Fig. 1
Axial computed tomography scans without contrast agent showing the dimension of a pterional flap (standard flap)
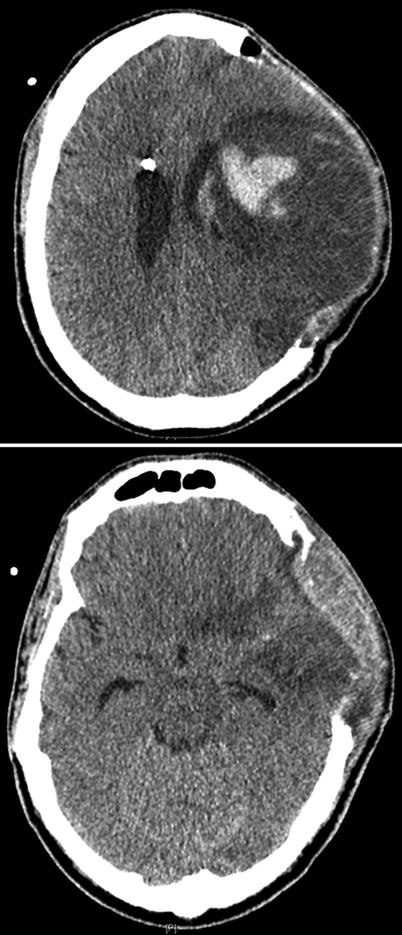
Fig. 2
Axial computed tomography scans without contrast agent showing the dimension of a large frontotemporoparietal flap (large flap)
One patient (16.7 %) presented with aphasia at admission, three patients (50 %) with focal neurologic deficits, and three patients (50 %) with cranial nerve palsy. In one case (16.7 %), a ventriculitis occurred, which was treated with intrathecal and i.v. antibiotics. Two of six patients showed a progression of neurologic deficits or postoperative complication, leading to a morbidity of 33 %. Mortality was 16.7 % (n = 1; case 2), caused by rebleeding of the aneurysm and vasospasm with hemispheric infarction.
All patients (n = 6) developed vasospasm and in all cases a hypertensive therapy was instaurated. In two cases (33 %), intraarterial transfemoral angioplasty and/or papaverine infusion was indicated. In two cases (33 %), delayed cerebral ischemia led to DIND, and, in three cases (50 %), a perfusion deficit was seen on CT with angiographic and perfusion sequences. In five cases (83 %), cerebral infarction was seen on radiologic examinations. One patient with a pterional bone flap (case 6) required additional surgical decompression because of diffuse brain swelling.
At discharge, the mean GCS was 8.8 (±4.4). The mean GCS of the standard flap group (9.75 ± 5.31) was better than in the large flap group (7 ± 0). Mini Mental Scores (MMS) were not assessable in two patients because of aphasia. Two patients had a MMS of 29 and two patients a MMS of 27 and 15. The mRS was 1 in three patients, and 3, 5, and 6 in one patient each (mean 4 ± 1.7). The Glasgow Outcome scale (GOS) was 3 in three patients and 1, 2, and 5 in the other three (mean 2.8 ± 1.3), while a Barthel Index (BI) of 100 was seen in two patients and a BI of 0 in three patients (mean 33.3 ± 51.6). Five patients (83.3 %) showed focal neurological deficits at discharge, four patients (66.7 %) showed cranial nerve palsy, and one patient (16.7 %) had aphasia.
In one case (case 3), bone flap reimplantation was not concluded because the patient deceased because of rebleeding and diffuse brain swelling. Three patients recovered to a sufficient clinical state to justify bone flap reimplantation after 2–7 months, and, in two cases, reimplantation was carried out earlier, after 3–4 weeks, because of hydrocephalus needing ventriculoperitoneal shunt placement. No complications or new neurologic deficits occurred after bone flap reimplantation.
At follow-up (n = 5, range 4–18 months, mean 6.5 months), four patients showed a GCS of 15, while one patient had a GCS of 10 (mean 14 ± 2.2). The mRS was in three patients 1, 3, and 5 in one patient each (mean 2.2 ± 1.8). The GOS was 5 in three patients, and 2 and 3 in one patient each (mean 4 ± 1.4), and a BI of 100 was seen in two patients and a BI of 50, 30, and 5 in one patient each (mean 57 ± 42.4). MMS was not assessable in two patients because of aphasia. Two patients had a MMS of 27 and one patient a MMS of 29 (mean 16.6 ± 15.8). All patients displayed improvement of neurologic deficits at follow up compared with discharge. Tables 1 and 2 summarize the patient characteristics and results.
Table 1
Results of decompressive hemicraniectomy group vs. pterional flap group
Pterional flap (n = 4) | Decompressive flap (n = 2) | |
|---|---|---|
Admission GCS | 13.75 (±1.26) | 8.5 (±0.7) |
Admission mRS | 1.75 (±1.5) | 4.5 (±0.7) |
Discharge GCS | 9.75 (±5.31) | 7.0 (±0) |
Discharge mRS | 3.75 (±2.06) | 4.5 (±0.7) |
Midline shift | 1.25 (±2.5) | 14.25 (±17.86) |
Hematoma volume | 14.50 (±3.56) | 79.20 (±22.91) |
Table 2
Patient characteristics
Characteristics | Radiology | Operation | |||||
|---|---|---|---|---|---|---|---|
Patient no. | Gender | Location | Fisher grade | MLS | Hematoma volume (cm3) | Age (years) | Flap |
1 | m | MCA | 3 | 17 | 95.4 | 46 | Large |
2 | f | MCA | 4 | 12 | 63 | 61 | Large |
3 | f | A-com | 4 | 0 | None | 25 | Standard |
4 | f | A-com | 4 | 0 | None | 53 | Standard |
5 | m | A-com | 3 | 0 | 37 | 48 | Standard |
6 | f | MCA | 4 | 5 | 20 | 50 | Standard |
Admission | Discharge | Follow-up | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Patient no. | H&H grade | WFNS grade | GCS | Neurologic deficits | GCS
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||||||||||


