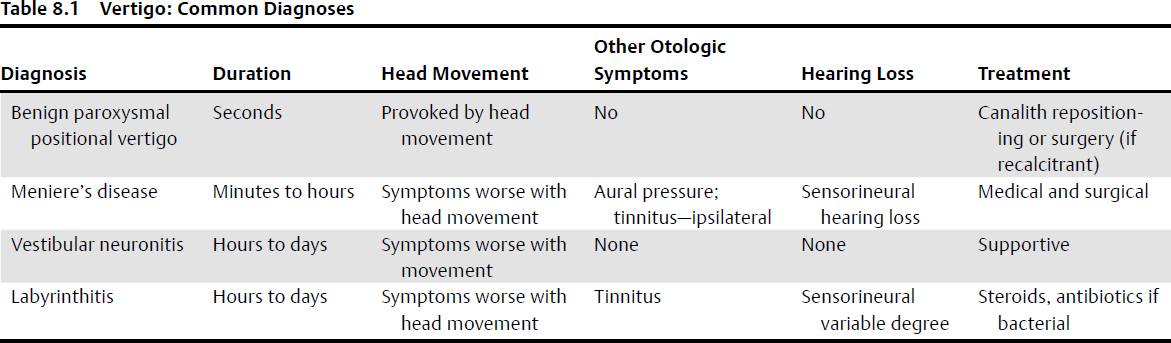
8 Otorhinolaryngology and Principles of Neurotology in Skull Base Surgery Neurotology is the study of the neurology associated with the ear, including hearing and balance function. Diagnostic Pearl A detailed history in a patient complaining of hearing and balance symptoms is the most valuable diagnostic information. • Common symptoms associated with skull base pathology such as hearing loss, tinnitus, imbalance, dysphagia, and nasal obstruction/epistaxis often prompt referral to otorhinolaryngology for assessment. A detailed history should address the presenting complaint as well as related symptoms such as hearing loss, tinnitus, aural pressure, imbalance, vertigo (hallucination of circling movement), diplopia, vision loss, altered facial sensation or weakness and nasal symptoms. • Lateral skull base • Local anatomy examination (including endoscopy) • Eye movements The Halmagyi head thrust is a test for unilateral peripheral vestibular weakness. The patient is asked to look at a target straight ahead, usually the nose of the examiner, while the examiner turns the patient’s head rapidly to the side. Normal: The patient’s gaze stays fixed on the target. Abnormal: A corrective saccadic eye movement occurs toward the target at the end of the head thrust, indicative of a peripheral vestibular weakness on the side that the head was moved toward. • Cerebellar testing • Gait • Special tests The Rinne test is useful to diagnose a conductive hearing loss and should be done along with the Weber test. A tuning fork is held firmly on the mastoid bone (bone conduction hearing) until patients report they can no longer hear the sound. Then the tuning fork is held adjacent to the external ear canal (air conduction). Patient are then asked if they can hear the tuning fork. Normal: a positive test. The patient can hear the tuning fork held beside ear canal (air conduction is greater than bone conduction). Abnormal: a negative test. The patient reports that the sound is not audible adjacent to the ear canal (bone conduction is greater than air conduction), which indicates a conductive hearing loss. A tuning fork is held on the vertex of the head or on the midline of the forehead, and the patient identifies where the sound is loudest: central (equal in both ears) or lateralized to one side. Normal: the sound is equal in both ears, or central. Abnormal: the sound is louder or “lateralizes” to one ear. In unilateral conductive hearing loss, sound is louder in, or lateralizes to, the ipsilateral ear. In unilateral sensorineural hearing loss, sound is louder in, or lateralizes to, the contralateral ear. Position testing is done with the patient in the sitting position, with the head turned 45 degrees to one side, and then rapid movement onto supine position and head hanging (neck in extension and supported by the examiner). The eyes are observed for nystagmus. Rotational geotropic nystagmus (toward the ground) is the classic diagnostic finding in benign positional vertigo. The test is repeated on the other side and with the head in the center position. Audiometric testing includes pure tone audiometry (PTA), which is standardized to assess the threshold of hearing between 250 and 8,000 Hz using a pure tone (sinusoidal) test frequencies. Normal threshold hearing levels are between 0 and 20 dB. Air conduction testing evaluates the entire hearing system, whereas bone conduction testing stimulates the cochlea, thereby bypassing the conduction mechanism. Both air and bone conduction hearing is tested using different headsets; air conduction headset is either an ear canal insert or a standard headset and the bone conduction headset is held against the mastoid bone. Comparison of the air and bone conduction threshold levels is useful to diagnose the etiology of hearing loss. • Conductive hearing loss: Air conduction threshold levels are elevated with normal bone conduction testing. • Air–bone gap: There is a difference in threshold levels between air and bone conduction. • Sensorineural hearing loss: Both the air and bone conduction thresholds levels are elevated (abnormal) to the same degree. • Mixed loss: Bone conduction thresholds are abnormal and air conduction levels are elevated relative to the bone levels. • Speech tests: each ear tested separately. The speech reception threshold (SRT) is the sound level (in dB) at which a patient can detect the presence of speech 50% of the time. • The percentage of words correctly repeated by a patient that were presented at a comfortable hearing level with a headset. • Relevant test to evaluate surgical approach options that put hearing at risk and for rehabilitation (e.g., hearing aid). If the speech discrimination score is markedly abnormal, then a hearing aid would not be useful. Pearl Unilateral reduction in hearing, especially in speech discrimination or distortion of language perception, is a classic finding of central pathology. Impedance testing is done with a probe inserted into the ear canal, which generates a sound pressure level tone high enough to assess middle ear pressure, and the mobility/integrity of the tympanic membrane as well as the ossicular chain. The peak of the tympanogram shows the pressure of the middle ear space, which has a normal range. The most common abnormality found in impedance testing is related to underlying eustachian tube (ET) dysfunction. Chronic ET dysfunction can cause middle ear fluid (serous otitis media [SOM]) and lead to chronic otitis media with or without a tympanic membrane perforation. Most ET disorders are developmental (common in children) or due to an inflammatory process (viral upper respiratory tract infection being the most common). However, tumors of the skull base can also cause similar symptoms (hearing loss, ear pressure, tinnitus) due to either direct tumor extension or secondary ET obstruction. Abnormal: A negative middle each pressure or middle ear fluid is often found when the ET is not ventilating the middle ear adequately. The stapedial reflex is a bilateral protective mechanism mediated via CN VII that stimulates the stapedial muscle/tendon to tense, thereby stabilizing the stapes from excessive movement under loud sound conditions. The test records changes in tympanic membrane compliance with sound exposure. • Normal: bilateral responses at 70- to 100-dB hearing level • The reflex is absent if there is a conductive hearing loss in the test ear. • Acoustic reflex decay: Assess if the stapedius muscle can sustain contraction in response to a test sound at 10 dB above the acoustic reflex threshold for 10 seconds. Abnormal: the response decreases to half or less within 5 seconds (usually tested at 500 and 1,000 Hz). Retrocochlear (central) pathology is an abnormal reflex decay or absent stapedial reflex without evidence of conductive hearing loss (ipsilateral ear). Auditory brainstem response (ABR, also termed brainstem auditory evoked potential [BAEP]) is an auditory evoked electrical potential of the auditory system. The ABR is measured using surface electrodes and a headset or in the ear canal insert probe presenting repeated tone or click stimuli. This test can be used to objectively determine auditory thresholds, diagnose auditory pathway pathology, and as an intraoperative monitoring tool. This is an objective test that does not require patient participation and is not affected by anesthesia or central nervous system suppressants. A normal ABR is recorded 8 to 10 ms after a transient sound (click or tone), which generates five to seven electrical peaks or waves within 10 ms that represent an afferent auditory system response from the cochlear nerve through to the midbrain. Prior to performing an ABR, a PTA is done to determine appropriate ABR test parameters. Abnormal: sensorineural hearing loss most often in retrocochlear pathology with reduced, delayed, or absent peak potentials. The ABR/BAEP waveform is generated by: • I and II: cochlea and extra-intracranial component of the auditory nerve (the average distance from the ear to the brainstem is 2.6 cm; this distance is traversed by the impulse in ~1 ms) • III: cochlear nucleus • IV: superior olivary complex • V: lateral lemniscus Waves I, III, and V are most consistent, but the wave peaks associated with VI and VII are inconsistent, and they are maybe generated by inferior colliculus neurons.2–5 The ABR/BAEP should also be performed preoperatively for baseline evaluation. Auditory evoked potential monitoring intraoperatively is most often done by ABR/BAEP, electrocochleography (ECochG) and/or compound action potential or CAP. Pearls • The ABR is affected by body temperature, traction, and ischemia. However, preservation of the ABR waveform is highly predictive of hearing preservation postsurgery.6,7 • Rapid loss of the ABR may be due to ischemic injury of the cochlear nerve.7 • Auditory waves give rise to a complex waveform that does not provide real-time feedback to the surgeon, as is the case in with facial nerve monitoring.7,8 The compound action potential or CAP can be recorded either using a probe on the promontory or by direct auditory nerve monitoring at the internal auditory canal. The CAP is the depolarization of the distal end of the auditory/cochlear nerve, stimulated by means of a click via an earphone as in an ABR,4 and registered by means of a wick electrode made from a Teflon-insulated silver wire. The CAP appears as a large (25–30 μV) triphasic response that can be reduced by surgical manipulation of the nerve. The main limitation of the technique is that the exposure of the nerve is often possible only at the end of the tumor resection, when the nerve may already be dysfunctional. Moreover, cerebrospinal fluid (CSF) may create impedance changes at the electrode–nerve interface.7 The ECochG consists of the electrical response to stimuli (i.e. clicks or tone bursts) from the cochlea and the distal auditory/cochlear nerve. The ECochG includes the cochlear microphonic (generated from the hair cells in the cochlea), the cochlear summating potential (also generated from within the cochlea) and the compound action potential. Near-field technique entails placing an electrode on the promontory of the inner ear through the tympanic membrane, or a ball-tip electrode on the round window membrane via a tympanomeatal flap or facial recess approach.7,8 The generated potentials originate from the organ of Corti within the cochlea. A latency shift in the recording is generally associated with neural hearing loss,9 and it can be useful for intraoperative monitoring. Surgical Anatomy Pearl Comparing ABR, recorded with a subdermal needle electrode at the mastoid, with ECochG, recorded by a ball electrode attached to the tympanic membrane or on the promontory, it has been shown that ECochG is more reliable in terms of clinical outcome, and it may replace ABR recording in CPA surgery.10 • The first wave of the ABR corresponds to the action potential of the cochlear/auditory nerve in response to the sound stimulus. The possible elicited responses include the cochlear microphonic, the summating potential (SP), and the whole nerve action potential (AP) depending on the type of sound stimulus presented. ECochG is primarily used to diagnose Meniere’s disease (endolymphatic hydrops) with an abnormal ratio of the SP and AP.11 The outer hair cells of the cochlea are able to amplify movement of the cochlear membranous partition of the labyrinth, which results in extremely low intensity acoustic emissions measurable in the ear canal. These otoacoustic emissions (OAEs) are classified as spontaneous (without any sound stimulus) or as evoked (in response to specific test sounds). OAEs are detectable in normal hearing and are reduced or absent in hearing loss of > 35 dB. The test uses an ear canal probe with a speaker and microphone and has become a standard of care to screen for hearing loss in newborn infants. Outer hair cells (and therefore OAEs) are particular sensitive to ototoxicity, hypoxia, and noise exposure. Hearing loss is described according to the etiology as conductive, sensorineural, or mixed (both). • Conductive hearing loss: common causes • Sensorineural hearing loss: common causes Management depends on the etiology, but workup will involve a complete physical examination, otoscopy (with microscope if there is an external/middle ear abnormality), and an audiogram including pure tone audiogram and speech discrimination testing. Surgical Anatomy Pearls • Most hearing loss and tinnitus symptoms are bilateral unless related to otitis media or trauma (identifiable from the history). • Unilateral sensorineural hearing loss, particularly loss of speech discrimination, is suspicious for central/skull base pathology until proven otherwise. This syndrome is a varicella zoster infection that most commonly presents with a painful herpetic skin rash in the ear canal, pinna, or tympanic membrane, with associated hearing loss and facial nerve weakness. Vertigo can also occur. Ototoxicity includes both hearing and balance toxicity due to an adverse effect of medical therapy. The most commonly implicated medications include aminoglycosides and platinum based chemotherapy. • Risk factors: age (elderly), renal failure, loop diuretics, duration of medication, elevated serum levels of aminoglycosides Vertigo is the hallucination of circling movement often accompanied by nausea, vomiting, sweating, and ataxia. • The history and physical examination are the most important tools in making an accurate diagnosis. Specifics should include the onset, frequency, and duration of vertigo, as well as aggravating and relieving factors. Other otologic (e.g., hearing loss, tinnitus, aural pressure, ear discharge) and nonotologic (e.g., headache, nausea, facial weakness, double vision, voice or swallowing changes) symptoms are relevant and should be a standard part of the history. The underlying diagnosis can be categorized by the duration and frequency of the vertiginous episodes and are summarized in Table 8.1. Benign paroxysmal positional vertigo (BPPV) is by far the most common diagnosis in a patient with vertigo. BPPV is characterized by vertigo lasting seconds (less than a minute) often provoked by a rapid head movement, particularly neck extension or rotational head motion. It is thought that displaced otoliths floating inside the membranous labyrinth are the underlying pathology, causing position-induced asymmetric movements of the inner ear fluid. BPPV is more common with a history of previous ear infection, head injury, or Meniere’s disease. Meniere’s disease classically presents with episodic vertigo lasting minutes to hours, with accompanying tinnitus, sensorineural hearing loss, and, less commonly, aural pressure or fullness. Although episodic in nature with some hearing recovery between episodes, most patients will eventually have a permanent sensorineural hearing loss (moderate to severe) with natural disease progression. Ablative treatment using gentamicin instillation into the middle ear has been shown to successfully stop the vertiginous episodes by vestibular ablation due to the ototoxic characteristics of gentamycin. This is not without risk of permanent sensorineural hearing loss. The etiology of vestibular neuronitis is unclear, and requires a clinical diagnosis of exclusion, with acute vertigo lasting hours to days without other otologic symptoms. Possible causes include viral, inflammatory, and vascular. Labyrinthitis is inflammation of the inner ear, including the cochlea and vestibular organs. Possible causes are viral, bacterial, and autoimmune disorders. The common CPA tumor typically presents with a progressive gradual unilateral hearing loss (found in 85% of patients) and tinnitus (66%).12 Imbalance symptoms rather than vertigo are more commonly reported and are present in 35 to 50% of patients.12 If a sudden sensorineural hearing loss is the presenting complaint, about 1% of patients are found to have a vestibular schwannoma.13,14 With increasing tumor size, signs and symptoms progress to include fifth nerve hypoesthesia and loss of corneal reflex. Large tumors can affect the lower cranial nerves, causing voice and swallowing dysfunction. With brainstem compression, hydrocephalus will result in headache and vision changes. Facial weakness is infrequent, and visual changes can be from lack of eye closure, hydrocephalus (blurring), or papilledema. Nystagmus, fast phase toward the ipsilateral side, is commonly present in larger tumors, and cerebellar signs may also occur. • Differential Diagnosis Vertigo (Common Causes) Balance function testing is useful to assist in the diagnosis of many vestibular disorders, helping to distinguish between peripheral and central pathology and to quantify the degree of vestibular dysfunction. Vestibular and ocular motor systems are evaluated in the standard test battery. The electronystagmogram (ENG) is based on the vestibular ocular reflex (VOR) and associated eye movements. • Standard ENG (widely available) records the changes in eye position using surface electrodes to measure electrical potential between the cornea (+) and retina (–). • Rotational head movement is normally accompanied by equal and opposite eye movements to maintain a stable retinal image mediated by the VOR. • The test results are measured either as a surface electrical response output or using a video ENG system to record eye movements using a goggle camera and near-infrared light tracking system. Nystagmus is the main eye movement tracked and is described by direction and velocity (degree/s) from the slow phase of the eye movement. Saccadic eye movements are quick movements used to track an object or move the target image to the fovea of the retina. Calibration of an ENG is done by asking patients to move their gaze between two test lights 10 degrees off center. The accuracy and symmetry of the eye movement is recorded. The smooth pursuit system stabilizes images of moving objects on the fovea and is assessed by the subject tracking a moving light or pendulum. The lateral (horizontal) semicircular canal is stimulated by flushing the test ear canal with warm or cool water (7°C above and below normal body temperature) for 30 to 60 seconds. The temperature change stimulates internal fluid flow in the lateral (horizontal) semicircular canal. Surface electrodes record the corneoretinal electrical potential as the eyes move. Nystagmus is the normal physiological response using the mnemonic COWS (see Pearl) to indicate the appropriate direction of the fast phase of the nystagmus. Fixation suppression (patient is asked to look at a target) should occur during the caloric testing. Pearl User the mnemonic COWS: Cold—Opposite; Warm—Same. • The velocity of the slow phase of the nystagmus is calculated and compared with that of the opposite ear. Less than a 20% difference is a normal, and 20% or greater represents a right- or left-sided weakness. • Test cannot be performed with water if a tympanic membrane perforation is present. • Results consistent with a peripheral disorder: • Findings suggestive of a central disorder15: The vestibular evoked myogenic potential (VEMP) is an evoked electromyographic response test of the ipsilateral sternocleidomastoid muscle to a loud click stimulus presented to the ipsilateral ear. The VEMP test is used to assess the inferior vestibular nerve (afferent) and the spinocerebellar tract (efferent). This test is not yet routinely available. The facial nerve is complex (see Chapter 3, page 83). It has motor, sensory, and general and specialized efferent/afferent nerve fibers for functional anatomy. Acute facial paralysis (arising over hours or days) is a disabling condition, and most patients will seek emergency treatment. The most common cause of facial paralysis is Bell’s palsy (> 50% of cases) followed by trauma (20% of cases). Neoplastic disease account for 5% of facial paralysis. The history should address the facial weakness symptoms, the rate of onset, the duration, and the following associated symptoms: • Otologic (ear pain, otorrhea or ear discharge, hearing loss, tinnitus, aural pressure, vertigo, or imbalance) • Facial numbness (CN V) • Hyperacusis (discomfort with loud noise exposure due to stapedial branch dysfunction) • Dry eyes (reduced tearing) • Past ear disorders or surgery Pearl Gradual onset (> 3 weeks) of facial weakness, multiple cranial nerve palsies, neck or facial mass, are suggestive of neoplastic etiology.
 History
History
Symptoms
 Diplopia, dizziness (imbalance), vertigo, hearing loss, unilateral tinnitus, aural fullness
Diplopia, dizziness (imbalance), vertigo, hearing loss, unilateral tinnitus, aural fullness
 Cranial nerve deficits causing dysphonia, dysphagia, dysarthria, facial weakness, and altered sensation to face
Cranial nerve deficits causing dysphonia, dysphagia, dysarthria, facial weakness, and altered sensation to face
 Shoulder weakness
Shoulder weakness
 Headache, otalgia
Headache, otalgia
 Midline lesions
Midline lesions
 Anosmia, epistaxis, nasal obstruction, unilateral hearing loss (conductive), headache, facial/sinus pain
Anosmia, epistaxis, nasal obstruction, unilateral hearing loss (conductive), headache, facial/sinus pain
 Hitselberger sign: decreased sensation in the external auditory canal from the sensory auricular branch of cranial nerve [CN] VII), often found in cerebellopontine angle (CPA) tumors.
Hitselberger sign: decreased sensation in the external auditory canal from the sensory auricular branch of cranial nerve [CN] VII), often found in cerebellopontine angle (CPA) tumors.
 Cranial nerve testing
Cranial nerve testing
 Facial weakness
Facial weakness
 Facial numbness or reduced sensation, loss of corneal reflex
Facial numbness or reduced sensation, loss of corneal reflex
 Palate symmetry with movement, gag reflex
Palate symmetry with movement, gag reflex
 Shoulder movement, strength, and head rotation
Shoulder movement, strength, and head rotation
 Tongue movement
Tongue movement
 Oral cavity inspection, palpation
Oral cavity inspection, palpation
 Nasal examination including upper airway endoscopy (also examine vocal fold movement and constrictor muscle movement)
Nasal examination including upper airway endoscopy (also examine vocal fold movement and constrictor muscle movement)
 Abnormal eye movements (asymmetric movement, saccadic pursuit)
Abnormal eye movements (asymmetric movement, saccadic pursuit)
 Nystagmus: Vertical nystagmus represents central pathology, horizontal nystagmus may be peripheral or central pathology.
Nystagmus: Vertical nystagmus represents central pathology, horizontal nystagmus may be peripheral or central pathology.
 Careful observation of eye movements with four-direction lateral gaze as well as smooth pursuit testing
Careful observation of eye movements with four-direction lateral gaze as well as smooth pursuit testing
 Horizontal nystagmus: etiology can be peripheral or central pathology
Horizontal nystagmus: etiology can be peripheral or central pathology
 Vertical nystagmus: etiology is central
Vertical nystagmus: etiology is central
 Testing
Testing
Halmagyi Head Thrust Test1
Interpretation
 Dysmetria, dysdiadochokinesis
Dysmetria, dysdiadochokinesis
 Romberg test
Romberg test
 Finger nose, assess for tremor
Finger nose, assess for tremor
 Alternative rapid movements, hand, foot
Alternative rapid movements, hand, foot
 Spontaneous gait
Spontaneous gait
 Tandem gait, eyes open/closed (normal: 10 steps without side stepping in patients < age 70)
Tandem gait, eyes open/closed (normal: 10 steps without side stepping in patients < age 70)
 Tuning fork tests are very useful bedside tests for rapidly distinguishing between conductive and sensorineural hearing loss.
Tuning fork tests are very useful bedside tests for rapidly distinguishing between conductive and sensorineural hearing loss.
 A 512-Hz tuning fork is most useful, and both Rinne and Weber tests should be done for accurate diagnostic information.
A 512-Hz tuning fork is most useful, and both Rinne and Weber tests should be done for accurate diagnostic information.
Rinne Test
Interpretation
Weber Test
Interpretation
Dix Hallpike Position Test
Audiometric Testing
Speech Reception Threshold
Speech Discrimination Testing
Impedance Testing
Interpretation
Stapedial Reflex
Interpretation
Retrocochlear (Central) Pathology
Audiometric Brainstem Response
Interpretation
Intraoperative Auditory Monitoring
Compound Action Potential
Electrocochleography (ECochG)
Otoacoustic Emissions
 Hearing Loss
Hearing Loss
 Acute otitis media (serous otitis media or purulent)
Acute otitis media (serous otitis media or purulent)
 Chronic otitis media
Chronic otitis media
 Otitis externa
Otitis externa
 Obstruction in canal (wax, debris, foreign body)
Obstruction in canal (wax, debris, foreign body)
 Tympanic membrane (TM) perforation
Tympanic membrane (TM) perforation
 Otosclerosis (stapes fixation with abnormal bone growth at stapes foot-plate)
Otosclerosis (stapes fixation with abnormal bone growth at stapes foot-plate)
 Trauma (temporal bone fracture, ossicular discontinuity, TM perforation)
Trauma (temporal bone fracture, ossicular discontinuity, TM perforation)
 Neoplasm in external canal, middle ear
Neoplasm in external canal, middle ear
 Presbycusis (aging)
Presbycusis (aging)
 Congenital/familial
Congenital/familial
 Ototoxicity (e.g., aminoglycoside exposure, loop diuretics, nonsteroidal anti-inflammatory drugs)
Ototoxicity (e.g., aminoglycoside exposure, loop diuretics, nonsteroidal anti-inflammatory drugs)
 Noise induced
Noise induced
 Trauma (temporal bone fracture involving otic capsule)
Trauma (temporal bone fracture involving otic capsule)
 Infectious (viral, bacterial [e.g., meningitis, herpes zoster oticus, syphilis])
Infectious (viral, bacterial [e.g., meningitis, herpes zoster oticus, syphilis])
 Autoimmune (rare [e.g., Wegener’s granulomatosis, Cogan’s syndrome])
Autoimmune (rare [e.g., Wegener’s granulomatosis, Cogan’s syndrome])
 Syndromes
Syndromes
Ramsay Hunt Syndrome (Herpes Zoster Oticus)
Ototoxicity
Vertigo
Benign Paroxysmal Positional Vertigo
Meniere’s Disease (Endolymphatic Hydrops)
Vestibular Neuronitis
Labyrinthitis
Acoustic/Vestibular Schwannoma
 Vertebral-basilar insufficiency
Vertebral-basilar insufficiency
 Presyncope (often associated with hypertension treatment)
Presyncope (often associated with hypertension treatment)
 Medication adverse effects
Medication adverse effects
 Migraine
Migraine
 Hyperventilation
Hyperventilation
Vestibular Diagnostic Tests
Electronystagmogram (ENG)
Optokinetic Testing
Pursuit
Bithermal Caloric Tests
 Unilateral caloric weakness (no other pathology on test)
Unilateral caloric weakness (no other pathology on test)
 Positional nystagmus
Positional nystagmus
 Direction fixed nystagmus
Direction fixed nystagmus
 Bilateral or absent caloric weakness with history of labyrinthine disorder or ototoxicity
Bilateral or absent caloric weakness with history of labyrinthine disorder or ototoxicity
 Vertical nystagmus
Vertical nystagmus
 Direction-changing nystagmus
Direction-changing nystagmus
 Failure of fixation suppression during caloric testing
Failure of fixation suppression during caloric testing
 Abnormal saccadic or pursuit testing
Abnormal saccadic or pursuit testing
Vestibular Evoked Myogenic Potentials
 Facial Nerve
Facial Nerve
Assessment of Facial Paralysis
History
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree