(1)
Cedars-Sinai Spine Center, Los Angeles, CA, USA
An anterior approach is optimal for many disease processes of the thoracic spine. These approaches have required a posterolateral thoracotomy to access the vertebral bodies or intervertebral disc spaces. This procedure carries with it the same known incisional morbidity of any intrathoracic procedure, making video-assisted thoracoscopic surgical techniques the clear choice in treating diseases of the thoracic spine. All patients sign a consent for video-assisted thoracoscopic surgery (VATS) of the spine with possible open thoracotomy and understand that such will be performed if VATS is unsuccessful.
All procedures should be performed under general endotracheal anesthesia with either a double lumen or Univent tube to allow for ipsilateral lung collapse and single lung ventilation. The patient is placed on a beanbag in the lateral decubitus position with the table maximally flexed to widen the intercostal spaces. The spine can be approached from either side, with the determining factor being the side to which the pathology presents. Because the spine is posterior, the patient should be rotated slightly anteriorly (20 to 30 degrees) to allow more anterior trocar placement. Placing the trocars too far posteriorly will make the visualization and work very difficult, especially when trying to identify the pedicles and the canal. A 30-degree-angle viewing scope should be used, and the surgeon and camera operator both stand on the ventral side of the patient. For proper orientation, the spine should be kept on the horizontal plane on the video monitor.
Trocar placement depends on the level of the spine to be approached, with the initial trocar inserted two levels above the affected disc space or vertebra at the anterior axillary line (Fig. 23.1). Ventilation to the ipsilateral lung is stopped to allow the lung to start collapsing before entering the pleural cavity. A 10-mm horizontal skin incision is then made at the chosen site, and a hemostat is used to spread the muscles and enter the pleural cavity by gently poking into it. A finger is then inserted through this incision to check for adhesions, which if found can be cleared with finger dissection to allow for a large enough space to insert a trocar. A 10-mm, 30-degree-angled scope is then inserted through this trocar and an initial exploratory thoracoscopy is performed. If adhesions are found, a second and third trocars are then inserted under vision to avoid lung injury. One should be two levels above and the other two levels below the original trocar and both slightly more anterior (Fig. 23.2). Through these working channels, the adhesions can be taken down using graspers, cautery, and the endoscissors. Any small pleural tears can be ignored at this time as they will seal spontaneously. Larger tears to the lung and pleura may need to be repaired using standard stapling techniques.
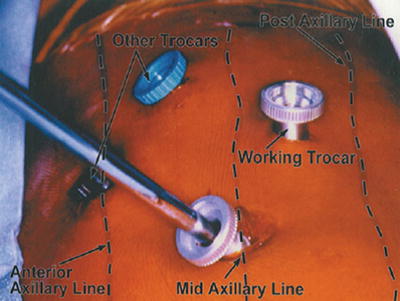
Fig. 23.1
Diagram for trocar positions at T5–T6 for pathology at T7–T8
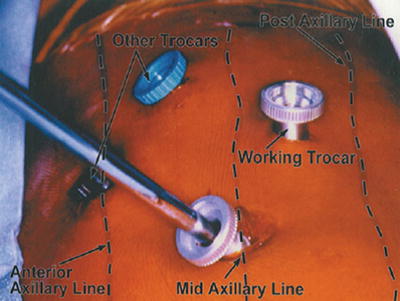
Fig. 23.2
Actual trocar positions
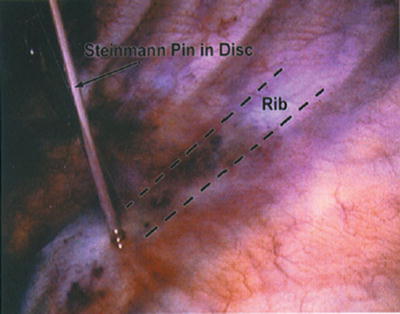
A fan retractor is then used to help finish collapsing the lung (by gently pushing on it) and to hold it anteriorly and visualize the spine through the parietal pleura. The target level is then tentatively identified by counting the ribs. The 1st rib is not visible through the parietal pleura, but it can be palpated with a blunt grasping instrument. The appropriate rib is followed and its base identified (Fig. 23.3). A long needle or pin is then inserted percutaneously into the pleural cavity and guided with a grasper into the disc space adjacent to the rib head (Fig. 23.4). Radiologic confirmation is then obtained.
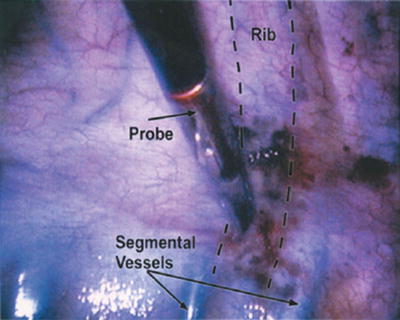
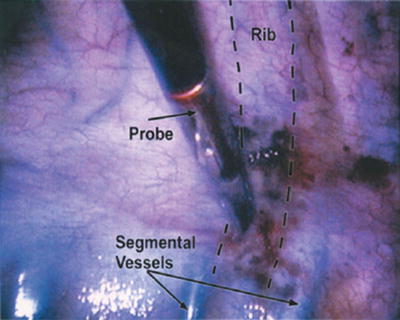
Fig. 23.3
Appropriate rib identified between segmental vessels