Video-Assisted ALIF with Cage and Anterior Plate Fixation for L5-S1 Spondylolisthesis
S. Aunoble
D. Hoste
B. Bley
Y. Basso
L. Villet
F. Liquois
P. Donkersloot
J. C. Le Huec
Anterior lumbar interbody fusion (ALIF) has become a widespread technique since the 1990s, when metallic cages were first used for interbody fusion (1). In comparison with the use of autologous bone grafts (2,3,4,5,6), the use of interbody fusion cages has improved fusion rates and clinical results (7). The anterior approach prevents epidural fibrosis and posterior muscle damage, and it can help prevent adjacent level disease after spinal fusion (8).
However, an increased rate of pseudarthrosis is associated with the use of a stand-alone anterior lumbar interbody fusion technique because the cage provides insufficient initial stability. In those cases, posterior stabilization can be added (9,10,11,12). Most certainly in patients with isthmic spondylolisthesis, complementary posterior fixation can be helpful in achieving fusion. The combination of anterior plate fixation and an interbody fusion cage provides better vertebral stabilization (13). The latter approach permits a single-stage surgery with improved fusion rates.
We report on the clinical and radiographic results in a series of 20 patients with an isthmic spondylolisthesis at the level L5-S1 of Grade 0 or 1 according to the classification of Meyerding. All patients were operated by means of an anterior retroperitoneal video-assisted approach (14). In every case, we used an interbody fusion cage and the Pyramid anterior plate fixation (Medtronic USA).
MATERIALS AND METHODS
We performed a prospective study on 20 patients, who underwent anterior lumbar interbody fusion at spinal level L5-S1. Patients were operated between February 2001 and March 2003. The Medtronic Sofamor Danek (Memphis, TN, USA) materials: Pyramid anterior plate, combined in 15 cases with a Union cage and in five cases with a Lordotec cage. Autologous bone graft from the iliac crest was used in all cases.
The patients were 11 women and nine men with a mean age of 44 years and 2 months (range 31 to 65 years). All suffered from single-level L5-S1 degenerative disc disease. They complained of chronic, severe low back pain resistant to conservative treatment for more than 6 months. All patients had an isthmic spondylolisthesis at the level L5-S1.
Two patients had a medical history of previous posterior decompressive spine surgery, and one patient had a L4-S1 posterior arthrodesis with persistent discogenic pain assessed by a positive provocative discography at the L5-S1 level only. Preoperative magnetic
resonance imaging (MRI) revealed Modic type 0 changes in two cases, type 1 in 13 cases, and type 2 in five cases.
resonance imaging (MRI) revealed Modic type 0 changes in two cases, type 1 in 13 cases, and type 2 in five cases.
Clinical and Radiographic Evaluation Criteria
Clinical data were collected preoperatively, at 6 weeks and at the 6-, 12-, and 24-month postoperative follow-up. Complication analysis includes the intraoperative and immediate postoperative period.
Clinical results were measured by means of the Oswestry Disability Index (ODI) and the visual analogue scale (VAS) for back and leg pain. The appearance of sacroiliac joint pain or posterior facet pain was registered.
At each visit, we obtained plain frontal and lateral radiographs at the L5-S1 level and lateral radiographs of the entire lumbar spine. Fusion was defined as the absence of a peri-implant lucency surpassing more than 50% of the total implant surface, a translation equal to or less than 3 mm, and the absence of implant breakage. Measurements of the L5-S1 intervertebral disc height led to the detection of cage subsidence into the vertebral endplates. Lumbar lordosis at the L1-S1 and L5-S1 level and sacral slope were found, leading to a global lumbar sagittal balance analysis.
Patients were operated by two surgeons (LH and PD). All measurements were performed by an independent surgeon. Radiographs were analyzed and measured by means of a graduated goniometer.
Clinical and radiographic information was stored using the File Marker Pro 5/0 program. The aortocaval bifurcation positioning and feasibility of an anterior approach were indicated by means of angio magnetic resonance imaging (MRI) performed in every patient.
In the procedure, patients are placed in supine position with slight hyperlordosis and the legs spread. Autologous bone harvesting is performed through a mini-incision on the left iliac crest.
A horizontal, left paramedial incision of about 8 cm is chosen. The anterior rectus sheath is split vertically, and the muscle is retracted laterally. The rectus muscle is freed from his posterior sheet. The retroperitoneal space is then reached between the fascia transversalis and the peritoneum. The superior anterior iliac spine is palpated. The psoas muscle is identified and retracted. The peritoneal sac is bluntly pushed aside allowing the surgeon to progressively clear out the retroperitoneal working space. A 10-mm cold-light endoscope coupled to a Tri-CCD screen is put in place. Through direct visual and endoscopic control, the left iliac artery and vein are located and dissected. Identification of the left ureter, which is left to the posterior peritoneal sheath, is performed. The peritoneum is further bluntly dissected from the anterior surface of the lumbar spine, being careful not to disturb the superior hypogastric plexus. We continue lateral dissection between the left and right iliac artery and vein, superior dissection ends at the aortic bifurcation. We thus obtain a triangular working space corresponding to the anterior surface of the intervertebral disc. Coagulation of the median sacral vessels is performed. An EndoRing orthostatic valve device is put in place by means of two pins in the L5 vertebral body and one pin in the S1 vertebral body (Fig. 23.1). The anterior longitudinal ligament is opened and discectomy is performed, permitting a release of the disc space and restoration of the intervertebral disc height. Subchondral bone is freshened up and, after trial implant, a definitive interbody fusion cage filled with spongeous autologous bone grafts is put in place. In a final step, the anterior Pyramid plate is applied through double screw fixation in S1 and single screw fixation in L5. Backing out of the screws is prevented
by a locking plate (Fig. 23.2). The plate is made of titanium; it is triangular with smooth angles and a posterior lip on the back of the plate. This shape fits well in the vessels’ bifurcation in the majority of cases as demonstrated with our angio MRI analysis in this series (Fig. 23.3).
by a locking plate (Fig. 23.2). The plate is made of titanium; it is triangular with smooth angles and a posterior lip on the back of the plate. This shape fits well in the vessels’ bifurcation in the majority of cases as demonstrated with our angio MRI analysis in this series (Fig. 23.3).
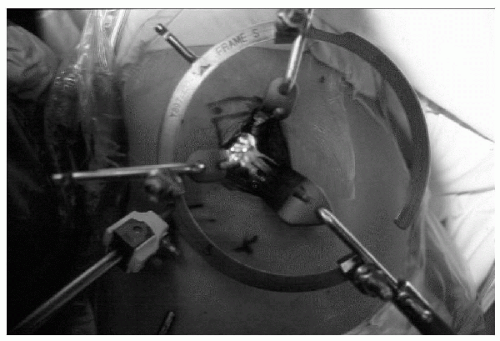 FIG. 23.1. Video-assisted L5-S1 retroperitoneal approach: Per operative view of the operating field. |
The average hospital stay is 5 days. In the postoperative period, no drainage is used. A soft lumbar brace is applied, and the patient can start ambulation the day after surgery. The soft brace is recommended for 6 weeks.
Statistics
Pre- and Postoperative Oswestry Disability Index scores were analyzed using the Student T-test.
RESULTS
Anterior lumbar interbody fusion with cage and anterior plate fixation was feasible in every patient.
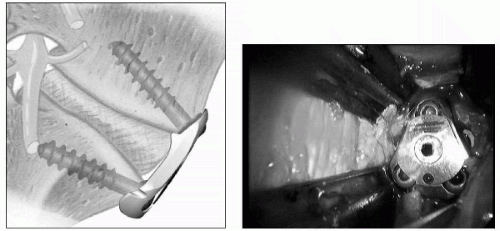 FIG. 23.2. Scheme of the plate on lateral view and per operative view of the plate with screw locking mechanism. |
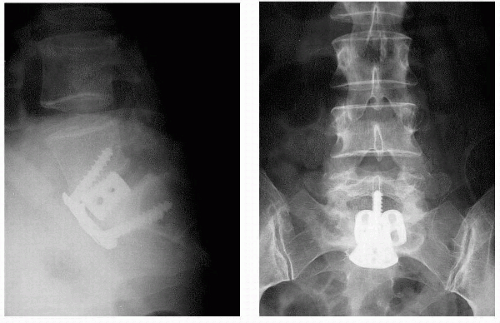 FIG. 23.3. Postoperative AP and lateral radiography of Grade 1 spondylolisthesis operated with anterior lordotic cages and pyramid plate. |
Complications
Vascular Complications. One vascular complication was noted. It involves a minor lateral injury to the left common iliac vein. The hole was clipped, and the procedure was continued without further problems. Deep venous thrombosis was not encountered.
No Retrograde Ejaculation. None of the nine male patients suffered from retroejaculation.
Donor Site Problems. One superficial wound infection that necessitated prolonged local aseptic dressings occurred. There were no lesions of the lateral femoral cutaneous nerve. However, a hypoesthesia in the region of the lateral cutaneous nerve was noted in six patients. After 1 year, there was a clear recuperation of sensibility in all patients but one.
Wound Problems. One case of superficial wound dehiscence occurred and was treated with local dressings. Abdominal wall herniation was not seen.
Clinical Results
Mean follow-up was 26.2 months (range 12 to 48 months). All patients but two, who sent us their questionnaires and radiographs by mail, were followed at the outpatient-clinic.
Oswestry Disability Index Score. Mean preoperative score was 57% (range 16% to 82%). With a mean ODI score of 30% at the 6-week follow-up consultation, there was a statistically significant improvement (p <0.0001). At the last follow-up visit, the mean ODI score was 21% (range 0 to 50%). This amelioration is also statistically significant in comparison with the 6-week follow-up scores (p <0.05).
Low Back Pain. Two patients suffered from invalidating chronic low back pain with ODI scores at the last visit comparable to their preoperative score (24% and 46%). The first case is a clear problem of adjacent level disease. The L4-L5 disc was degenerated before the surgery with a black disc without Modic change. This overweight patient has a clear sagittal imbalance with a high incidence angle, and this could be the reason for a higher constraint on the superior level. The second patient had undergone a posterior
arthrodesis earlier in his medical history, and he presented with a pseudarthrosis. (See discussion later in the chapter.)
arthrodesis earlier in his medical history, and he presented with a pseudarthrosis. (See discussion later in the chapter.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








