What is the Evidence Base for IDET?
Brian J. C. Freeman
In 2000 Saal and Saal (25) introduced a new method for the treatment of chronic discogenic low back pain using intradiscal electrothermal therapy (IDET). The technique involved placement of a 17-gauge introducer needle under fluoroscopic guidance into the center of the disc. A navigable intradiscal catheter with a temperature controlled thermal resistive heating coil was then deployed through the needle and positioned under two-plane fluoroscopy to a final position at the inner posterior annulus (Fig. 8.1).
The standard heating protocol raises the temperature of the catheter tip from 65° to 90°C over 12.5 minutes. The temperature is then maintained at 90°C for 4 minutes. According to Saal and Saal (23), this creates annular temperatures of 60° to 65°C. After heating, the catheter is removed and 10 mg of cephazolin is injected intradiscally. The authors propose the mechanism of action of IDET to be a combination of thermocoagulation of native nociceptors and ingrown unmyelinated nerve fibers plus annular collagen shrinkage stabilizing annular fissures (25). The postprocedural care allowed patients
o walk and perform low-intensity leg stretches for the first month, to resume stabilization floor exercises by the end of the second month, and to increase the intensity of exercise at the end of the third month.
o walk and perform low-intensity leg stretches for the first month, to resume stabilization floor exercises by the end of the second month, and to increase the intensity of exercise at the end of the third month.
Prospective Cohort Studies (Level of Evidence 2b) (22)
Early studies were promising, with 80% of patients reporting a reduction of at least two points on the visual analogue scale (VAS) for low back pain and 72% reported improvement in sitting tolerance and reduction in analgesic requirement (25). Improvements in physical function and bodily pain subsets of the Short Form-36 (SF-36) were also noted. Patients working prior to the procedure returned to work within 5 days of the procedure. The authors demonstrated statistically significant improvements in function as measured by VAS, sitting tolerance, and SF-36 following IDET.
Saal and Saal (26) subsequently reported the 1-year outcome of an expanded cohort of 62 patients undergoing IDET. Between November 1997 and October 1998, 62 from 1,116 patients treated by the authors did not improve adequately after a minimum of 6 months of conservative care. All 62 patients were offered long-term pain management, fusion surgery, or IDET. All 62 chose to undergo IDET. From 62 patients, 33 were men and 29 were women. The mean age was 41 (range 21–58). Thirty-nine patients were private payers and 23 were receiving workers’ compensation. The mean duration of preoperative symptoms was 60 months (range 10 months to 17 years). Twenty of 39 private-paying patients were working; none of the 23 workers’ compensation patients were working. Thirty patients were treated at one disc level and 32 patients at two or more disc levels.
The VAS improved a mean of 3.0 points for the whole group. For the single-level patients the mean improvement in VAS was 3.4 points, but for the multilevel patients the mean improvement was only 2.6 points. Twelve of 62 patients did not show any improvement in VAS. For the whole group, the physical function score of the SF-36 improved 20 points (23.6 points for the single-level group and 17 points for the multilevel group). For the bodily pain score of the SF-36, the mean improvement for the whole group was 17.4 points (16.8 points for the single level group and 18.0 points for the multilevel group). Six of 62 patients did not improve in either physical function or bodily pain subscales of the SF-36. Three of 62 patients underwent an epidural injection during the first 8 weeks following the procedure. Two of 62 patients underwent fusion surgery 1 year following the IDET procedure. Ninety-seven percent of private-paying patients and 83% of the workers’ compensation patients returned to work. The time to return to work varied between 14 days for those with sedentary jobs and 4 to 6 months for those with heavy jobs. There was no significant difference in clinical outcome between private-paying and workers’ compensation patients. For patients with decreased disc height (more than 30% loss of disc height) who had treatment at multiple levels, the outcome was less favorable than those with multilevel treatment who had preserved disc height.
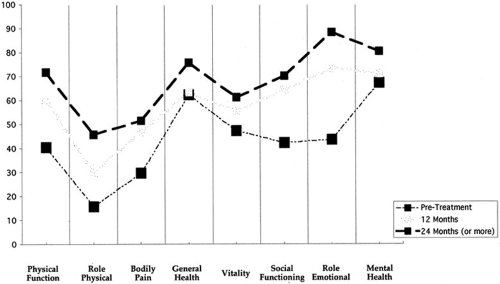
Saal and Saal (27) reported on the 24-month outcome in the same cohort. The mean VAS dropped from 6.57 to 3.41, an improvement of 3.16 points. The sitting time increased on average by 52.7 minutes. The mean physical function score of the SF-36 improved 31.33 points and the mean bodily pain score improved 21.87 points (Fig. 8.2). Eighty-one percent of patients showed at least a 7.0-point improvement in physical function and 78% improved at least 7.0-point improvement in bodily pain. Seventy-two
percent of patients improved their VAS by at least 2.0 points. Also striking was that the improvement continued over 2 years and seemed to be comparable in one-, two-, or three-level treated disease.
percent of patients improved their VAS by at least 2.0 points. Also striking was that the improvement continued over 2 years and seemed to be comparable in one-, two-, or three-level treated disease.
Derby et al. (9) reported 32 consecutive cases of IDET. All patients were initially assessed by an orthopaedic surgeon and told either they were not suitable for spine surgery or they were offered surgery and declined. Outcome measures included the Roland-Morris disability questionnaire, the VAS, a patient satisfaction index, and a questionnaire related to activities of daily living. The mean age of participants was 42 years, with only four workers’ compensation cases. Seven patients had previous surgery. Derby treated both discrete annular fissures and global disc degeneration. The mean improvement in VAS was 1.84 (SD 6 2.38). The mean improvement in Roland-Morris was 4.03 (SD ± 4.82). There was no significant change in outcome measures at 6 months and at 12 months. Overall, 62.5% had a favorable outcome, 25% had no change, and 12.5% had a nonfavorable outcome. One patient underwent a spine fusion due to persistent discogenic back pain.
Karasek and Bogduk (17) reported 12-month follow-up of a controlled trial of IDET for back pain due to internal disc disruption. From 110 patients undergoing computed tomography (CT) discography, 53 satisfied the criteria for internal disc disruption at one or two levels. Authority to undergo IDET was sought from the insurance carriers of these patients. Authority was granted in 36 and denied in 17. The 36 patients constituted the index treatment group and underwent IDET followed by rehabilitation. The 17 patients constituted a “convenience sample control group” and underwent rehabilitation. Outcome measures included the VAS, return to work, use of opioid analgesics, and Oswestry Disability Index (ODI) in some patients. The control group were followed for 3 months: the median VAS was 8 (range 5–8) before rehabilitation and 8 (range 7 to 8) at 3 months. The IDET group had a median VAS of 8 (range 7–9) before treatment reducing to 3 (range 1–7) at 12 months. Some patients returned to work and reduced their opioid intake. Bogduk and Karasek (4) subsequently reported on the 24-month follow-up in the IDET group. Fifty-four percent of patients reduced their pain by half, with
one in five patients achieving complete relief of pain. The authors concluded that IDET relieved discogenic pain, had a success rate of between 20% to 60%, and was superior to physical rehabilitation. The use of patients who had been denied treatment as a “control group” raises serious methodologic flaws in this paper.
one in five patients achieving complete relief of pain. The authors concluded that IDET relieved discogenic pain, had a success rate of between 20% to 60%, and was superior to physical rehabilitation. The use of patients who had been denied treatment as a “control group” raises serious methodologic flaws in this paper.
Gerszten et al.(15) studied 27 patients following IDET. Eight had private insurance and nine had received workers’ compensation. Sixteen patients underwent IDET at one level and 11 patients underwent IDET at two or more levels. The mean duration of symptoms was 38 months and the follow-up was 12 months. Outcome measures included quality of life as assessed by the SF-36 and disability as measured by the ODI. The physical function score of the SF-36 improved from a baseline of 32 to 47 points at final follow-up. The bodily pain score of the SF-36 improved from 27 to 38 at final follow-up. The ODI improved from 34 at baseline to 30 points at final follow-up. The authors noted that at 1 year 45% of patients reported a significant improvement on the SF-36 survey and that 75% of patients had improvement of their symptoms following IDET. Pain was not measured in this study. The authors found no relationship between outcome and the number of levels treated, the duration of symptoms, or workers’ compensation status.
Spruit and Jacobs (31) reported on pain and function after IDET for symptomatic lumbar disc degeneration in a cohort of 20 patients. The mean VAS improved by 1.4 points (p = 0.046), but the individual scores showed great variation. The ODI did not improve significantly. The SF-36 showed improvement, but only for the subscales vitality (p = 0.023) and bodily pain (p = 0.047). The authors concluded that IDET was not effective in reducing pain and improving functional performance.
Lutz et al. (19) treated 33 patients with chronic constant lumbar discogenic pain of more than 6 months with IDET. The mean age was 40 years and the mean duration of symptoms was 46 months. The mean follow-up period was 15 months. The mean VAS improved from 7.5 to 3.9 (p, 0.001) and a mean improvement in the Roland-Morris disability questionnaire of 7.3 points was noted (p 0.001). With regard to patient satisfaction, 75.7% reported that they would undergo the same procedure for the same outcome. Complete pain relief was achieved in 24% of the patients and partial pain relief in 46% of the patients.
A summary of the clinical outcome following IDET for these prospective cohort studies is presented in Table 8.1. From a total of 191 patients the mean improvement in VAS was 3.02 (range 1.48–5.0) at a mean of 15 months (range 12–28 months).
Retrospective Cohort Studies (Level of Evidence 3b) (22)
Freedman et al. (13) reported on his experience with IDET for the management of chronic discogenic low back pain in active-duty soldiers. Forty-one active-duty soldiers (34 men, 7 women) underwent IDET for chronic discogenic low back pain unresponsive to nonoperative therapy. During the study period, 36 of 41 patients underwent a single trial of IDET and the remaining 5 underwent two trials of IDET. Only the results of the first 36 patients were analyzed. All 36 patients had follow-up data at 6 months but only 31 patients had reached final follow-up (mean 29.7 months, range 24–46). Success was defined as a 50% decrease in pain from baseline. The success rate was 47% (17 out of 36) at 6 months and 16% (5 of 31 patients) at latest follow-up. Fifty-two percent of patients had a two-point or greater decrease in the VAS for pain.
Nineteen of 31 soldiers (61%) remained on active-duty at a minimum of 24 months after IDET. Seven of 31 soldiers (23%) went onto spinal surgery within 24 months of failed IDET. The authors conclude that IDET is not a substitute for spinal fusion in the treatment of chronic discogenic pain. They consider it at best an antecedent rather than an alternative to spinal fusion.
Nineteen of 31 soldiers (61%) remained on active-duty at a minimum of 24 months after IDET. Seven of 31 soldiers (23%) went onto spinal surgery within 24 months of failed IDET. The authors conclude that IDET is not a substitute for spinal fusion in the treatment of chronic discogenic pain. They consider it at best an antecedent rather than an alternative to spinal fusion.
TABLE 8.1 Summary of Clinical Outcome Following IDET: Prospective Cohort Studies (Level of Evidence 2b) | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree