X STOP Interspinous Implant for Lumbar Spinal Decompression
Jim F. Zucherman
Patrick Simons
Jake Timothy
Neurogenic intermittent claudication (NIC) secondary to lumbar spinal stenosis (LSS) is a posture-dependent complaint and it typically affects patients at the age of 50 years or older. NIC is defined as pain or numbness in the buttocks, thighs, and/or lower legs caused by decrease of the spinal canal area and brought on by either prolonged standing or exercise in the erect posture. The symptom is typically relieved by various maneuvers that flex the lumbar spine, which increases the spinal canal area significantly(1,2,3,4,5,6,7,8,9).
Decompressive surgery with or without fusion is the current gold standard treatment for moderate to severe symptomatic LSS.
Interspinous Process Decompression (IPD)
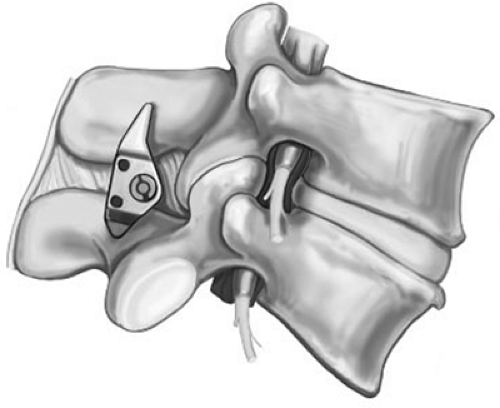
A new minimally invasive, stand-alone alternative to conservative and standard surgical decompressive treatments has been developed (10,11,12,13). The interspinous implant (X STOP, St. Francis Medical Technologies Inc., Alameda CA) is placed between the spinous processes to prevent extension of the symptomatic levels, yet allowing flexion, axial rotation, and lateral bending (Fig. 23.1)(14). Eliminating the symptomatic extension at the abnormal segment and keeping it in that position would maintain the asymptomatic state and allow the more normal spinal segments to function normally. The patient would no longer be forced to keep the entire lumbar spine in flexion just to maintain enough space at the localized stenotic areas.
Because the load-bearing element is anterior to the retained supraspinous ligament a cantilever effect results, unloading the middle column of the spine while restoring height loss from degenerative changes. This is born out by biomechanical testing mentioned later. Also the retained posterior supraspinous ligament prevents kyphotic deformity as is verified by the radiographic studies mentioned later. The load that is taken up by the device is taken from the middle column of the spine, which has deteriorated from its inability to efficiently handle loads over the years. This then may allow slowing of the degenerative process or even some recovery of inflamed chronically overloaded tissues over time as is evidenced by the persistence of benefit from the device with a 78% success rate at 4-year follow-up based on
Oswestry Disability Index (ODI) scores (15). Because sagittal balance effect is minimal, motion limitation is minimal, and adjacent disc and facet joint pressures are unaffected, there is no reason to believe the device will adversely affect the natural history of adjacent segments.
Oswestry Disability Index (ODI) scores (15). Because sagittal balance effect is minimal, motion limitation is minimal, and adjacent disc and facet joint pressures are unaffected, there is no reason to believe the device will adversely affect the natural history of adjacent segments.
Biomechanical studies have shown that, in extension, the implant significantly increases the canal area by 18%, the subarticular diameter by 50%, the canal diameter by 10%, the foraminal area by 25%, and the foraminal width by 41%. These dimensions were not affected at adjacent levels. This is the primary mechanism of action (16). Wardlaw et al. reported equal results in their clinical study evaluating positional magnetic resonance imaging (MRI) changes after X STOP implantation (17,18). Further studies have also demonstrated that, at the implanted level, the implant significantly reduces the pressure on the facets, in the nucleus pulposus, and in the posterior annulus of the disc, without influence on adjacent levels (16,19,20).
Surgical Procedure
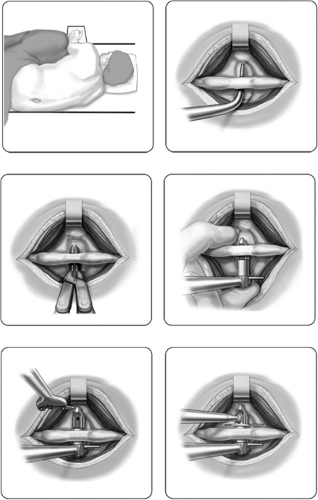
Patients may be operated on under local anesthesia with light intravenous sedation, placed in either lateral decubitus or prone position. A 4- to 8-cm midline incision is made exposing the spinous processes at the appropriate disc level, which is confirmed radiographically. The supraspinous ligament and its attachments are preserved, which is of paramount importance to prevent postoperative kyphosis and also to serve to stabilize the implant. The interspinous ligament is pierced, but retained, and the implant is placed between the spinous processes. The spinous processes are not modified to allow implantation, but in cases where hypertrophied facets protrude posteriorly, they should be trimmed without interfering its integrity in function (Fig. 23.2). The spinal canal is not violated, and neither laminotomy, nor laminectomy, nor foraminotomy is performed. Removal of any portion of the ligamentum flavum is unnecessary.
Clinical Results in Literature
X STOP Prospective Randomized Multicenter Study
Based on very promising results of a clinical pilot study of ten symptomatic LSS patients treated with the X STOP, a United States Food and Drug Administration (US FDA) prospective randomized clinical multicenter study was undertaken, comparing the interspinous implant with conservative (nonoperative) treatment for the management of NIC. Study results demonstrated a clinically and statistically significant difference favoring the interspinous implant. Two years after the surgery, 60% of the patients reported that their symptoms were significantly improved, compared to 18% of the control patients. Regarding physical function, 57% of X STOP patients reported significant improvement, compared to 15% of control patients. Among X STOP patients, 73% were satisfied or very satisfied with their treatment compared to 36% of the control group patients (Table 23.1)(21).
Of interest, 39 patients with grade I degenerative spondylolisthesis were treated in the U.S. study with the X STOP and 22 patients were treated nonoperatively. Using 15-point improvement over baseline scores in the Zurich Claudication Questionnaire
(ZCQ) as the criterion of clinical success, 69% of the X STOP patients had a successful outcome at 2-year follow-up, compared to 9% of the control patients. The mean improvement score for the 39 X STOP patients was 26 points. There were no significant differences in the mean percentage of slip between X STOP and control patients at baseline or at 2-year follow-up. The X STOP represents a significantly less invasive alternative therapy for these patients, resulting in very good clinical outcomes, and most importantly, no evidence that the implant results in any instability of the motion segment. In this study, more than a third of the patients treated with the X STOP implant suffered from a degenerative spondylolisthesis up to grade 1 (out of 4). Spondylolisthesis patients are mostly treated with an instrumented spinal fusion. Analysis of this subgroup showed that the X STOP procedure is as effective as that applied on patients without spondylolisthesis (22).
(ZCQ) as the criterion of clinical success, 69% of the X STOP patients had a successful outcome at 2-year follow-up, compared to 9% of the control patients. The mean improvement score for the 39 X STOP patients was 26 points. There were no significant differences in the mean percentage of slip between X STOP and control patients at baseline or at 2-year follow-up. The X STOP represents a significantly less invasive alternative therapy for these patients, resulting in very good clinical outcomes, and most importantly, no evidence that the implant results in any instability of the motion segment. In this study, more than a third of the patients treated with the X STOP implant suffered from a degenerative spondylolisthesis up to grade 1 (out of 4). Spondylolisthesis patients are mostly treated with an instrumented spinal fusion. Analysis of this subgroup showed that the X STOP procedure is as effective as that applied on patients without spondylolisthesis (22).
TABLE 23.1 Zurich Claudication Questionnaire (ZCQ) Success Rates 2 Years After Surgery | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
Furthermore, Implicito et al. (23) reported on their subanalysis of the X STOP patients in this study, comparing 63 one-level and 33 double-level IPD patients. With the current surgical options, NIC patients treated surgically at multiple levels typically have worse outcomes than those treated at one level. This study showed that both X STOP groups had significant improvements postoperatively (p <0.0001). The success rate of the one-level IPD patients was 56% and for the two-level IPD patients it was 73%, with no significant difference between the success rates, showing the X STOP to be an effective way to surgically treat patients with NIC at more than one level.
Sagittal Balance
The requirement to maintain proper sagittal alignment and balance in patients receiving spinal implants is well understood. Experience with lumbar fusion procedures that cause a flat back has overwhelmingly resulted in unacceptable clinical outcomes. Three different radiologic studies were therefore undertaken to measure any possible effect of the X STOP on sagittal alignment. In the U.S. study, x-rays were taken at each follow-up visit for both X STOP and control patients and measurements were made of the lumbosacral angle (L1 to S1) and the treated intervertebral angle. At 2-year follow-up, there were no significant differences in the mean scores between the two groups of patients. Preoperative x-rays from a subset of X STOP patients were also compared to standing films taken at 2-year follow-up. In 23 patients with single-level implants, the change in the intervertebral angle was only 0.5 degree (±2.0 degrees), and the change in the
lumbosacral angle was 0.1 degree (±3.8 degrees). Similar values were recorded for 18 patients with double-level implants.
lumbosacral angle was 0.1 degree (±3.8 degrees). Similar values were recorded for 18 patients with double-level implants.
Interim data from an ongoing study being conducted at the University of Aberdeen by Wardlaw and Smith (24) have recently been presented, in which preoperative images were compared to postimplant images obtained in a positional MRI scanner. In addition to confirming in vivo the increases in the area of the foramen and canal that were measured in the preclinical in vitro cadaver study, results of this study confirm a change in angulation for both the lumbosacral angle and intervertebral angle of between 1 and 2 degrees. These three studies confirm that the X STOP results in only minimal changes to sagittal alignment. This due is to preserving the supraspinous ligament and its original insertions. This ligament is a very robust structure receiving the confluence of the lumbodorsal fascia and its preservation prevents overdistraction of the segment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree