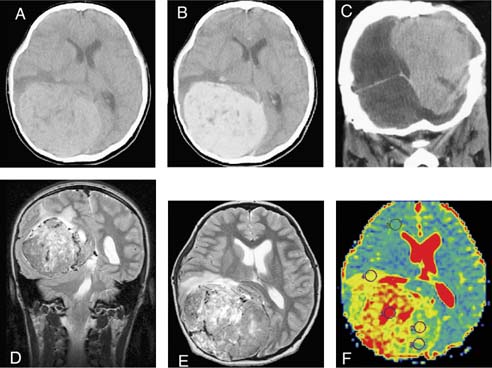
52 Diagnosis Giant meningeal hemangiopericytoma Problems and Tactics Meningeal hemangiopericytomas are rare malignant neoplasms arising from perivascular pericytes. Because hemangiopericytomas have a tendency to disseminate and locally recur, they have to be removed with follow-up irradiation 60 gr1–3. These tumors can be intensively vascularized, and their removal may present a serious problem, as illustrated by this case. Keywords Meningeal hemangiopericytoma, tumor embolization, blood-saving technique A 16-year-old girl was admitted to the Moscow Burdenko Neurosurgery Institute. For 7 years she had suffered from headaches, which became severe in the 3 months prior to her admission. The examination revealed signs of intracranial hypertension, edema, and partial atrophy of the optic nerves, decreased visual acuity in the right eye (0.6), left-side hemianopsia, instability, and gate ataxia. Computed tomography (CT) revealed a giant tumor of the right temporal parietooccipital region (96 × 80 × 94 mm). The tumor was hyperdense with multiple small hypodense regions and actively enhanced after contrast administration. There were marked parietal bone deformation and erosion above the tumor. Magnetic resonance imaging (MRI) (T2-regime) visualized a large number of pathological vessels and a large amount of microcysts. Ventricles were compressed and displaced by the tumor. The tumor penetrated into the tentorium and displaced the cerebellum hemisphere and the fourth ventricle. On diffusion-weighted images the tumor had a hypointensive signal in comparison with a gray matter signal. The apparent diffusion coefficient (ADC) map (Fig. 52–1F) showed high ADC values from the solid part of the tumor.1 H-spectroscopy revealed increased N-acetyl aspartate (NAA), decreased creatine (CR), increased Chodin (Cho), and myo-inositol (mI) peaks. The lactate (Lac) peak was also found. This type of spectra and ADC values may correspond to atypical meningioma. Selective angiography showed rich vascularization of the tumor, which was fed from the right posterior cerebral artery, both occipital arteries, the right middle meningeal, medial posterior auricular, and ascending pharyngeal arteries. In addition, the tumor was supplied by branches of the right internal carotid artery: meningo-hypophyseal trunk and middle cerebral artery. The right sinus trans-versus was not visualized. The aforementioned investigations suggested a meningeal hemangiopericytoma of a supra- and subtemporal localization. FIGURE 52–1 Axial computed tomography before surgery (A) without and (B) with contrast medium. (C) Coronal view shows bone erosion by the tumor. (D) Coronal and (E) axial T2-weighted magnetic resonance imaging scans revealing a huge mass with neoplastic vessels. (F) Apparent diffusion coefficient (ADC) map shows the higher level of diffusion in the tumor compared with brain tissue. To diminish tumor vascularization a tumor vessels embolization with polyvinyl alcohol (PVA) particles (500–1000 m m in diameter) was performed through the right occipital, middle meningeal, and left occipital arteries with a marked angiographic effect (Fig. 52–2). Five days later the patient was taken to the operating theater for tumor removal; however, during subclavian vein catheterization with a Swan-Ganz introducer (8.5F), a mediastinal hemorrhage occurred, and surgery was postponed for 3 weeks. Control angiography revealed revascularization of the tumor. Additional embolization of the feeding vessels was fulfilled: the right occipital artery was embolized by PVA microparticles and the middle meningeal artery by enbucrilat (HistoacrilR).
Surgical Removal of a Giant Meningeal Hemangiopericytoma
Clinical Presentation
Surgical Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree