CHAPTER 27 Drug Addiction
OVERVIEW
During the last decade, the number of patients treated for substance abuse–related problems in the United States has grown steadily. Between 1997 and 2002, the number of emergency department (ED) visits for drug-related events increased by more than 24%.1 In 2004, 1.3 million ED visits involved drug misuse or abuse.2 The National Survey on Drug Use and Health (NSDUH) findings in 2004 showed that 19.1 million Americans, or 7.9% of the population age 12 and older, used an illicit drug in the past month.3 Clinical presentations are also becoming more complex. More than 55% of the drug-related problems seen in EDs in the first half of 2002 involved the use of multiple drugs. In 37% of these cases, drug dependence was identified as the primary problem; 20% of the cases involved individuals seeking drug-induced psychic effects and 20% involved suicide attempts. Among individuals who abuse drugs, 53% have a second co-occurring psychiatric disorder. Successful treatment of this expanding group of patients requires that clinicians improve their skills in the management of patients with substance use disorders and co-occurring psychiatric disorders. Although physicians may feel comfortable treating the symptoms of substance abuse, they are often reluctant to deal with the core disease process, and little effort is made to refer patients for substance abuse treatment. The chronic, relapsing nature of substance abuse is inappropriately thought to imply that substance abuse treatment is not helpful. This leads clinicians to ignore multiple opportunities to intervene in the disease process. Most clinicians fail to appreciate that the relapse rate in other common chronic medical disorders (such as diabetes, hypertension, and asthma) exceeds that for the substance abuse disorders, and, hence, they do not handle substance abuse patients with comparable therapeutic diligence.4 Problems related to substance abuse should always be addressed with the same degree of compassion and persistence that is directed to other common relapsing medical disorders.
THE NEUROBIOLOGY OF ADDICTION
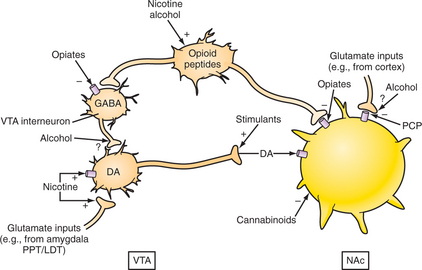
Disruption of the endogenous reward systems in the brain is a common feature of all of the major drugs of abuse; most of these drugs act by disrupting dopamine circuits in the brain. Acute changes increase synaptic dopamine and disrupt circuits that mediate motivation and drive, conditioned learning, and inhibitory controls (Figure 27-1). This enhancement of synaptic dopamine is particularly rewarding for individuals with abnormally low density of the D2dopamine receptor (D2DR). Normal individuals (with normal levels of the D2DR) find this experience too intense and aversive and thus may be shielded from the risk of addiction. Low D2DR availability is associated with an increased risk for abuse of cocaine, heroin, methamphetamine, alcohol, and methylphenidate. Chronic drug use produces long-lasting and significant decreases in dopamine brain function, manifested by decreases in both the D2DR and dopamine cell activity. These decreases are also associated with dysfunction in the prefrontal cortex, including the orbitofrontal cortex (which is involved in salience attribution) and the cingulated gyrus (which is involved in inhibitory control and mood regulation).5 Low baseline levels of beta-plasma endorphins are associated with a higher endorphin response to alcohol and an increased risk for alcohol dependence; it is less clear whether this abnormality also increases the risk for opiate dependence. Table 27-1 lists the major drugs of abuse and the associated disruption of CNS neurotransmitter systems.
Table 27-1 Neurobiology of Drug Reinforcement
| Drug Type | Mechanism of Reinforcement |
|---|---|
| Cocaine Amphetamines Nicotine | Mesolimbic dopamine system |
| Opioids | Mesolimbic dopamine system |
| Alcohol | GABA and glutamate Dopamine and serotonin Opioid peptide systems |
| Cannabinoids | Dopamine in the nucleus accumbens |
GABA, γ-aminobutyric acid.
COCAINE
Abuse
After alcohol, cocaine is the leading drug of abuse in terms of frequency of ED contacts, general hospital admissions, family violence, and other social problems.6 The Drug Abuse Warning Network (DAWN) estimates that out of 940,953 illicit drug-related ED visits in 2004, cocaine was involved in nearly 40% of them.2 Even mature individuals with normal psychological profiles are vulnerable to compulsive cocaine use. Acute users experience intense euphoria often associated with increased sexual desire and with improved sexual function. These acute rewards are often followed by a moderate-to-severe post–cocaine use depression that provides a strong compulsion for further cocaine use. These responses are primarily mediated by disruptions of synaptic dopamine. The initial cocaine response is stimulated by elevated dopamine generated by blockade of the dopamine reuptake transporter (DAT) and the inhibition of the reuptake of synaptic dopamine. Chronic cocaine use leads to down-regulation of dopamine receptors and ultimately depletion of synaptic dopamine, which is thought to be the cause of post–cocaine use depression (Figures 27-1 and 27-3). Like other stimulants, cocaine also disrupts the synthesis and reuptake of serotonin. Other receptors affected include norepinephrine, N-methyl-d-aspartate (NMDA), γ-aminobutyric acid (GABA), and opioid receptors. Plasma cholinesterases rapidly convert cocaine into benzoylecognine (BE), an inactive metabolite that can be detected in the urine for 3 days. When alcohol is taken in conjunction with cocaine, liver esterases produce cocaethylene, an active metabolite that is longer lasting (2- to 4-hour half-life) and more cardiotoxic than is cocaine. The combination of cocaine and marijuana also produces more intense euphoria, higher plasma levels, and more cardiotoxicity than does cocaine alone.
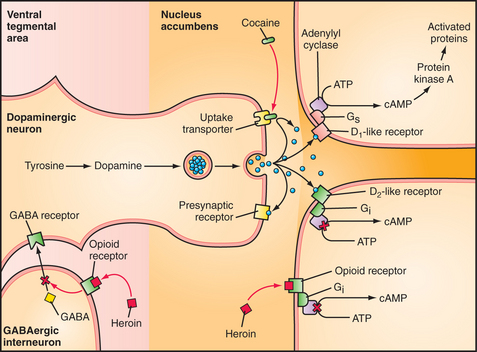
Figure 27-3 Schematic of the effects of cocaine and heroin in the synapse.
(Redrawn and adapted from Leshner A and the US National Institute on Drug Abuse: New understandings of drug addiction, Hospital Practice Special Report, April 1997, McGraw-Hill.)
The signs and the symptoms of acute cocaine intoxication are similar to those of amphetamine abuse. Typical complaints associated with intoxication include anorexia, insomnia, anxiety, hyperactivity, and rapid speech and thought processes (“speeding”). Signs of adrenergic hyperactivity (such as hyperreflexia, tachycardia, diaphoresis, and dilated pupils responsive to light) may also be seen. More severe symptoms (such as hyperpyrexia, hypertension, and cocaine-induced vasospastic events [e.g., stroke or myocardial infarction]) are relatively rare among users, but are fairly common in those seen in hospital EDs. Patients may also manifest stereotyped movements of the mouth, face, or extremities. Snorting may produce rhinitis or sinusitis and, rarely, perforations of the nasal septum. Free-basing (inhalation of cocaine alkaloid vapors) may produce bronchitis. Grand mal seizures are another infrequent complication. Patients also describe “snowlights” (i.e., flashes of light usually seen at the periphery of the visual field). Crack is a highly addictive free-base form of cocaine that is sold in crystals and can be smoked.
Management
Chronic cocaine use produces tolerance, severe psychological dependency, and physiological dependence (marked by irritability, anhedonia, low mood, insomnia or hypersomnia, and anxiety).7 Dependent users typically follow a cyclical pattern of 2 or 3 days of heavy binge use, followed by a withdrawal “crash.” Use is resumed again in 3 to 4 days, depending on the availability of cash and the drug. A gradual reduction in use of the drug is almost never possible. Detoxification is accomplished by the abrupt cessation of all cocaine use, usually through restricted access (e.g., a loss of funds or contacts, or incarceration). Withdrawal symptoms begin to resolve within 7 days; the value of medication treatment for withdrawal symptoms has yet to be confirmed. Drugs that enhance central nervous system (CNS) catecholamine function may reduce craving, although they are of limited clinical benefit and they have not been proven effective in double-blind placebo-controlled trials. There is some indication that amantadine (an indirect dopamine agonist) and propranolol may help individuals with severe withdrawal symptoms. The major complication of withdrawal is a severe depression with suicidal ideation. If this occurs, the patient requires psychiatric hospitalization. The need for inpatient care may be brief, since suicidal ideation usually clears promptly with the cessation of cocaine use. A less severe anhedonic state may persist for 2 to 3 months and is thought to reflect a more persistent state of dopamine depletion.
Once compulsive cocaine use has begun, it is almost impossible for the user to return to a pattern of occasional, controlled use. Such individuals are also likely to develop problems with alcohol and other drugs. For that reason, the goal of treatment should be abstinence from cocaine and all other drugs. All cocaine abusers should be referred for individual or group counseling, and participation in 12-step self-help programs should be strongly recommended. Manual-guided cognitive-behavioral therapy (CBT) has been efficacious in the treatment of cocaine dependence.8 Twelve-step facilitation and CBT appear to be helpful, particularly in individuals with more severe dependence and in those with co-morbid disorders.9 Family members or significant others should be referred separately to Al-Anon because they will gain insights that may help them eliminate systemic support for the patient’s drug use. There is no Food and Drug Administration (FDA)–approved pharmacotherapy for cocaine dependence. Trials with desipramine, fluoxetine, bupropion, amantadine, and carbamazepine have had inconsistent results. Positive responses have been reported in trials with topiramate, baclofen, and modafinil, but these drugs require further investigation. Several trials with disulfiram have shown benefit, with reduced craving and use, and a reported increase in the aversive effects of cocaine should the patient relapse. These reactions are thought to be mediated by the inhibitory effect of disulfiram on dopamine beta-hydroxylase. This action will elevate depleted plasma dopamine levels in chronic users and will produce abnormally high dopamine levels if cocaine is ingested; this results in a dysphoric experience for most users.
AMPHETAMINES
Abuse
Stricter federal controls on the production and distribution of amphetamines have greatly reduced the number of amphetamine abusers. Nonetheless, stimulants (including amphetamine and methamphetamine) were involved in 10% of all illicit drug–related ED visits in 2004.2 Illicitly produced methamphetamine has fueled a major abuse epidemic on the West Coast and in much of the Midwest.
A more serious problem involves the patient who develops a severe psychological dependence on amphetamines or methamphetamine and who may have the same symptoms seen in younger street-drug abusers. Amphetamine and methamphetamine (speed) accounted for a total of 16,215 ED visits in the first half of 2002.1 The signs and symptoms of acute amphetamine intoxication are similar to those of cocaine abuse. Long-term effects also include depression, brain dysfunction, and weight loss. The other classic syndrome seen in either acute or chronic amphetamine intoxication is a paranoid psychosis without delirium. Although typically seen in young people who use IV methamphetamine hydrochloride, it can also occur in chronic users of dextroamphetamine or other amphetamines. A paranoid psychosis may also occur with or without other manifestations of amphetamine intoxication. The absence of disorientation distinguishes this condition from most other toxic psychoses. This syndrome is clinically indistinguishable from an acute schizophrenic episode of the paranoid type, and the correct diagnosis is often made in retrospect, based on a history of amphetamine use and with a urine test that is positive for amphetamines. Use of haloperidol or low-dose atypical antipsychotics is often effective in the acute management of this type of substance-induced psychosis.
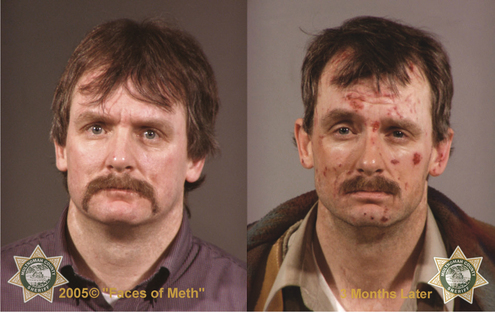
Other distinctive features of chronic stimulant abuse include dental problems (e.g., caries, missing teeth, and bleeding and infected gums), muscle cramps (related to dehydration and low levels of magnesium and potassium), constipation (due to dehydration), nasal perforations, and excoriated skin lesions (speed bumps) (see Figure 27-2). The urine may have a stale smell due to ammonia constituents used in the illicit manufacture of methamphetamine.
Treatment
Most signs of intoxication clear in 2 to 4 days. The major problem is appropriate psychiatric management of post–amphetamine use depression. In mild cases, this depression is manifest by feelings of lethargy, as well as by the subsequent temptation to use amphetamines again for energy. In more serious cases, the patient may become suicidal and require inpatient psychiatric treatment. The efficacy of antidepressants in such cases has not been adequately documented.Even with support and psychotherapy, most patients experience symptoms of depression for 3 to 6 months following the cessation of chronic amphetamine abuse. CBT has been helpful, but it may need to be adapted to allow for the cognitive impairment associated with long-term methamphetamine use.
CLUB DRUGS
During the 1990s there was a steady increase in the abuse of “club drugs,” primarily 3,4-methylenedioxy-methamphetamine (MDMA, or “Ecstasy”), γ-hydroxybutyrate (GHB), and ketamine. This trend was reversed between 1998 and 2001 when the Monitoring the Future Survey reported a steep decline in the use of Ecstasy. The drop has been attributed to a general recognition of the dangers associated with the use of this drug. The NSDUH reported that the number of current users of Ecstasy for individuals age 12 and older remained the same in 2003 and 2004.3 MDMA has both amphetamine-like and hallucinogenic effects. Its primary mechanism of action is via indirect serotonin agonism, but it also affects dopamine and other neurotransmitter systems. These drugs increase synaptic dopamine and alter serotonergic neurotransmission. MDMA was initially used experimentally to facilitate psychotherapy, but its use was banned after it was found to be neurotoxic in animals. The intense feelings of empathy experienced by users may be a result of the flooding of the serotonin system. In toxic amounts, it produces distorted perceptions, confusion, hypertension, hyperactivity, and potentially fatal hyperthermia. With chronic use, serotonin stores are depleted and subsequent doses produce a less robust high and more unpleasant side effects (such as teeth gnashing and restlessness). Frequent users learn to anticipate these effects and tend to limit their long-term consumption of the drug.
The treatment for overdoses of all of these drugs is primarily symptomatic.
NARCOTICS
While abuse of all major drug classes increased during the 1990s, the most dramatic increase was seen among new abusers of prescription pain relievers. In 2004, of all illicit drug–related ED visits, the DAWN survey estimates that 17% involved heroin.2 However, the 2004 NSDUH estimated that 31.8 million Americans used pain relievers nonmedically during their lifetime, up from 29.6 million in 20029; 4.4 million persons age 12 and older used opiates nonmedically in 2004.3 Lifetime nonmedical use of OxyContin increased from 1.9 to 3.1 million persons between 2002 and 2004.10 In 2004, among those age 12 and older, 2.4 million initiated nonmedical use of prescription pain relievers.10 This pattern of use has reached epidemic proportions on the East Coast, and OxyContin has replaced heroin as the entry point for opiate addiction. According to the 2005 Monitoring the Future Survey, the annual prevalence of OxyContin use among twelfth-graders was 5.5%, representing a 40% increase since 2002.11 Among nonmedical use of prescription drugs, opioid analgesics (including oxycodone and combination forms) were the most frequent drugs reported in the DAWN survey, present in 32% of the ED visits.2 Nearly one-third (31%) of acquired immunodeficiency syndrome (AIDS) cases in the United States are related to a history of injection drug use.12 As a result, the treatment of opiate dependence is becoming commonplace on medical and surgical floors of general hospitals. Proper management of such patients necessitates knowledge of FDA regulations and community treatment resources, and competence in the management of detoxification and opiate substitution therapy.
All opiates act by binding to the mu opioid receptor. Binding to receptors in the ventral tegmental area stimulates the release of dopamine (Figure 27-3), which activates brain reward centers in the nucleus accumbens (Figure 27-4). Opiates produce a wide range of effects (including analgesia, euphoria, sedation, decreased secretions, nausea, vomiting, constipation, miosis, urinary hesitation, and hypotension [Table 27-2]). The classic signs of opiate withdrawal are easily recognized and usually begin 8 to 12 hours after the last dose (of a short-lasting agent) (Table 27-3). The patient generally admits the need for drugs and shows sweating, yawning, lacrimation, tremor, rhinorrhea, marked irritability, dilated pupils, piloerection (“gooseflesh”), and an increased respiratory rate. More severe signs of withdrawal occur 24 to 36 hours after the last dose and include tachycardia, hypertension, insomnia, nausea, vomiting, and abdominal cramps. Untreated, the syndrome subsides in 3 to 7 days. Withdrawal symptoms are similar in patients addicted to methadone, but they may not appear until 24 to 36 hours after the last dose (because of methadone’s longer half-life) and abate over 2 to 4 weeks. Patients addicted to oxycodone may present a particularly severe and prolonged withdrawal syndrome and may require high doses of opiates for adequate control.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree