is first asked to read a Snellen chart and static visual acuity is ascertained. The examiner then moves the head from side to side at a frequency of 1-2hz (using a metronome) and the patient then is asked to read a Snellen chart again. If visual acuity changes by more than 3 lines, acuity during head movement is considered impaired. |
| Positional tests Hallpike-Dix test (Figure 13.3) | The patient is long sitting on plinth with eyes open. The head is turned 45° to the side that is being tested. The patient is brought quickly into a lying position by the examiner until the cervical spine is in 30° of extension. This position is maintained for 50 seconds and the presence, duration and direction of nystagmus is noted. Symptoms are also noted. This test is diagnostic for BPPV. A positive finding is nystagmus (most commonly torsional towards the tested side) that comes on with a latency, may stay or disappear, and attenuates with repeated testing. |
* Abnormality detected during these tests is indicative of central nervous system pathology.
Ménière’s disease
The cause of Ménière’s disease is an increase in volume and a problem with absorption of the endolymph (one of the fluids in the inner ear). This results in dilation of the endolymphatic spaces (endolymphatic hydrops). This happens episodically and an attack is characterized by a complaint of a fullness in the ear, reduction of hearing and tinnitus (a ringing sound in the ear). This is followed by vertigo, vomiting and postural imbalance and nystagmus is observed. The episodes may last from 30 minutes to 72 hours and then the patient gradually improves. Episodes are generally managed with medication, diet and rest, but in severe cases surgery may be indicated (see below). Although it was formerly thought vestibular rehabilitation was not indicated in patients with Ménière’s, as attacks remit spontaneously, there is now some evidence to suggest it has a role in those patients who present with complaints of impaired balance between attacks (Gottshall et al., 2005).
Recovery from vestibular pathology: vestibular compensation
Research has shown that plastic changes occur in the CNS in response to peripheral vestibular pathology and these changes are responsible for vestibular compensation (Curthoys, 2000; Zee, 2000). Three processes are thought to contribute:
The reasons why some patients fail to compensate are not always clear, but may be a result of abnormality in the CNS, visual, somatosensory or musculoskeletal systems. Animal studies have shown that compensation is delayed by immobilization, reduced or absent visual inputs and is promoted by exercise (Courjon et al., 1977; Lacour et al., 1997). It is thought that the CNS needs to experience the error signals in order for vestibular compensation to occur. Certain medications, including those used in the treatment of vestibular problems, can delay compensation (Zee, 1985). An intact CNS is vitally important for the process of vestibular compensation and thus patients with central vestibular problems will have a slower and more incomplete recovery (Rudge & Chambers, 1982). In bilateral vestibular loss, there may be no remaining VOR function with which to compensate, so the process of sensory substitution plays a major role in the recovery of these patients and recovery will always be incomplete.
Medical and surgical management
Diagnosis/investigations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree